Abstract
Purpose
This study investigated whether etoricoxib (COX-II blocker) has a superior efficacy of preventing heterotopic ossification (HO) after total hip arthroplasty (THA) compared to diclofenac (non-selective NSAID).
Methods
One hundred patients were included (50 in each group) in this single centre, prospective, double-blinded, randomized, controlled trial. Etoricoxib (90 mg) was administered once and diclofenac (75 mg) twice per day for a perioperative period of nine days. The incidence of HO was evaluated on radiographs of the pelvis six months after surgery.
Results
Eighty nine of 100 (89 %) patients could be analysed. The overall HO incidence was 37.8 %. There was no significant difference between both study groups. Twelve patients (27.3 %) of the DIC group and 13 patients (28.9 %) of the ETO group showed Brooker grade I ossifications. Five patients (11.4 %) of the DIC and four patients of the ETO (8.9 %) group showed grade II HO formations. No class III or IV HO formations occured in both groups. Ad hoc analysis detected a negative correlation between HO incidence and limited abduction and internal rotation of the hip.
Conclusions
Etoricoxib and diclofenac are equally effective for oral HO prophylaxis after primary cementless THA when given for nine peri-operative days to ensure a full recovery and high patient satisfaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heterotopic ossification (HO) is a complication after total hip arthroplasty (THA), arthroscopy of the hip or trauma of the musculo-skeletal system (i.e. distal humerus and acetabular fractures, cerebral or spinal cord injuries) [1–4]. The origin of HO and exact pathogenesis are yet unknown. The incidence of HO after THA can lie between 0.6-90 %, but is mostly reported to be 30-40 % after primary THA [5–7]; 15 % of all HOs could become symptomatic by causing pain and limited range of motion of the affected joint [8, 9]. The satisfaction rate of patients with severe HO after THA can decrease to only 30 % compared to 90 % satisfaction among patients without HO [10]. An oral prophylaxis by using NSAIDs (non-steroidal anti-inflammatory drugs) and prophylactic low dose irradiation seem to be the most effective therapy [6, 11, 12].
Non-selective NSAIDs like indomethacin, ibuprofen and diclofenac can cause serious side-effects, i.e. gastric ulcers, GI-bleeding etc. Selective COX-II blockers have a lower rate of GI-complications and seem to be a reasonable alternative for oral prophylaxis if considering the contraindications (i.e. cardiac conditions) [7, 13]. Rofecoxib (Vioxx®) and celecoxib (Celebrex®) were found effective for HO prophylaxis [14, 15]. The efficacy of etoricoxib (Arcoxia®) for HO prophylaxis has remained unclear.
This study aimed to compare the efficacy of diclofenac (non-selective NSAID) and etoricoxib (selective COX-II blocker) in preventing heterotopic ossification after primary THA. The hypothesis was that etoricoxib has a superior efficacy in preventing HOs compared to diclofenac.
Material and methods
Objectives
The findings described in this article are a sub-analysis of a secondary endpoint (incidence of HO 6 months after THA) of the ETO-DIC study. The primary endpoint was the total blood loss in both groups. Further secondary endpoints were gastrointestinal tolerability and analgesic efficacy. These data were published separately with a detailed description of methods and safety analysis [16].
Patients and pharmaceuticals
One hundred patients with primary or secondary osteoarthritis (Kellgren ≥ 3) were included, 50 patients in each group: etoricoxib (ETO) and diclofenac (DIC). Criteria for ex- and inclusion and contraindications are shown in Table 1. Diclofenac-sodium (Novartis, Germany) and etoricoxib (MSD Sharp& Dohme, Germany) were coated in identically looking pills, systematically packed and sequentially numbered by the University pharmacy in Dresden, Germany. Randomization was performed at the Institute for Medical Statistics and Epidemiology, Technische Universität Munich, Germany.
Study design
The study (single-centre, prospective, randomized and double-blinded phase IIIb superiority trial) was conducted between May 4th 2011 (first patient in) and January 31st 2014 (last patient out) in the orthopaedic surgery department at the Regensburg University Medical Centre, where 600 primary and 100 revision THAs are implanted each year. The Münchner Studienzentrum (Munich, Germany) supervised and supported this study. Participants gave their written consent prior to study inclusion and received one of 100 sequentially numbered sets of containers. This allowed a double-blinded and random allocation to each study group. All study members had a wash-out phase of at least five days, in which NSAIDS, COX-II blockers, aspirine, acetaminophen and metamizole were prohibited, prior to study inclusion. Only tilidine and tramadol were allowed. Table 2 shows the drug application plan.
In case of persistent pain, all patients received additional opioids. Patients were instructed to contact study investigators immediately in case of discomfort or emergency. Sealed envelopes for a premature unblinding of each patient were stored in a pre-defined room in the orthopaedic surgery department. Adverse events (AE) and serious adverse (SAE) events were noticed during study conduct and appropriate countermeasures were initiated.
After the trial period of nine days, the patients underwent a physical examination and were discharged to rehabilitation. Only acetaminophen and opioids were allowed for analgesia until follow-up. Six months after surgery patients were re-examined and a conventional radiography of the pelvis (anterior-posterior and axial) was taken in our department of radiology. The radiographs were evaluated by a senior orthopaedic surgeon (SW). If present, heterotopic ossifications were graded according to the Brooker classification [17]:
-
Grade 1
small islands of bone in the soft tissue/muscle around the hip.
-
Grade 2
bone formation in pelvis or proximal end of femur with a distance of > 1 cm between both surfaces.
-
Grade 3
bone formation in pelvis or proximal end of femur with a distance of < 1 cm between opposing surfaces.
-
Grade 4
ankylosis of the hip.
The study personal (investigators, patients, monitors, study nurse) remained blinded until the database was locked.
Ethics
This study was designed and conducted according to ICH harmonized tripartite guideline for Good Clinical Practice (including European Directive 2001/83/EC) and the Declaration of Helsinki on biomedical research involving human subjects. This trial was registered at EudraCT (nr. 2009-015383-33) and at clinicaltrials.gov (nr. NCT01229774) prior to study enrolment. Institutional ethical review board (IRB; Ethikkommission der Universität Regensburg) (nr. 10-111-0135) and German Federal Institute for Drugs and Medical Devices (BfArM) approvals were obtained.
Surgery and anaesthesia
Surgery was performed in a supine position by five senior orthopaedic surgeons, each having an operative experience of more than 200 THAs. A cementless THA (Corail® and Pinnacle®; DePuy®) was implanted by using a lateral approach (Bauer’s approach). An antibiotic single shot prophylaxis (cephazolin 2 g i.v.) was administered 20 minutes prior to surgery. Intra-operative blood salvage techniques were applied in every patient (Electa, Sorin Group, USA) and a re-transfusion was performed if indicated. Two patients had general anaesthesia, 97 patients had spinal anaesthesia (carbostesin 0.5 % 3.5-4.5 ml and 0.1 mg morphine). Patients were given intravenous infusions (crystalloids) and vital parameters (temperature, pulse, blood pressure) were obtained before and during surgery. All patients were monitored overnight on an intermediate care unit after surgery. Oral food and fluid intake were allowed a few hours after surgery. All patients received antithrombotic prophylaxis (certoparin sodium, Mono-Embolex® 3000 I.E. s.c.) once per day for five to six weeks after surgery until full-weight bearing was permitted.
Statistics
Statistics were planned and performed by the Institute for Medical Statistics and Epidemiology at the Technische Universität in Munich, Germany. A sample size calculation (two-sided independent samples t-test) was performed and a total of 100 patients (50 patients per group) were considered to be enough to find a statistical difference in the primary endpoint of the study (blood loss) with statistical power of 90 % and level of significance (α) of 5 %.
This article analyses the incidence of HO six months after THA in both groups (a secondary endpoint). It was tested on the ITT population, which consisted of all patients randomized in the study who received study medication and a primary THA with a Bauer’s approach. All statistics presented in this paper are with exploratory p-values. All analyses were performed on the ITT set. Missing values were not imputed. All tests were two-sided with significance level of 5 % (unadjusted for multiple comparisons). Descriptive statistics included mean and standard deviation (SD) and/or median with range for continuous variables and actual and relative frequencies or incidence rates for categorical variables. The HO incidences were compared using the Mann–Whitney-U test. Correlations between a) ossification and post-operative functional outcome and b) improvement in range of motion (before–after surgery) were calculated by using Spearman’s correlation coefficient. Statistical analysis was performed with IBM SPSS Statistics V23 (IBM Corporation, Armont, NY, USA). Tables and figures were created by using Microsoft Excel and Word (Microsoft, Redmond, Washington, USA).
Results
Of the 605 patients screened 100 patients were included. The main reasons against study inclusion were an elevated blood pressure, incompliance and predominantly the inability to waive NSAIDS for five days prior to surgery.
Of 100 patients 95 (44 women and 51 men) were included for ITT analysis (48 in DIC-group, 47 in ETO-group). The study patients were between 39 and 80 years old. Demographics were evenly distributed between both groups (see Table 3). Five patients were excluded from analysis since one patient denied surgery after being included in the study, one patient had a perioperative femur shaft fracture (and therefore different surgery), one patient refused to take any study medication and two patients had a different surgical approach (not Bauer’s approach).
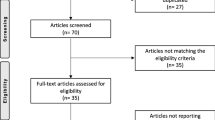
The study flow is illustrated, according to CONSORT, in Fig. 1.
Study flow chart according to CONSORT (DIC = diclofenac; ETO = etoricoxib; AE = adverse event), see also [16]
Compliance
The 95 patients showed a high compliance. Forty-two patients (87.5 %) of the DIC-group and 43 patients (91.5 %) of the ETO-group completed the nine days protocol, although there was a mild decrease in both groups from day one to day seven after surgery. Two patients of each group complained of nausea, one patient of the ETO group had elevated blood pressure. Two patients of the ETO group and three patients of the DIC group felt only low pain, which resulted in a personal decline of willingness to take any pain medication.
Incidence of heterotopic ossifications
Ninety-five patients were contacted for a physical and radiological follow-up examination 6 months after surgery. Six of 95 patients (6 %) were lost to follow-up. The reasons were incompliance or a lack of transportation to the hospital.
The overall HO rate was 37.8 % six months after THA (see Table 4). HOs were detected in 38.6 % (17 of 44 patients) of the DIC-group and 37.8 % (17 of 45 patients) of the ETO-group. Only Brooker grades 1 and 2 were found and there was no statistical significant difference between the two study groups (p = 0.871, Mann Whitney U test). No aseptic loosenings were detected.
Ad hoc analysis revealed no significant difference in postoperative range of motion between the two study groups on screening day, seven days and six months post-operative. All patients in both groups had a significant increase in ROM (except extension) six months after THA compared to pre-op (see Table 5).
The entire patient collective (both groups) showed a significant negative correlation between ossification and hip abduction and internal rotation (see Table 6). This means that an increase of HO formation most likely decreases hip abduction and internal rotation.
Complications
There was no significant difference in the rate of adverse events (n = 126) and serious adverse events (SAE) between both study groups. Only six of 64 (9.4 %) adverse events (AEs) in the DIC group and eight of 62 (12.9 %) AEs in the ETO group were evaluated to be related to the study medication. The most frequent AEs in both groups were post-operative pain (n = 43), nausea (n = 13), vomiting (n = 9), dizziness (n = 5) and diarrhoea (n = 5). Most of these symptoms have been described before in the official drug information of both investigational drugs and could be associated with morphine consumption especially in the first days after THA.
During the trial (9 days) two SAEs occurred, which were graded as “not related to study medication”. One patient suffered a femoral fracture during THA (DIC group), which led to study exclusion and one patient (ETO group) had haemorrhoidal bleeding five days after surgery.
During the following six months further incidences or symptoms were reported and registered as SAEs, but assessed not to be related to the study medication: a post-operative lymphadenectomy (ETO), a thrombosis (DIC) and pulmonary embolism (DIC), a rib fracture (ETO) and a post-operative seroma (ETO). SAEs were analysed and reported. All patients had a full recovery. A premature unblinding was not required.
Discussion
HO formations often appear six to 12 weeks after THA surgery and do not seem to increase in size afterwards [9, 18]. HO prophylaxis has to take place shortly after tissue trauma (i.e. surgery) during the initial inflammatory tissue response. Currently, there are no further prophylactic options after the HO stage of fibroproliferation and chondrogenesis [19]. If an oral prophylaxis is waived, the incidence of HO after THA can possibly rise to 76 % with higher numbers of symptomatic Brooker grades 3 and 4, which often require surgical excision for therapy [7].
Numerous trials examined oral HO prophylaxis during the last 30 years. Indomethacin was found effective and often referred to as the gold standard. It is mostly given for one to six weeks after surgery or trauma [18]. An alternative or addition for oral HO prophylaxis is perioperative radiotherapy (pre- or post-operative) in risk patients, who are prone to HO formation [20].
Ibuprofen can reduce HO rates after THA, but the clinical outcome is similar to placebo [21]. Acetylsalicylic acid (aspirin) is not suited for an effective oral prophylaxis [22]. Non-selective NSAIDs can have damaging side-effects on the gastrointestinal system, reduce thrombocyte aggregation and are nephrotoxic [23, 24].
Celecoxib (COX-II blocker) had fewer gastrointestinal adverse reactions in comparison to indomethacin if taken for 20 post-operative days after THA [25]. Xue et al. (2009) concluded in a meta-analysis that selective COX-II blockers are equally effective for oral HO prophylaxis after THA compared to non-selective NSAIDs [13]. Two recent studies investigated celecoxib after THA and confirmed this assumption [15, 26].
The main finding of this current trial is that both, etoricoxib and diclofenac are equally effective in reducing HO rates (37.8 % and 38.6 %). Although all study patients improved significantly in ROM after primary THA a significant negative correlation was found in the combined patient sample between HO incidence and limited internal rotation and abduction. This indicates that HO formations had an impact on the patients’ outcome, even if the HO size is small (Brooker 1 and 2).
The results of this current trial are in line with a recent study, which is to our knowledge the only other study to investigate etoricoxib for HO prophylaxis [7]. Brunnekreef et al. found a comparably high HO incidence for etoricoxib (38 %) and also only Brooker grades 1 (31 %) and 2 (7 %) six months after cemented THA. Their study group, which received etoricoxib for seven post-operative days, was compared to two historical groups of patients, which received either indomethacin (27 % HO rate) or no prophylaxis (76 % HO rate) [7].
This current study has possible limitations. First, the sample size of 95 patients could not find a significant supremacy of etoricoxib. This trial was powered to detect a difference for the primary outcome (blood loss) between both study groups. Nevertheless, our secondary outcome (HO prevalence) was tested in an explorative manner. Future trials, i.e. multi-centre study, could use our results for power analysis to further explore our findings confirmatively. Furthermore, Brunnekreef et al. found almost identical results for etoricoxib in a similar small study group (42 patients). In contrast to our study, Brunnekreef et al. only compared their study group to two “historical patient groups” [7]. Second, the double-blinded study design allowed an evaluation of the six months postop radiographs by only one senior orthopaedic surgeon. This aimed to reduce the inter-observer variability, which was reported, especially for higher Brooker grades (>2) [27, 28]. However, although a preference of either study group was not possible, the size of HO formations could have been underrated. The very homogenous distribution of Brooker grades between both study groups indicated a balanced and realistic assessment. In addition, as mentioned above, Brunnekreef et al. found an almost identical HO rate for etoricoxib and also no grade 3 and 4 formations six months after THA [7]. Third, the HO incidence was calculated among all patients (89 of 95), who were available for follow-up, although only 42 patients (87.5 %) of the diclofenac and 43 patients (91.5 %) of the etoricoxib group completed the full nine days protocol. The assessed HO incidence in both groups could possibly be too high. Finally, due to ethical reasons, we did not have a control group without oral HO prophylaxis, to compare the efficacy of both study medications.
A further clinically relevant finding of this current trial is that a short period of oral HO prophylaxis (seven post-operative days) seems to be sufficient. Although the HO incidence was still over 30 % and a negative correlation with ROM was detected, large and symptomatic HO formations did not occur. Some authors have recommended an oral HO prophylaxis for four to six weeks after THA, others described an effective HO prophylaxis with a seven to 20 days protocol [6, 25]. The concept of a short period of oral HO prophylaxis (1–2 weeks after surgery or trauma) offers a reduction of potential cardiovascular and gastrointestinal risks, which can occur with long-term drug use [29, 30]. This will increase patients’ safety during post-operative recovery and improve the clinical outcome. Furthermore, this effect could also be used in traumatology to further reduce HO rates (i.e. after elbow or acetabular fracture) and limit the risk of bony non-unions [31, 32].
Conclusion
This trial was able to confirm that both, etoricoxib and diclofenac are effective for oral HO prophylaxis after cementless THA. A short peri-operative period of nine days seems to be sufficient to successfully limit the rate and size of HO formations and to increase patients’ safety by reducing potential side-effects, which can occur with long-term drug intake. Furthermore there was a significant negative correlation between HO incidence and ROM (internal rotation and abduction), which underlines that HO formations have an impact on the patients’ outcome. The findings of this study support a routine HO prophylaxis after THA to ensure a full recovery and high patient satisfaction.
References
Beckmann JT, Wylie JD, Kapron AL et al (2014) The effect of NSAID prophylaxis and operative variables on heterotopic ossification after hip arthroscopy. Am J Sports Med. doi:10.1177/0363546514526361
Hamid N, Ashraf N, Bosse MJ et al (2010) Radiation therapy for heterotopic ossification prophylaxis acutely after elbow trauma: a prospective randomized study. J Bone Joint Surg Am 92:2032–2038. doi:10.2106/JBJS.I.01435
Griffin SM, Sims SH, Karunakar MA et al (2013) Heterotopic ossification rates after acetabular fracture surgery are unchanged without indomethacin prophylaxis. Clin Orthop Relat Res. doi:10.1007/s11999-013-2871-4
Guo JJ, Tang N, Yang HL et al (2010) Impact of surgical approach on postoperative heterotopic ossification and avascular necrosis in femoral head fractures: a systematic review. Int Orthop 34:319–322. doi:10.1007/s00264-009-0849-3
Neal B, Gray H, MacMahon S, Dunn L (2002) Incidence of heterotopic bone formation after major hip surgery. ANZ J Surg 72:808–821
Macfarlane RJ, Ng BH, Gamie Z et al (2008) Pharmacological treatment of heterotopic ossification following hip and acetabular surgery. Expert Opin Pharmacother 9:767–786. doi:10.1517/14656566.9.5.767
Brunnekreef JJ, Hoogervorst P, Ploegmakers MJ et al (2013) Is etoricoxib effective in preventing heterotopic ossification after primary total hip arthroplasty? Int Orthop 37:583–587. doi:10.1007/s00264-013-1781-0
Neal B (2003) Effects of heterotopic bone formation on outcome after hip arthroplasty. ANZ J Surg 73:422–426
Ahrengart L (1991) Periarticular heterotopic ossification after total hip arthroplasty. Risk factors and consequences. Clin Orthop Relat Res 49–58
Eggli S, Rodriguez J, Ganz R (2000) Heterotopic ossification in total hip arthroplasty: the significance for clinical outcome. Acta Orthop Belg 66:174–180
Neal BC, Rodgers A, Clark T et al (2000) A systematic survey of 13 randomized trials of non-steroidal anti-inflammatory drugs for the prevention of heterotopic bone formation after major hip surgery. Acta Orthop Scand 71:122–128. doi:10.1080/000164700317413076
Pellegrini VD Jr, Gregoritch SJ (1996) Preoperative irradiation for prevention of heterotopic ossification following total hip arthroplasty. J Bone Joint Surg Am 78:870–881
Xue D, Zheng Q, Li H et al (2011) Selective COX-2 inhibitor versus nonselective COX-1 and COX-2 inhibitor in the prevention of heterotopic ossification after total hip arthroplasty: a meta-analysis of randomised trials. Int Orthop 35:3–8. doi:10.1007/s00264-009-0886-y
Grohs JG, Schmidt M, Wanivenhaus A (2007) Selective COX-2 inhibitor versus indomethacin for the prevention of heterotopic ossification after hip replacement: a double-blind randomized trial of 100 patients with 1-year follow-up. Acta Orthop 78:95–98. doi:10.1080/17453670610013484
Lavernia CJ, Contreras JS, Villa JM, Rossi MD (2013) Celecoxib and heterotopic bone formation after total hip arthroplasty. J Arthroplasty. doi:10.1016/j.arth.2013.06.039
Winkler SH, Barta S, Kehl V et al (2016) Perioperative blood loss and gastrointestinal tolerability of etoricoxib and diclofenac in total hip arthroplasty (ETO-DIC study): a single-center, prospective double-blinded randomized controlled trial. Curr Med Res Opin 32(1):37–47. doi:10.1185/03007995.2015.1100987
Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55:1629–1632
Board TN, Karva A, Board RE et al (2007) The prophylaxis and treatment of heterotopic ossification following lower limb arthroplasty. J Bone Joint Surg (Br) 89:434–440. doi:10.1302/0301-620X.89B4.18845
Shimono K, Uchibe K, Kuboki T, Iwamoto M (2014) The pathophysiology of heterotopic ossification: current treatment considerations in dentistry. Jpn Dent Sci Rev 50:1–8. doi:10.1016/j.jdsr.2013.07.003
Sheybani A, Tennapel MJ, Lack WD et al (2014) Risk of radiation-induced malignancy with heterotopic ossification prophylaxis: a case–control analysis. Int J Radiat Oncol Biol Phys. doi:10.1016/j.ijrobp.2014.03.008
Fransen M, Anderson C, Douglas J et al (2006) Safety and efficacy of routine postoperative ibuprofen for pain and disability related to ectopic bone formation after hip replacement surgery (HIPAID): randomised controlled trial. BMJ 333:519. doi:10.1136/bmj.38925.471146.4F
Neal BC, Rodgers A, Gray H et al (2000) No effect of low-dose aspirin for the prevention of heterotopic bone formation after total hip replacement: a randomized trial of 2,649 patients. Acta Orthop Scand 71:129–134. doi:10.1080/000164700317413085
Laine L, Curtis SP, Cryer B et al (2007) Assessment of upper gastrointestinal safety of etoricoxib and diclofenac in patients with osteoarthritis and rheumatoid arthritis in the Multinational Etoricoxib and Diclofenac Arthritis Long-term (MEDAL) programme: a randomised comparison. Lancet 369:465–473. doi:10.1016/S0140-6736(07)60234-7
Laine L, Curtis SP, Cryer B et al (2010) Risk factors for NSAID-associated upper GI clinical events in a long-term prospective study of 34 701 arthritis patients. Aliment Pharmacol Ther 32:1240–1248. doi:10.1111/j.1365-2036.2010.04465.x
Romanò CL, Duci D, Romanò D et al (2004) Celecoxib versus indomethacin in the prevention of heterotopic ossification after total hip arthroplasty. J Arthroplasty 19:14–18
Oni JK, Pinero JR, Saltzman BM, Jaffe FF (2014) Effect of a selective COX-2 inhibitor, celecoxib, on heterotopic ossification after total hip arthroplasty: a case-controlled study. Hip Int. doi:10.5301/hipint.5000109
van der Heide HJL, Spruit M, Slappendel R et al (2004) Prophylaxis for heterotopic ossification after primary total hip arthroplasty. A cohort study between indomethacin and meloxicam. Acta Orthop Belg 70:240–246
Zhang H, Guo W, Zhang K, Lou Z (2013) Comment on Brunnekreef et al.: Is etoricoxib effective in preventing heterotopic ossification after primary total hip arthroplasty? Int Orthop 37:1629. doi:10.1007/s00264-013-1943-0
Oviedo JA, Schroy PC (2005) Does celecoxib use increase the risk of cardiovascular events? Gastroenterology 129:1348–1350. doi:10.1053/j.gastro.2005.08.029
Bresalier RS, Sandler RS, Quan H et al (2005) Cardiovascular events associated with rofecoxib in a colorectal adenoma chemoprevention trial. N Engl J Med 352:1092–1102. doi:10.1056/NEJMoa050493
Pountos I, Georgouli T, Calori GM, Giannoudis PV (2012) Do nonsteroidal anti-inflammatory drugs affect bone healing? a critical analysis. ScientificWorldJournal. doi:10.1100/2012/606404
Vuolteenaho K, Moilanen T, Moilanen E (2008) Non-steroidal anti-inflammatory drugs, cyclooxygenase-2 and the bone healing process. Basic Clin Pharmacol Toxicol 102:10–14. doi:10.1111/j.1742-7843.2007.00149.x
Acknowledgments
The excellent help of the following is highly appreciated:
Karoline Fischer, Ferdinand Wagner M.D., Franz-Xaver Köck M.D., Eva-Maria Bauser M.D., Christoph Schröter M.D., Jochen Wolfsteiner M.D., Jens Schaumburger M.D., Guido Heers M.D.
Department of Orthopaedic Surgery (Regensburg University Medical Centre, Bad Abbach, Germany).
We thank Taylor & Francis Ltd. (www.tandfonline.com) for granting us permission to reproduce parts of our material in this publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
J.G. reports connections to Springer International outside the submitted work. S.W. has received grants from the Medical faculty of the University of Regensburg outside the submitted work. HRS, TV, MH, SB, VK and BC report no competing interests.
Funding
This study was an investigator initiated trial (IIT) and funded by MSD Sharp & Dohme, Germany. The sponsor did not contribute to the preparation of this article.
Rights and permissions
About this article
Cite this article
Winkler, S., Springorum, HR., Vaitl, T. et al. Comparative clinical study of the prophylaxis of heterotopic ossifications after total hip arthroplasty using etoricoxib or diclofenac. International Orthopaedics (SICOT) 40, 673–680 (2016). https://doi.org/10.1007/s00264-015-3077-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3077-z