Abstract
Purpose
The potential influence of acetabular component orientation on iliopsoas impingement in total hip arthroplasty (THA) has not been previously quantified. The aim of the present study was to utilize pre- and post-operative CT-based 3D models to quantify iliopsoas impingement on acetabular components, and to identify any potential factors associated with iliopsoas impingement.
Methods
Iliopsoas muscle was modelled from pre-operative CT scans and transferred to the post-operative 3D models in 19 THAs. The volume and the area of the overlap between iliopsoas muscle and acetabular cup (iliopsoas volume & area) was measured on axial and sagittal images. Most protruded lengths of cup uncovered by acetabular bone were measured on axial sagittal scan of CT scans. Version of acetabulum, acetabular cup, and the difference between the two (version difference) were also measured with cup inclination and size. Linear regression analysis was performed to identify any factor influencing iliopsoas impingement.
Results
Iliopsoas impingement volume and area were 100.6 ± 226.1 (range, 0.0–663.9) mm³ and 52.6 ± 102.0 (0.0–342.3) mm³, respectively. The protruded lengths on axial and sagittal view were 6.9 ± 5.3 (0.0–16.0) and 2.1 ± 2.7 (0.0–8.0). Linear regression model showed that version difference was significantly related to the iliopsoas impingement volume and area (beta = −0.709, p = 0.041 for volume, and beta = −0.684, p = 0.047 for area).
Conclusions
The results of this study demonstrate that iliopsoas impingement on acetabular components was influenced by the version difference between pre-operative acetabular bone and acetabular component rather than the magnitude of post-operative cup version alone.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty is one of the most successful procedures in the orthopaedic field [1]. Patient satisfaction is generally high following this procedure; however, a number of patients have functional difference according to the procedures [2], or pain after the operation [3]. Among the possible various causes, iliopsoas impingement (IPI) and tendinitis is one possible reason for persistent groin pain after THA [1]. The incidence of iliopsoas impingement after total hip replacement (THR) is reported up to 4.3 % [4], however the mechanism is not yet fully understood.
For the evaluation of iliopsoas impingement, one or more imaging studies can be used for diagnosis and treatment [5]. Although ultrasonography described in several studies is helpful in evaluating dynamic status of iliopsoas [6–9], it has not been widely used and it is highly dependent on the experience and technique of ultrasonographers [5]. For computed tomography (CT), it is known to enable diagnosis with a good sensitivity and specificity for iliopsoas impingement [10]; however, to our knowledge, only two studies reported the evaluation of iliopsoas impingement using CT scans [10, 11]. Although these two studies used CT scans to measure acetabular component version [10, 11], the potential influence of acetabular component orientation on iliopsoas impingement in patients with THA has not been reported. To date, there have been no quantitative analyses of 3-dimensional (3D) evaluation of iliopsoas impingement using CT scans. Although CT scans have achieved widespread popularity owing to their easy interpretation, accuracy and precision, CT-scan accuracy of anatomical hip evaluation was debated recently when it was compared to the 3D modelling technique [12, 13], the virtual equivalent of the gold standard. Therefore, the aim of the present study was to utilize pre- and post-operative CT-based 3D models to quantify iliopsoas impingement on acetabular components, and to identify any potential factors associated with iliopsoas impingement. We hypothesized that the cup anteversion would correlate with the amount of impingement between iliopsoas and the acetabular component.
Methods
Patients
Nineteen hips (7 left and 12 right) in 16 patients (3 males and 13 females) with primary osteoarthritis who underwent robotic assistance cementless THA (RIO Robotic Arm Interactive Orthopedic System, Stryker Mako, Fort Lauderdale, FL, USA) between January 2012 and April 2013 were included in this study. Approval of the institutional review board was obtained and each patient provided written informed consent for this study. Mean age was 64.2 ± 7.4 (range, 47–73) years. Mean height was 167.0 ± 7.6 (range, 155–183) cm, mean weight was 72.6 ± 17.6 (54–111) kg, and mean body mass index (BMI) was 25.3 ± 5.3 (18.5–35.8). Prior to the scheduled operation, CT scans of the each patient from the fifth lumbar vertebra to the distal femur was obtained (Sensation 64, Siemens, Germany) with an image resolution of 512 × 512 pixels and a voxel size of 0.97 × 0.97 × 0.60 mm using 140 kVp. A posterior approach was used in all cases and a tapered stem (Linear stem, DJO Global, Vista, CA, USA) was inserted using a haptic robotic hip system (MAKOplasty® total hip application; MAKO Surgical Corporation, Ft. Lauderdale, FL, USA). Although the utility of robot-assisted THA was outside the scope of the present study, the study was limited to those patients who underwent robot-assisted THAs as CT is routinely performed for surgical planning purposes in these patients. Thus, inclusion of these THA patients avoided exposing additional radiation to the potential study patients. Post-operative hip CT scan of the each patient was also obtained at a mean of 10.0 ± 2.3 (range 6–14) months after surgery. The mean follow up was 19.6 ± 4.8 months (range, 12–24 months). There was no case of infection or dislocation during the follow-up period.
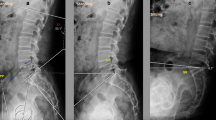
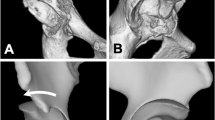
Using a commercially available program (Rhinoceros®, Robert McNeel and Associates, Seattle, WA, USA), surface models of pre-operative pelvis and femur, and those of post-operative pelvis, femur, and THA components were created from CT scans in accordance with a previously published study protocol [14]. Iliopsoas (IP) muscle contour was created from the pre-operative CT scans to avoid the artefacts of the post-operative CT scans. The iliopsoas muscle model that was created was transferred together with pre-operative pelvis models to the post-operative 3D hip models based on the pelvic bones (Fig. 1). The deviation of the distances between surface models of the pre- and post-operative pelves were 0.98 ± 0.24 mm. Overlap volume and contact area (iliopsoas impingement volume and area) on the cup side between iliopsoas muscle and acetabular component were calculated. The most protruded lengths of acetabular cup uncovered by the acetabular bone were also measured directly on the post-operative 2D CT images on axial and sagittal view based on the method by Cyteval et al. [10] (Fig. 2).
All created models were imported to the MATLAB program (The Mathworks Inc., Natick, MA) for measurement of the true (anatomical) anteversion and the inclination of native acetabulum preoperatively and the acetabular component postoperatively. First, the pelvic coordinate system was determined based on a previous study by Murray et al. [15]. The best-fitting 3D opening plane was determined after digitizing multiple points which are distributed on the rim of the acetabulum or cup, and each targeted angle of anteversion and inclination was obtained based on this opening plane.
Statistical analysis
For descriptive analysis, all data was presented using a mean value and a standard deviation with a range. Linear regression analyses were performed to determine the influencing factors for iliopsoas impingement volume and area between iliopsoas muscle and acetabular component. Further analysis of comparisons of the parameters of iliopsoas impingement (iliopsoas volume and area, and protruded lengths) between the hips with the cup anteverted greater than 10 degrees relative to native acetabular version and those with anteverted less than 10 degrees relative to native acetabular version was performed using Mann–Whitney U test. Statistical analyses were performed with SPSS software for Windows (version 20.0, SPSS, Chicago, IL) and p value of <0.05 was considered significant.
Results
Iliopsoas impingement (measured as overlap between iliopsoas muscle and acetabular cup) was detected in more than half of the hips (11 hips) in the study. The iliopsoas impingement volume and area on 3D models were 100.6 ± 226.1 (range, 0.0–663.9) mm³ and 52.6 ± 102.0 (range, 0.0–342.3) mm³ (Table 1). There was iliopsoas impingement volume over 500 mm³ in three cases. Protruded lengths were 6.9 ± 5.3 (range, 0.0–16.0) mm on axial view and 2.1 ± 2.7 (range, 0.0–8.0) on sagittal view, respectively (Table 1).
In the linear regression analyses to determine the potential factors on the parameters of iliopsoas impingement (iliopsoas impingement volume and area, and protruded lengths), the version difference was significantly related to the iliopsoas impingement volume and area (standardized regression coefficient (R) = −0.709, p = 0.041 for volume, and R = −0.684, p = 0.047 for area). This indicates that the difference in the cup version relative to the pre-operative native acetabular version is associated with iliopsoas impingement with greater overlap between iliopsoas muscle and acetabular component (Table 2). Interestingly however, other factors such as the absolute magnitude of cup version, cup inclination or cup size were not correlated to the iliopsoas impingement volume or area.
Further analyses of comparisons of parameters of iliopsoas impingement according to the version difference between native acetabulum and acetabular component revealed that THA hips with cup version anteverted greater than 10° relative to the native acetabular version showed significantly lower iliopsoas impingement volume and area along with protruded lengths than those with cup version anteverted less than 10° relative to the native acetabular version (Table 3).
Discussions
Iliopsoas impingement is an important differential diagnosis in patients with painful total hip arthroplasty (THA). Prevention of iliopsoas impingement in THAs is important as it often needs surgical treatment such as iliopsoas muscle tenotomy or revision of acetabular component [1]. The present study quantified the influence of the acetabular component orientation on iliopsoas impingement using CT scans and CT-based 3D models. The results of this study demonstrate that iliopsoas impingement on the acetabular component was influenced by the version difference between acetabular bone and acetabular component rather than the absolute magnitude of post-operative cup version alone.
For the diagnostic imaging tools for iliopsoas impingement, ultrasonography has been reported in several studies as helpful in diagnosis and treatment [6–9]. It is known that, in the hands of an experienced radiologist, ultrasonography can show a greater degree of soft tissue contrast than CT scans [7–9], and the iliopsoas tendon is frequently displaced antero-medially by the acetabular component in iliopsoas impingement patients [16]. Peritendinous injection can be performed during the ultrasonography, but there is concern for its temporary effect [5] or the risk of infection [1]. Even though CT scans cannot observe the dynamic status of the iliopsoas muscle, there is an advantage to measure acetabular component version and to detect how much of the acetabular component is uncovered [5, 10, 11]. Although it is known that CT scans enable diagnosis with a good sensitivity and specificity for iliopsoas impingement [10], the information regarding CT scans on iliopsoas impingement is limited. Cyteval et al. reported that acetabular component prominence >12 mm was seen on CT in patients with IPI [10], and Dora et al. described that the mean prominence of the acetabular component on CT scans was reported to be 5.8 mm [11]. However, it remains unknown whether acetabular component version is related to iliopsoas impingement [5] or which factors influence iliopsoas impingement. Furthermore, given that there are controversies over the accuracy of CT studies with 2D images [12, 13], information using 3D images along with 2D images would be helpful to understand the features of the IPI on acetabular components. In the present study utilizing CT scans and CT-based 3D models for evaluation of iliopsoas impingement, there were overlaps between iliopsoas muscle and acetabular component in more than half of the hips, and in three cases, there was iliopsoas impingement volume of over 500 mm³. Furthermore, the difference between the native acetabular version and cup version influenced the iliopsoas impingement rather than the acetabular cup version as previous studies reported [17–19]. This finding indicates that surgeons may need to consider a cup version relative to the native acetabulum to minimize the risk of iliopsoas impingement after a THA.
In our further analysis of comparisons of parameters of iliopsoas impingement on acetabular components (iliopsoas impingement volume and area, and protruded lengths), according to the version difference between acetabular and cup versions, all potential impingement parameters were significantly lower when cup version was anteverted more than 10 degrees compared to the native acetabular version (Table 3) than those with the cup anteverted less than 10 degrees compared to the acetabulum. This indicates that the probability of iliopsoas impingement would decrease if cup version is anteverted over 10 degrees compared to the native acetabular version. In each case, the acetabular cup was covered more by the native acetabulum when cup version is anteverted more than 10 degrees compared to the native acetabular version. For the cup version, we acknowledge that multiple factors should be considered for the acetabular cup version such as native acetabular version or combined anteversion [20]. However, in perspective of iliopsoas impingement, the present study data suggest that acetabular cup version less than the native acetabular version should be avoided to minimize the risk of iliopsoas impingement.
This study has several limitations. First, it was a retrospective study. We were not able to determine that the patients’ symptom was specifically related to the impingement of iliopsoas muscle, thus we focused only on images rather than clinical symptoms. Second, we segmented iliopsoas muscle from preoperative CT scans and transferred it to the postoperative 3D models. As the femur position of postoperative CT scans may differ from that of preoperative CT scans, the iliopsoas position of postoperative CT scans could have been changed. However, we performed this study as we focused on the overlapped volume and area between the preoperative iliopsoas muscle contour and postoperative acetabular cup, and the focused area of iliopsoas impingement in this study is the inguinal area which is less mobile than the distal insertion area of iliopsoas. Finally, the present study investigated primary THA cases without severe dysplasia or osteophyte formations. When there is a dysplasia of the anterior wall of the native acetabulum or extensive osteophytes, it is often challenging to determine the cup version during the operation and care should be taken to avoid relying solely on the anatomical acetabular ring to antevert the acetabular component. Further studies with patients with dysplasia would be necessary.
In conclusion, the results of this study demonstrate that iliopsoas impingement on the acetabular component was influenced by the version difference between pre-operative acetabular bone and acetabular component rather than the magnitude of post-operative cup version alone. This finding indicates that surgeons need to consider a cup version relative to the native acetabulum to avoid iliopsoas impingement after a THA.
References
Duffy PJ, Masri BA, Garbuz DS, Duncan CP (2005) Evaluation of patients with pain following total hip replacement. J Bone Joint Surg Am 87(11):2566–2575
Reichert JC, Volkmann MR, Koppmair M, Rackwitz L, Ludemann M, Rudert M, Noth U (2015) Comparative retrospective study of the direct anterior and transgluteal approaches for primary total hip arthroplasty. Int Orthop 39(12):2309–2313. doi:10.1007/s00264-015-2732-8
Britton AR, Murray DW, Bulstrode CJ, McPherson K, Denham RA (1997) Pain levels after total hip replacement: their use as endpoints for survival analysis. J Bone Joint Surg (Br) 79(1):93–98
Ala Eddine T, Remy F, Chantelot C, Giraud F, Migaud H, Duquennoy A (2001) Anterior iliopsoas impingement after total hip arthroplasty: diagnosis and conservative treatment in 9 cases. Rev Chir Orthop Reparatrice Appar Mot 87(8):815–819
Lachiewicz PF, Kauk JR (2009) Anterior iliopsoas impingement and tendinitis after total hip arthroplasty. J Am Acad Orthop Surg 17(6):337–344
Adler RS, Buly R, Ambrose R, Sculco T (2005) Diagnostic and therapeutic use of sonography-guided iliopsoas peritendinous injections. AJR Am J Roentgenol 185(4):940–943. doi:10.2214/AJR.04.1207
Bianchi S, Martinoli C, Keller A, Bianchi-Zamorani MP (2002) Giant iliopsoas bursitis: sonographic findings with magnetic resonance correlations. J Clin Ultrasound 30(7):437–441. doi:10.1002/jcu.10093
Rezig R, Copercini M, Montet X, Martinoli C, Bianchi S (2004) Ultrasound diagnosis of anterior iliopsoas impingement in total hip replacement. Skeletal Radiol 33(2):112–116. doi:10.1007/s00256-003-0703-4
Wank R, Miller TT, Shapiro JF (2004) Sonographically guided injection of anesthetic for iliopsoas tendinopathy after total hip arthroplasty. J Clin Ultrasound 32(7):354–357. doi:10.1002/jcu.20043
Cyteval C, Sarrabere MP, Cottin A, Assi C, Morcos L, Maury P, Taourel P (2003) Iliopsoas impingement on the acetabular component: radiologic and computed tomography findings of a rare hip prosthesis complication in eight cases. J Comput Assist Tomogr 27(2):183–188
Dora C, Houweling M, Koch P, Sierra RJ (2007) Iliopsoas impingement after total hip replacement: the results of non-operative management, tenotomy or acetabular revision. J Bone Joint Surg (Br) 89(8):1031–1035. doi:10.1302/0301-620X.89B8.19208
Kim JS, Park TS, Park SB, Kim IY, Kim SI (2000) Measurement of femoral neck anteversion in 3D. Part 2: 3D modelling method. Med Biol Eng Comput 38(6):610–616
Sugano N, Noble PC, Kamaric E (1998) A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr 22(4):610–614
Tsai TY, Li JS, Wang S, Lin H, Malchau H, Li G, Rubash H, Kwon YM (2013) A novel dual fluoroscopic imaging method for determination of THA kinematics: in-vitro and in-vivo study. J Biomech 46(7):1300–1304. doi:10.1016/j.jbiomech.2013.02.010
Murray DW (1993) The definition and measurement of acetabular orientation. J Bone Joint Surg (Br) 75(2):228–232
Potter HG, Nestor BJ, Sofka CM, Ho ST, Peters LE, Salvati EA (2004) Magnetic resonance imaging after total hip arthroplasty: evaluation of periprosthetic soft tissue. J Bone Joint Surg Am 86-A(9):1947–1954
Bricteux S, Beguin L, Fessy MH (2001) Iliopsoas impingement in 12 patients with a total hip arthroplasty. Rev Chir Orthop Reparatrice Appar Mot 87(8):820–825
Lequesne M, Dang N, Montagne P, Lemoine A, Witvoet J (1991) Conflict between psoas and total hip prosthesis. Rev Rhum Mal Osteoartic 58(9):559–564
Trousdale RT, Cabanela ME, Berry DJ (1995) Anterior iliopsoas impingement after total hip arthroplasty. J Arthroplasty 10(4):546–549
Dorr LD, Malik A, Dastane M, Wan Z (2009) Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res 467(1):119–127. doi:10.1007/s11999-008-0598-4
Acknowledgments
The authors would like to acknowledge the technical guidance of Dr. Guoan Li. There was a partial funding from Mako Surgical Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical review committee statement
This study was approved by the Institutional Review Board at the authors’ institute.
Rights and permissions
About this article
Cite this article
Park, K.K., Tsai, TY., Dimitriou, D. et al. Three-dimensional in vivo difference between native acetabular version and acetabular component version influences iliopsoas impingement after total hip arthroplasty. International Orthopaedics (SICOT) 40, 1807–1812 (2016). https://doi.org/10.1007/s00264-015-3055-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3055-5