Abstract
Purpose
The purpose of this study was to identify risk factors of post-operative malalignment in medial unicompartmental knee arthroplasty (UKA) using multivariate logistic regression.
Methods
We retrospectively enrolled 92 patients who had 127 medial UKAs. According to post-operative limb mechanical axis (hip-knee-ankle [HKA] angle), 127 enrolled knees were sorted into acceptable alignment with HKA angle within the conventional ± 3 degree range from a neutral alignment (n = 73) and outlier with HKA angle outside ± 3 degree range (n = 54) groups. Multivariate logistic regression was used to analyse risk factors including age, gender, body mass index, thickness of polyethylene tibial insert, pre-operative HKA angle, distal femoral varus angle (DFVA), femoral bowing angle (FBA), tibial bone varus angle (TBVA), mechanical distal femoral and proximal tibial angles, varus and valgus stress angles, size of femoral and tibial osteophytes, and femoral and tibial component alignment angles.
Results
Pre-operative DFVA, TBVA and valgus stress angle were identified as significant risk factors. As DFVA increased by one degree, malalignment was about 45 times probable (adjusted OR 44.871, 95 % CI 2.608–771.904). Shift of TBVA and valgus stress angle to a more varus direction were also significant risk factors (adjusted OR 13.001, 95 % CI 1.754–96.376 and adjusted OR 2.669, 95 % CI 1.054–6.760).
Conclusions
Attention should be given to the possibility of post-operative malalignment during medial UKA in patients with a greater varus angle in pre-operative DFVA, TBVA and valgus stress angle, especially with a greater varus DFVA, which was the strongest predictor for malalignment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicompartmental knee arthroplasty (UKA) is a treatment option for single compartment knee osteoarthritis, especially in the medial compartment. Among various factors that have been associated with post-operative outcome and longevity of UKA, post-operative knee alignment is critical to the inhibition of the progression of osteoarthritis and implant-related complications including early loosening [1–6]. The correction of knee alignment achieved at surgery is also the single most important factor that can be controlled by the surgeon during surgery. Thus, knee alignment axes after UKA have been used as a measure of the outcome of UKA and a risk factor of early failure. The relationship between the post-operative knee alignment and clinical outcomes has been well studied [7–9], as has survivorship of UKA [1–6], while there is a paucity of studies regarding the risk factors of post-operative malalignment in UKA [10, 11]. In this study, we investigated the risk factors of the post-operative malalignment of medial UKA by assessing clinical parameters including age, gender, and body mass index (BMI) and various radiographic parameters.
Enrolled UKAs were sorted into two groups according to the knee mechanical axis angle (KMAA) measured in a standing anteroposterior (AP) radiograph of the whole lower extremity taken three months post-operatively. For medial UKA, neutral correction or slight undercorrection has been recommended because overcorrection may increase the progression of osteoarthritis in the lateral compartment, whereas undercorrection may accelerate polyethylene wear and recurrence of deformity [6, 8, 12]. Although neutral correction or slight undercorrection of the knee alignment angle has been suggested in previous studies to minimize UKA failure rates, the optimal level of correction still remains debatable [6, 8, 12]. Considering previous findings [6, 12–14] concerning post-operative knee alignment after medial UKA, we aimed at the neutral knee alignment of hip-knee-ankle (HKA) axis during surgery. Acceptable alignment after UKA was defined as knee alignment of HKA axis within ±3 degrees of neutral, and malalignment as outside ±3 degrees.
It was hypothesized that one or more pre-operative or intra-operative factors could reasonably predict post-operative malalignment after medial UKA. The purpose of this study was to identify risk factors that predict post-operative malalignment in medial UKA using multivariate logistic regression.
Materials and methods
Institutional review board approval was obtained for this retrospective trial. From January 2013 through March 2015, 131 medial UKAs in 94 patients were consecutively performed by a single surgeon using a fixed-bearing Uni-compartmental High-Flex Knee System (Zimmer, Warsaw, ID, USA). The pre-operative varus-valgus stress radiographs with the knee extended in supine position and the whole extremity radiographs of the knee in extended weight bearing were studied. Inclusion criteria were patients who underwent the pre-operative varus-valgus stress radiographs before UKA for medial degenerative arthritis with varus deformity. Exclusion criteria were post-traumatic arthritis and inappropriate varus-valgus stress radiograph due to flexion contracture. Of 131 medial UKAs, four cases were excluded: two cases were post-traumatic arthritis and two cases underwent inappropriate varus-valgus stress radiograph due to flexion contracture. The final 127 medial UKAs in 92 patients were reviewed respectively.
Radiographic evaluations
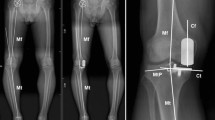
Pre-operative knee mechanical axis was assessed using the HKA angle determined using a standing AP radiograph of the whole lower extremity. The hip centre, notch centre of distal femur and ankle talus centre were also assigned and connected, and the angle between these lines was defined as the knee mechanical axis angle (KMAA) (Fig. 1). KMAA of zero degrees was considered a neutral knee, a valgus knee considered to be a negative value and a varus knee considered to be a positive value. Post-operative knee mechanical axis was also assessed with a similar method to pre-operative KMAA at three months post-operatively.
The knee mechanical axis angle (KMAA) was defined as the angle among the hip centre, notch centre of distal femur and ankle talus centre. The mechanical lateral distal femoral angle (mLDFA) was measured by the lateral angle between the distal femur articular surface and mechanical axis of the femur, while the medial mechanical proximal tibia angle (mMPTA) was defined as the medial angle between the knee joint line of the tibia and the mechanical axis line of the tibia
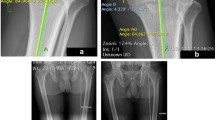
For the assessment of distal femoral varus angle (DFVA), femoral bowing angle (FBA) and mechanical lateral distal femoral angle (mLDFA) were measured. DFVA was measured using the angle between the mechanical axis and the distal anatomical axis of the femur in a standing AP radiograph of the whole lower extremity [15]. The distal anatomical axis was defined by a line connecting midpoints of the distal femoral shaft, which were 5 and 10 cm from the knee joint line (Fig. 1). The FBA was measured by the angle between lines bisecting the femur at 0 and 5 cm below the lowest portion of the lesser trochanter and a line connecting points bisecting the femur at 5 and 10 cm above distal articular surface (Fig. 2). Lateral bowing was designated with a positive value, and medial bowing was designated with a negative value. The mLDFA was measured by the lateral angle between the distal femur articular surface and mechanical axis of the femur (Fig. 1).
The femoral bowing angle (FBA) was measured by the angle between lines bisecting the femur at 0 and 5 cm below the lowest portion of the lesser trochanter and a line connecting points bisecting the femur at 5 and 10 cm above the distal articular surface. The tibial bone varus angle (TBVA) was defined as the angle between a line from the centre of the tibial spines to a point midway to the proximal tibia epiphysis and the mechanical axis line of the tibia. Osteophyte size was defined as the largest perpendicular distance from the cortical line to the outer margin of an osteophyte
Proximal tibia varus deformity was determined by the medial mechanical proximal tibia angle (mMPTA) and the tibial bone varus angle (TBVA) as described previously [16]. The mMPTA was defined as the medial angle between the knee joint line of the tibia and the mechanical axis line of the tibia (Fig. 1). The TBVA was used to determine constitutional tibia varus deformity. TBVA was defined as the angle between a line from the centre of the tibial spines to a point midway of the proximal tibia epiphysis and the mechanical axis line of the tibia (Fig. 2). A positive value represented a varus direction of the angle described.
The pre-operative varus-valgus stress radiographs with the knee extended in supine position were used to assess and classify the pre-operative medio-lateral ligament imbalance. AP varus-valgus stress radiographs were taken while a varus or valgus stress of 20 pounds was applied to the knee in extension using a Telos stress device (Austin & Associates, Fallston, MD, USA). As previously described [17], midpoints of the distal femoral shaft, which were 10 and 15 cm from the knee joint line, respectively, and the midpoints of the proximal tibial shaft, which were 7.5 and 12.5 cm from the knee joint line, were also assigned and connected on each AP varus-valgus stress radiograph (femoral midpoint line and tibial midpoint line) (Fig. 3). The angle between femoral and tibial midpoint lines was measured and defined as varus stress angle (VrSA) or valgus stress angle (VgSA) according to varus or valgus stress radiograph.
For mathematical analysis in varus-valgus stress radiograph, the value for the varus or valgus stress angle in cases with a valgus direction angle compared with neutral knee axis between femoral and tibial midpoint lines was considered to be a negative value, while the value for the varus or valgus stress angle in cases with a varus direction angle compared with the neutral knee axis was considered to be a positive value. Femoral osteophyte size and tibial osteophyte size (Fig. 2) were measured using a standing AP radiograph of the whole lower extremity. Osteophyte size was defined as the largest perpendicular distance from the cortical line to the outer margin of an osteophyte [17].
Post-operative KMAA, and femoral and tibial component alignment angles were also measured in a standing anteroposterior (AP) radiograph of the whole lower extremity (Fig. 4), three months post-operatively. The angle between a perpendicular line to the femoral component long axis and femoral mechanical axis was defined as femoral component alignment angle. The angle between a parallel line to the tibial component and tibial mechanical axis was defined as tibial component alignment angle.
Post-operative femoral component alignment angle was measured using the angle between a perpendicular line to the femoral component long axis and femoral mechanical axis. The angle between a parallel line to the tibial component and tibial mechanical axis was defined as the tibial component alignment angle. Post-operative knee mechanical axis angle (KMAA) was measured with a similar method to pre-operative KMAA
The radiographic measurements of all parameters were done by two orthopaedic surgeons who were blinded to the patient status using PiViewSTAR version 5.0.9.2 (Infinitt, Seoul, South Korea). The interobserver reliability was calculated and assessed with intraclass correlation coefficient (ICC). The ICC value for interobserver reliability ranged from 0.852 to 0.923.
Surgical technique
A fixed-bearing Zimmer Uni-compartmental High-Flex Knee System was implanted in all patients. A standard midline incision and medial parapatellar arthrotomy through a minimally invasive, quadriceps-sparing surgical exposure were used to implant the prosthesis. Medial osteophytes were removed from the femur and tibia. Using the Spacer Block (Zimmer) technique recommended by the manufacturer, tibial resection was made perpendicular to its long axis with an extra-medullary guidance system first and the femoral resection was based off the tibia cut.
After resecting the tibia, the Spacer Block was inserted into the joint space and knee alignment was checked using the alignment rod. The distal femoral cut with the knee in extension was made, ensuring the proximal tibia cut and distal femoral cut were parallel. The posterior femoral resection then created a flexion gap equal to the extension space. Thickness of the polyethylene was adjusted to ensure a well-balanced knee capable of full extension with about 2 mm medial laxity. Both femoral and tibial components were cemented in all cases.
Statistical analyses
According to post-operative KMMA, 127 enrolled UKAs were allocated to the acceptable alignment group within ±3 degrees of neutral HKA angle (group AA, n = 73) and the malalignment group outside ±3 degrees (group MA, n = 54).
Mean and range were calculated to characterize continuous variables, and percentages were calculated for discrete variables. An independent-sample t test was applied to analyse group distribution, and the Fisher’s exact test was applied to compare proportions between two groups.
For logistic regression analysis of predictors for post-operative malalignment in UKA, the variables of risk factors included age at surgery (years), gender (male versus female), body mass index (BMI), thickness of polyethylene tibial insert (mm), pre-operative KMAA (degrees), FBA (degrees), DFVA (degrees), and TBVA (degrees), VgSA (degrees), VrSA (degrees), mLDFA (degrees), mMPTA (degrees), femoral osteophyte size and tibial osteophyte size (mm), and femoral and tibial component alignment angles (degrees). To identify potential predictors of developing post-operative malalignment, we compared 16 variables of risk factors of group AA to group MA using univariate logistic regression.
Using multivariate logistic regression, combination of risk factors significant in univariate analyses were assessed and were selected in a stepwise algorithm, with variables entered and excluded for P > 0.05. The results of regression analyses were presented as odds ratios (ORs) with accompanying 95 % confidence intervals (CIs). Results were considered to be statistically significant when the null value (1.00) was absent from the CI or p-values < 0.05. Data were analysed using SPSS version 19.0 (SPSS Inc., Chicago, IL). Using G-Power 3.1 calculation software, the post-hoc analysis for the multivariate logistic regression was performed to achieve statistical power of this study. The computed power was achieved with an alpha of 0.05, a sample size of 127, and each OR and R-squared attributed to 16 independent variables using the Z test with a significance level of 0.05.
Results
The demographic and clinical scores of each group are shown in Table 1.
After statistical analysis with univariate logistic regression, nine risk factor variables among 16 independent variables were identified as potential predictors with p < 0.05. These were pre-operative KMAA, FBA, DFVA, mLDFA, mMPTA, TBVA, VgSA, femoral osteophyte size and tibial component alignment angle. Multivariate logistic regression analysis for these nine potential predictors revealed that pre-operative DFVA, TBVA, and VgSA were significant risk factors predicting post-operative malalignment after UKA.
The mean of pre-operative DFVA was 5.4 ± 0.8 degrees (range, 3.4–7.8 degrees) in group AA and 7.6 ± 1.2 degrees (range, 3.1–9.7 degrees) in group MA (p < 0.0001, 95 % CI –2.549 to –1.824). As pre-operative DFVA increased, the risk for post-operative knee malalignment also increased (p < 0.0001 in univariate analysis and p = 0.009 in multivariate analysis). The OR of pre-operative DFVA was 7.928 (95 % CI 3.840–16.369), and the adjusted OR was 44.871 (95 % CI 2.608–771.904).
The mean of pre-operative TBVA was 1.3 ± 1.8 degrees (range, –5.1 to 5.1 degrees) in group AA and 4.7 ± 1.3 degrees (range, 0.5–6.3 degrees) in group MA (p < 0.0001, 95 % CI –3.984 to –2.848). In logistic regression analysis, pre-operative TBVA with more varus direction was a significant risk factor of post-operative malalignment in univariate analysis (p < 0.0001, OR = 3.852 with 95 % CI 2.540–5.841) and multivariate analysis (p = 0.012, adjusted OR = 13.001 with 95 % CI 1.754–96.376).
There was a significant difference in pre-operative VgSA between groups AA and MA (p = 0.005, 95 % CI –2.233 to –0.406). The mean of pre-operative VgSA was –5.8 ± 2.7 degrees (range, –12.0 to 0.8 degrees) in group AA and –4.5 ± 2.3 degrees (range, –11.0 to 0.0 degrees) in group MA. In logistic regression analysis, pre-operative VgSA with more varus direction was the risk factor of post-operative malalignment in univariate analysis (p = 0.007, OR = 1.226 with 95 % CI 1.057–1.422) and multivariate analysis (p = 0.038, OR = 2.669 with 95 % CI 1.054–6.760).
The other 13 variables, except pre-operative DFVA, TBVA, and VgSA, were not significant risk factors of malalignment using univariate and multivariate logistic regression analyses. The ORs and adjusted ORs with 95 % CI for each risk factor variable are shown in Table 2.
Post-hoc tests suggested that the power of our tests ranged from 0.051 to 0.999 with 127 enrolled cases, each OR and a significance level of 0.05. The power for pre-operative DFVA was 0.999 with high OR, while the powers for BMI and post-operative mLDFA were low (0.051 and 0.062, respectively).
Discussion
The most important finding of our study is that pre-operative DFVA, TBVA, and VgSA are risk factors predicting post-operative malalignment after UKA. The primary hypothesis was supported; one or more pre-operative or intra-operative factors could reasonably predict post-operative malalignment after medial UKA.
Post-operative alignment after medial UKA of the varus osteoarthritic knee has been amply studied [1, 2, 4–9, 12–21], while only several studies [10, 11, 19, 21] have examined the risk factors of post-operative malalignment. Kim et al. [10] and Hopgood et al. [21] suggested that the thickness of polyethylene tibial insert is useful for predicting the post-operative alignment, while Tashiro et al. [19] and Mulljai et al. [11] reported pre-operative valgus stress angle measurement and coronal knee alignment as an important predictor for the post-operative alignment, respectively. Presently, pre-operative DFVA was the most significant risk factor for the post-operative malalignment of the medial UKA (p < 0.0001, adjusted OR = 44.871 with 95 % CI 2.608–771.904). Pre-operative TBVA and VgSA were also significant predictors of the post-operative malalignment. We measured the pre-operative DFVA to estimate the bony deformity of distal femur; DFVA was the most important predictor of post-operative malalignment of the medial UKA using multivariate logistic regression. Most previous studies [1, 2, 4, 10, 11, 18–22] on post-op alignment after medial UKA focused on pre-operative knee mechanical axis, valgus stress radiograph, component alignment and the thickness of polyethylene tibial insert as the risk factors of post-op malalignment, while in our study, the various bony deformities of femur and tibia including DFVA, TBVA, and FBA were evaluated as potential predictors for post-operative malalignment in medial UKA. This is the main difference between our present study and the previous studies [1, 2, 4, 10, 11, 18–22].
In our study, pre-operative TBVA was a significant risk factor, while TBVA was not a stronger predictor for post-operative malalignment than DFVA. In all enrolled cases, the range of pre-operative TBVA was –5.1 to 6.3 degrees, because we did not perform UKA in cases with pre-operative TBVA over 7 degrees in the varus direction. This may be a possible explanation for the weaker correlation of TBVA with post-operative malalignment than that of DFVA.
The role of valgus stress radiograph in UKA has been controversial. Kreitz et al. [2] suggested that pre-operative stress radiographs have overstated value in patients undergoing medial UKA, since the full extent of correctability of varus deformity cannot be determined until after removal of osteophytes. Waldstein et al. [20] reported that valgus stress radiographs provided no added benefit to the radiographic assessment of the correctability of the varus deformity. Presently, VgSA in pre-operative stress radiographs was identified as a significant risk factor of malalignment after medial UKA. This is similar to the results of a previous study [19], while VgSA showed weaker correlation with post-operative malalignment than other identified predictors, such as DFVA and TBVA.
For the effect of the tibial insert thickness on post-operative alignment, Kim et al. [10] reported that the overall changes in post-operative mechanical axis angle was significantly different according to tibial insert thickness using mobile-bearing UKA. Presently, the tibial insert thickness was not found to be a predictor for post-operative malalignment using fixed-bearing UKA. In previous studies [23, 24] comparing mobile-bearing and fixed-bearing UKAs, undercorrection in a post-operative mechanical knee axis was much more common with a fixed-bearing design than with mobile-bearing. It may be a possible explanation for the finding that during a surgical procedure for medial UKA tighter medial joint space was recommended for the prevention of insert dislocation in a mobile-bearing design than in fixed-bearing [23, 24]. Our study used a fixed-bearing medial UKA; the medial joint space was allowed to be looser with a fixed bearing design than with a mobile-bearing design in a previous study [10]. This may explain why the tibial insert thickness was not a predictor in our study. Hopgood et al. [21] suggested that the amount of correction in the tibiofemoral angle could be achieved in fixed-bearing UKA, while they did not measure the mechanical knee axis angle, but anatomical tibiofemoral angle.
In several previous studies [7, 9, 25], it was suggested that post-operative knee alignment after UKA had no influence on clinical outcomes, while in various previous studies [1–6] post-operative knee malalignment could lead to risk of implant failure. For the optimal post-operative knee alignment in UKA, minor varus alignment might provide better results than neutral alignment in medial UKA [8], while several previous studies [6, 12] reported that surgeons should attempt to restore the mechanical axis to the neutral knee alignment during UKA to achieve better function and prevent revision surgery. In a study [14] of the pattern of cartilage loss in neutral, varus, and valgus knees, the medial-to-lateral ratio of femorotibial cartilage loss was 1.4:1 in neutral knees, 3.7:1 in varus knees, and 1:6.0 in valgus knees. From these results, it can be suggested that even in a neutral knee after UKA there may be higher distribution of medial knee joint load. Adduction impulse predominates until 7 degrees of valgus knee alignment from the varus knee [13]. On the basis of these previous results, we aimed to achieve neutral knee alignment during medial UKA surgery and the post-operative malalignment was defined as outside ±3 degrees of neutral HKA angle in our study.
The present study has several strengths. The results were analysed with multivariate logistic regression analysis, which was used to estimate the association between post-operative malalignment in medial UKA and independent risk factors including various clinical and radiographic factors. Most previous studies concerning post-operative alignment in medial UKA examined pre-operative knee mechanical axis, valgus stress radiograph and tibial insert thickness. These studies did not focus on various extra-articular deformities, such as DFVA and TBVA, which were addressed in the present study. We analysed the risk factors to predict post-operative malalignment using multivariate logistic regression to control the confounding variables. With respect to the clinical relevance of the present study, careful attention should be paid during UKA to prevent post-operative malalignment in medial UKA, especially in patients with a high degree of pre-operative DFVA. Although pre-operative TBVA and VgSA were also risk factors for post-operative malalignment, high degree of pre-operative DFVA was identified as the strongest risk factor. Recently, the long-term survivorship after UKA was demonstrated [26], and the indication of UKA has been expanded to knee osteoarthritis with severe varus deformity over 15 degrees and tibiofemoral subluxation [27, 28]. In UKA for severe varus knee, the results of our study may give meaningful clinical information and caution to the operator.
Several limitations were noted. Retrospective data collection and analysis were performed, which could have allowed for patient selection bias and the opportunity for confounding. Although we adjusted for potential confounders, there may have been additional confounders that we did not control. Secondly, the assessment of clinical outcomes according to post-operative alignment was not performed. We performed the analysis of predictors for post-operative malalignment, while the influence of malalignment on functional findings was not analyzed. Further study about the relationship between malalignment and clinical outcomes in fixed-bearing medial UKAs is needed. A third limitation is the low statistical power for several risk factor variables in the post hoc analysis. The study was sufficiently powered to detect pre-operative DFVA as a risk factor with high OR (power = 0.999), while the low OR resulted in limited statistical power for several parameters including BMI and post-operative mLDFA, and may have contributed to limiting the significance of the results.
Conclusions
The overall results suggest that the careful notice should be given to the possibility of post-operative malalignment during medial UKA in patients with a greater varus angle in pre-operative DFVA, TBVA, and valgus stress angle, especially with a greater varus DFVA, which was the strongest predictor for post-operative malalignment.
References
Burnett RS, Nair R, Hall CA, Jacks DA, Pugh L, McAllister MM (2014) Results of the Oxford Phase 3 mobile bearing medial unicompartmental knee arthroplasty from an independent center: 467 knees at a mean 6-year follow-up: analysis of predictors of failure. J Arthroplasty 29(9):193–200
Barbadoro P, Ensini A, Leardini A, d’Amato M, Feliciangeli A, Timoncini A, Amadei F, Belvedere C, Giannini S (2014) Tibial component alignment and risk of loosening in unicompartmental knee arthroplasty: a radiographic and radiostereometric study. Knee Surg Sports Traumatol Arthrosc 22(12):3157–3162
Kim KT, Lee S, Kim TW, Lee JS, Boo KH (2012) The influence of postoperative tibiofemoral alignment on the clinical results of unicompartmental knee arthroplasty. Knee Surg Relat Res 24(2):85–90
Collier MB, Engh CA Jr, McAuley JP, Engh GA (2007) Factors associated with the loss of thickness of polyethylene tibial bearings after knee arthroplasty. J Bone Joint Surg Am 89(6):1306–1314
Kasodekar VB, Yeo SJ, Othman S (2006) Clinical outcome of unicompartmental knee arthroplasty and influence of alignment on prosthesis survival rate. Singap Med J 47(9):796–802
Ridgeway SR, McAuley JP, Ammeen DJ, Engh GA (2002) The effect of alignment of the knee on the outcome of unicompartmental knee replacement. J Bone Joint Surg (Br) 84(3):351–355
Gulati A, Chau R, Simpson DJ, Dodd CA, Gill HS, Murray DW (2009) Influence of component alignment on outcome for unicompartmental knee replacement. Knee 16(3):196–199
Vasso M, Del Regno C, D’Amelio A, Viggiano D, Corona K, Schiavone Panni A (2015) Minor varus alignment provides better results than neutral alignment in medial UKA. Knee 22(2):117–121
Gulati A, Pandit H, Jenkins C, Chau R, Dodd CA, Murray DW (2009) The effect of leg alignment on the outcome of unicompartmental knee replacement. J Bone Joint Surg (Br) 91(4):469–474
Kim SJ, Bae JH, Lim HC (2012) Factors affecting the postoperative limb alignment and clinical outcome after Oxford unicompartmental knee arthroplasty. J Arthroplasty 27(6):1210–1215
Mullaji AB, Shetty GM, Kanna R (2011) Postoperative limb alignment and its determinants after minimally invasive Oxford medial unicompartmental knee arthroplasty. J Arthroplasty 26(6):919–925
John J, Kuiper JH, May PC (2009) Age at follow-up and mechanical axis are good predictors of function after unicompartmental knee arthroplasty. An analysis of patients over 17 years follow-up. Acta Orthop Belg 75(1):45–50
Leitch KM, Birmingham TB, Dunning CE, Giffin JR (2013) Changes in valgus and varus alignment neutralize aberrant frontal plane knee moments in patients with unicompartmental knee osteoarthritis. J Biomech 46(7):1408–1412
Eckstein F, Wirth W, Hudelmaier M, Stein V, Lengfelder V, Cahue S, Marshall M, Prasad P, Sharma L (2008) Patterns of femorotibial cartilage loss in knees with neutral, varus, and valgus alignment. Arthritis Rheum 59(11):1563–1570
Kim JM, Hong SH, Kim JM, Lee BS, Kim DE, Kim KA, Bin SI (2015) Femoral shaft bowing in the coronal plane has more significant effect on the coronal alignment of TKA than proximal or distal variations of femoral shape. Knee Surg Sports Traumatol Arthrosc 23(7):1936–1942
van Raaij TM, Takacs I, Reijman M, Verhaar JA (2009) Varus inclination of the proximal tibia or the distal femur does not influence high tibial osteotomy outcome. Knee Surg Sports Traumatol Arthrosc 17(4):390–395
Moon YW, Kim JG, Han JH, Do KH, Seo JG, Lim HC (2013) Factors correlated with the reducibility of varus deformity in knee osteoarthritis: an analysis using navigation guided TKA. Clin Orthop Surg 5(1):36–43
Kreitz TM, Maltenfort MG, Lonner JH (2015) The valgus stress radiograph does not determine the full extent of correction of deformity prior to medial unicompartmental knee arthroplasty. J Arthroplasty 30(7):1233–1236
Tashiro Y, Matsuda S, Okazaki K, Mizu-Uchi H, Kuwashima U, Iwamoto Y (2014) The coronal alignment after medial unicompartmental knee arthroplasty can be predicted: usefulness of full-length valgus stress radiography for evaluating correctability. Knee Surg Sports Traumatol Arthrosc 22(12):3142–3149
Waldstein W, Bou Monsef J, Buckup J, Boettner F (2013) The value of valgus stress radiographs in the workup for medial unicompartmental arthritis. Clin Orthop Relat Res 471(12):3998–4003
Hopgood P, Martin CP, Rae PJ (2004) The effect of tibial implant size on post-operative alignment following medial unicompartmental knee replacement. Knee 11(5):385–388
Falez F (2014) Knee arthroplasty today. Int Orthop 38(2):221–225
Emerson RH Jr, Hansborough T, Reitman RD, Rosenfeldt W, Higgins LL (2002) Comparison of a mobile with a fixed-bearing unicompartmental knee implant. Clin Orthop Relat Res 404:62–70
Emerson RH Jr, Head WC, Peters PC Jr (1992) Soft-tissue balance and alignment in medial unicompartmental knee arthroplasty. J Bone Joint Surg (Br) 74(6):807–810
Citak M, Dersch K, Kamath AF, Haasper C, Gehrke T, Kendoff D (2014) Common causes of failed unicompartmental knee arthroplasty: a single-centre analysis of four hundred and seventy one cases. Int Orthop 38(5):961–965
Vasso M, Del Regno C, Perisano C, D’Amelio A, Corona K, Schiavone Panni A (2015) Unicompartmental knee arthroplasty is effective: ten year results. Int Orthop. Jul 2 [Epub ahead of print]
Seng CS, Ho DC, Chong HC, Chia SL, Chin PL, Lo NN, Yeo SJ (2014) Outcomes and survivorship of unicondylar knee arthroplasty in patients with severe deformity. Knee Surg Sports Traumatol Arthrosc. 2014 Dec 3 [Epub ahead of print]
Nam D, Khamaisy S, Gladnick BP, Paul S, Pearle AD (2013) Is tibiofemoral subluxation correctable in unicompartmental knee arthroplasty? J Arthroplasty 28(9):1575–1579
Acknowledgments
This study was not supported by any foundation.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ahn, J.H., Kang, H.W., Yang, T.Y. et al. Risk factors of post-operative malalignment in fixed-bearing medial unicompartmental knee arthroplasty. International Orthopaedics (SICOT) 40, 1455–1463 (2016). https://doi.org/10.1007/s00264-015-3014-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3014-1