Abstract
Purpose
Trapezio-metacarpal (TM) joint arthritis is a common cause of pain and functional disability of the hand. The ideal surgical procedure for TM joint osteoarthritis is still controversial. The aim of the current study is to assess the outcome of complete trapezial excision and abductor pollicis longus tendon interposition arthroplasty in the treatment of TM osteoarthritis.
Methods
Twenty patients (16 women and 4 men) were prospectively enrolled in the current study with average age of 51.5 years (36-64). All patients had complete trapezial excision and abductor pollicis longus tendon interposition arthroplasty with minimum follow-up of 24 months.
Results
At final follow-up there was significant improvement as regard pain, range of motion, and functional assessment scores. Pre-operative visual analogue scale (VAS) for pain improved from 6.2 (±1.54) to 1.1 (±0.97), and the average Quick DASH Score improved from 47.6 (±8.81) points pre-operatively to 13.6 (±5.46) points post-operatively. The mean pre-operative Buck-Gramcko score system improved from 21 (±6.2) points to 41.5 (±7). The average post-operative satisfaction score was 9.1(±2.1), with all the patients somewhat satisfied and recommending operation to other patients.
Conclusions
The total trapeziectomy tendinoplasty with suspension and interposition using the abductor pollicis longus is a reliable procedure for the treatment of TMJ osteoarthritis, providing satisfactory functional results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although the trapezio-metacarpal (TM) joint is the second most commonly involved hand joint in osteoarthritis after the distal interphalangeal (DIP) joint, its involvement causes potentially far more significant functional disability secondary to painful, weakened pinch and grip. Women with the disorder outnumber men by a ratio of 10–15:1 [1].
TM arthritis may be confined to the TM joint, or it may involve the pan-trapezial joint complex. The staging system originated by Eaton and Littler [2] described four stages, with stage four indicating additional trapezio-scaphoid arthritis. A stage V has recently been suggested to account for pan-trapezial arthritis [1].
Numerous operative techniques have been described for treating disabling TM arthritis after failure of conservative measures, including arthrodesis [3], trapezial excision alone [4], trapezial excision and ligament reconstruction with tendon interposition (e.g., FCR [5], APL [6]), silicone arthroplasty [7], and total joint replacement arthroplasty [8].
Patients and methods
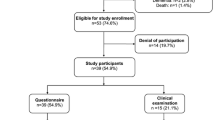
Between February 2010 and October 2011, 25 patients were prospectively enrolled in the current study. Five of them were lost at follow-up and 20 completed the minimum two years follow-up. Inclusion criteria included patients with osteoarthritis of trapezio-metacarpal joint (primary or post traumatic) Eaton and Littler [2] grade II or more, resulting in severe pain located at the base of the thumb limiting the patient activities of daily living. All patients had failed trials of non-operative management for at least three months. We excluded patients with systemic inflammatory disease (rheumatoid arthritis, etc.).
There were 16 women (80 %) and four men (20 %), with average age of 51.5 years (36–64). The dominant hand was involved in 12 patients. All the cases were classified according to the system of Eaton and Littler [2]. There were two patients with grade II, ten patients with grade III, six with grade IV and two with grade V.
All patients signed an informed consent, and the study protocol was accepted by Benha University ethical board committee.
Surgical technique
Wagner’s approach [9] was used for exposure of the first TMC joint. The capsule of the joint was longitudinally incised. The trapezium is then resected by enucleation after complete release of attachment inside the capsule or piecemeal removal using a rongeur, taking care not to damage the joint capsule or flexor carpi radialis (FCR) tendon (Fig. 1). The abductor pollicis longus (APL) tendon was then identified. It is usually composed of two or more slips. The dorsal one is dissected and cut proximally approximately 3.5 cm from the insertion. In three patients, a single APL tendon had a large insertion which encompasses both the metacarpal base and the thenar fascia. In such cases, the single tendon was split by a lancet and dissected from distal to proximal, until reaching the distal exit of the first extensor compartment; the dorsal slip was then used as the usual one. We did not record any difference in the outcome with the rest of patients.
The slip is looped around FCR from behind to forward two to three times while maintaining traction on the thumb to preserve trapezial space height. It is then sutured under tension to the palmer slip of APL using non absorbable sutures (Fig. 2). The rolled lope occupy the position of trapezium acting as spacer maintaining thumb height, while its suspensory effect reducing the sublaxed first metacarpal volarly and supporting the base of first metacarpal like a hammock. Skin is then closed with mean operative time 38 (±10.2) min.
After skin closure, a thumb slap was used for two weeks and replaced by disposable thumb support for another three weeks to protect the tendinoplasty.
Assessment of the patients
Each patient was assessed pre-operatively and post-operatively at final follow-up for pain using a visual analogue scale (VAS) composed of ten points, where 0 indicates no pain and 10 the maximum unbearable pain, Quick DASH questionnaire, range of motion, grip strength, Buck-Gramcko score, and overall satisfaction using a ten point scale, where 0 is totally dissatisfied and 10 is completely satisfied. Opposition was assessed by Kapandji score [10], and grip strength by using a dynamometer.
Results
The average follow-up was 24 months ranging from 18 to 35 months (Fig. 3). The mean preoperative VAS for pain was 6.2 (±1.54). This improved significantly post-operatively to 1.1 (±0.97) (p value <0.0001).
The average pre-operative thumb abduction was (17.25 ± 6.38) which improved post-operatively to an average of (26.5 ± 7.45). The mean pre-operative Kapandji opposition score was 3.2 (±1.44) that increased significantly to 6.9 (±1.25) post-operatively (p value = 0.001).
Grip strength showed improvement from 13 (±1.25) to 13.3 (±1.1); however, this improvement was not statistically significant.
The average Quick DASH Score markedly decreased (improved) from 47.6 (±8.81) point pre-operatively to 13.6 (±5.46) point post-operatively. The mean pre-operative Buck-Gramcko score was 21 (±6.2) points. This increased post-operatively to 41.5 (±7).
The average pos-toperative satisfaction score was 9.1 (±2.1), with all the patients somewhat satisfied and recommend operation to other patients.
Discussion
There are still controversies about the best surgical procedure for the management of thumb TM joint osteoarthritis. Although TM arthrodesis provides a stable thumb, relieves pain, and possibly increases strength; however, arthrodesis reduces manual dexterity, requires prolonged immobilization, and is associated with higher rate of complications and re-operation due to nonunion or trapezio-scaphoid arthritis [11].
There appears to be consensus that removal of the arthritic surface of the trapezium leads to successful outcomes. Trapezoid excision and spacer ligamentoplasties showed overall good results in terms of pain relief and restoration of function [12]. They have been reported to achieve a better range-of motion in comparison with fusion; a lower rate of complications when compared with total joint arthroplasty; a lower percentage of thumb “sinking” in respect with simple excision [12, 13].
Many surgical procedures were described to reconstruct the anterior oblique ligament with the most popular described by Pellegrini and Burton [5] using the FCR tendon to reconstruct the ligament and as a spacer after trapeziectomy. However the use of the FCR for basal joint reconstruction has been associated with weakness in wrist flexion and torsion [5, 14].
Our results matched the results obtained by other series of FCR [15] and APL ligamentoplasties [16–18] in regard of postoperative pain, range of motion, or functional outcome scores as shown in Table 1.
Systematic review studies showed that more complex or extensive procedures were found to have a higher complication rate. In our study we tried to simplify the procedure of trapeziectomy and ligamentoplasty using slip of the APL to perform tenodesis, preventing subluxation and acting at the same time as a spacer against collapse, in a rapid and easy way avoiding creating difficult bone tunnels and avoiding using any k wires, which may be a source of discomfort and pin tract infection as in the technique of Kochevar et al. [13] or extensive difficult dissection as done in case series of Rocchi et al. [18]; with an average operative time of about half an hour.
References
Tomaino MM, King J, Leit M (2005) Thumb basal joint arthritis. In: Green DP, Hotchkiss RN, Pederson WC, Wolfe SW (eds) Green’s operative hand surgery, vol 1. Churchill Livingstone, New York
Eaton R, Littler J (1973) Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg 55:1655–1666
Muller G (1949) Arthrodesis of the trapezio-metacarpal joint for osteoarthritis. J Bone Joint Surg 31:540–542
Murley A (1960) Excision of the trapezium in osteoarthritis of the first carpo-metacarpal joint. J Bone Joint Surg 42:502–507
Burton R, Pellegrini V (1986) Surgical management of basal joint arthritis of the thumb: part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg [Am] 11:324–332
Thompson J (1986) Surgical treatment of trapeziometacarpal arthrosis. Adv Orthop Surg 10:105–120
Swanson A (1972) Disabling arthritis at the base of the thumb. Treatment by resection of the trapezium and flexible (silicone) implant arthroplasty. J Bone Joint Surg 54:456–471
Lemoine S, Wavreille G, Alnot JY, Fontaine C, Chantelot C (2009) Second generation GUEPAR total arthroplasty of the thumb basal joint: 50 months follow-up in 84 cases. Orthop Traumatol Surg Res 95:63–69
Wagner C (1950) Methods of treatment of Bennett’s fracture-dislocation. Am J Surg 80:230–231
Kapandji A (1986) Cotation clinique de l’opposition et de la contreopposition du pouce. Ann Chir Main 5:67–73
Mureau M, Rademaker R, Verhaar J, Hovius S (2011) Tendon interposition arthroplasty versus arthrodesis for the treatment of trapeziometacarpal arthritis: a retrospective comparative follow-up study. J Hand Surg [Am] 26(5):869–876
Haase S, Chung K (2011) An evidence-based approach to treating thumb carpometacarpal joint arthritis. Plast Reconstr Surg 127(2):918–925
Kochevar AJ, Adham CN, Adham MN, Angel MF, Walkinshaw MD (2011) Thumb basal joint arthroplasty using abductor pollicis longus tendon: an average 5.5-year follow-Up. J Hand Surg Am 36(8):1326–1332. doi:10.1016/j.jhsa.2011.05.026
Naidu S, Poole B, Horne A (2006) Entire flexor carpi radialis tendon harvest for thumb carpometacarpal arthroplasty alters wrist kinetics. J Hand Surg [Am] 31:1171–1175
Basar H, Basar B, Erol B, Tetik C (2012) Ligament reconstruction and tendon interposition arthroplasty of the trapeziometacarpal joint with the use of the full thickness of the flexor carpi radialis tendon. Chir Main 31:331–336
Avisar E, Elvey M, Wasrbrout Z, Aghasi M (2013) Long-term follow-up of trapeziectomy with abductor pollicis longus tendon interposition arthroplasty for osteoarthritis of the thumb carpometacarpal joint. J Orthop 10:59–64
Ferrière S, Mansat P, Rongières M, Mansat M, Bonnevialle P (2010) Total trapeziectomy with suspension and interposition tendinoplasty for trapeziometacarpal osteoarthrisis: results at 6.5 years average follow-up. Chir Main 29:16–22
Rocchi L, Merolli A, Cotroneo C, Morini A, Brunelli F, Catalano F (2011) Abductor pollicis longus hemitendon looping around the first intermetacarpal ligament as interposition following trapeziectomy: a one-year follow-up study. Orthop Traumat Surg Res 97(7):726–733. doi:10.1016/j.otsr.2011.05.008
Conflict of interest
The authors declare that they have no conflicts of interest. They did not receive any funding or grant from any institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Singer, M.S., Kandel, W.A. Slip abductor pollicis longus suspension tendinoplasty for management of trapezio-metacarpal joint osteoarthritis. International Orthopaedics (SICOT) 40, 765–769 (2016). https://doi.org/10.1007/s00264-015-2904-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2904-6