Abstract
Purpose
Revision hip arthroplasty using a modular tapered design gives the possibility for customising the prostheses to the individual anatomy intra-operatively. The success of this kind of surgery is still controversial due to the relative lack of medium- to long-term follow-up. Therefore we analysed the clinical and radiological outcome of the modular MRP-TITAN stem with diaphyseal fixation in revision hip surgery.
Methods
In this retrospective study we included 136 consecutive patients with MRP-TITAN stem implanted during revision hip arthroplasty. The average follow-up was 55 months. For clinical evaluation we used the Harris Hip Score and the Merle d’Aubigné and Postel score. The health-related quality of life was determined with the visual analogue pain scale.
Results
The surgeries were performed 109 months after primary total hip arthroplasty on average. The main indications for the MRP-TITAN revision stem were aseptic loosening, infection, and periprosthetic fracture. In the clinical outcome, patients achieved 75.1 points in the Harris Hip Score and 14.4 points in the Merle d’Aubigné and Postel Score. Mean level of persisting pain was 0.7 (VAS). The overall survival of the MRP stem in revision hip arthroplasty revealed 85.6 % survival at 9.75 years’ follow-up with a repeat revision rate of 6.8 %.
Conclusions
Performing revision hip arthroplasty using the MRP-TITAN stem revealed a good clinical outcome. There is a tendency for better results in comparison with the information given in literature for cementless modular revision stems including a lower rate in re-revisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cementless modular revision stems are widely used in revision hip arthroplasty with promising results in medium- and long-term follow-up [1]. In complex revision surgery the advantages of stem modularity are the greater variability for restoration of the leg length, femoral offset, femoral anteversion and soft tissue tension [2, 3]. The proper reconstruction of the anatomic centre of rotation and press-fit bone fixation of the revision stem are essential for long-term outcome [4]. The individual intra-operative anatomical situation can be addressed by modular-designed prosthesis and allows nearly physiological joint reconstruction [4]. In difficult anatomical findings the use of a distal diaphyseal press-fit stem provides more options than non-modular revision stems [2]. The cementless distal diaphyseal fixating modular MRP-TITAN revision stem (Fig. 1) has excellent short- and long-term results in a number of studies, with low mechanical failure rates and high overall survival rates. Most of the reports with higher patient numbers are multicentre-designed, have different exclusion criteria and use different stem lengths with or without additional distal fixation [3, 5, 6]. Because of these shortcomings, we investigated the clinical and radiological outcomes, of femoral revision arthroplasty with the 200-mm curved MRP-TITAN stem in a retrospective, monocentric and consecutive study.
Patients and methods
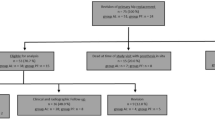
From our own database, we identified 136 patients who underwent a femoral revision arthroplasty using a 200-mm curved MRP-TITAN stem in our institution during the years 2005–2011. Twenty-three patients were lost to follow-up (16.9 %) and 24 patients died from non-implant-related reasons with the femoral stem not revised (17.6 %). Of the 89 patients analysed, 43 were women and 46 men, with a mean age of 72.3 (min. 52, max. 95) years. The major diagnosis leading to indicate total hip arthroplasty (THA) was primary osteoarthritis in 78 % of the cases, post-traumatic osteoarthritis in 4 %, and others in 18 % of the cases. Stem revision was performed on average 109 (min. one, max. 420) months after primary THA. When necessary, cup revision, liner exchange or synovectomy was performed additionally. In all cases we used a lateral approach with lateral skin incision and excision of the old scar. Mean follow-up time was 55 (min. 24, max. 117) months.
Clinical assessments included determination of the Harris Hip Score and the Merle d’Aubigné and Postel Score. The health-related quality of life was determined with the visual analogue pain scale (VAS). Pre-operative and postoperative standard radiographs were available for all patients. The radiographs were analysed for signs of implant loosening regarding the criteria by Kavanagh and Fitzgerald [7] and periprosthetic radiolucencies according to Gruen in zones 1–7. Pre-operative femoral defects were classified according to the paper of Pak et al. [8]. We defined revision of an MRP-TITAN stem as a failure when patients underwent re-revision surgery for any reason.
Statistical analysis
The main end point of this study was the overall survival after revision hip arthroplasty implanting the MRP-TITAN stem, and univariate analysis was performed using the Kaplan-Meier test and the log-rank test, respectively.
We compared the global range of motion preoperative to postoperative by using t-test for paired data. A p value of <0.05 was considered to be statistically significant. For statistical analysis the SPSS 15.0 program (SPSS, Chicago, IL, USA) was used.
Results
The main indications for revision of the primary femoral implant were aseptic loosening (48 %), periprosthetic joint infection with two-stage treatment using an articulating antibiotics-impregnated cement spacer (38 %), periprosthetic fracture (10 %) (Fig. 2), and fracture of the primary THA stem (2 %). Preoperative femoral defect classification revealed a Paprosky I defect in 9.1 % of the cases, Paprosky II A in 38.6 %, Paprosky II B in 18.1 %, and Paprosky II C in 10.3 %. Larger femoral bone defects were found in 15.8 % of the patients according to Paprosky III A and 8.1 % with a Paprosky III B defect. The type of failure and the pre-operative defined bone defect revealed no significant difference in all parameters investigated.
In the clinical outcome patients achieved 75.1 points (min. 18, max. 100) in the Harris Hip Score and 14.4 points (min. 5, max. 18) in the Merle d’Aubigné and Postel Score. Mean level of persisting pain was 0.7 (VAS). The rate of patients without any pain revealed 89.7 %. Patients were satisfied in 88.4 % with their results, 10.1 % were partly satisfied and only 1.5 % were not satisfied according to the patients’ subjective satisfaction consideration.
In the radiographic evaluation, 96 % of the cases had stable stem ingrowth without any radiolucencies or stem migration. In Gruen zone 1 only 4 % showed a radiolucency of less than 1 mm without any hints for aseptic loosening. According to Brookers’ classification, 61.4 % of the patients revealed no periarticular ossifications, 26.1 % had Brooker type I, 5.7 % Brooker type II and 6.8 % Brooker type III ossifications [9].
The global range of motion was significantly increased in the postoperative clinical follow-up compared to the preoperative status (Fig. 3).
The calculated overall survival for using the MRP-TITAN stem in revision hip arthroplasty revealed 85.6 % survival at 9.75 years’ follow-up (Fig. 4). Six out of 89 (6.8 %) patients were considered failures of revision with the MRP-TITAN due to re-revision. Reasons for repeated revision were early postoperative superficial infection (3), treated with head and inlay exchange, meticulous debridement and antibiotic medication for four weeks postoperatively. Two patients were revised because of recurrent dislocation with head and inlay exchange and one patient with fascia defect was treated with secondary suture. None of all the patients had an exchange of the MRP-TITAN stem.
Discussion
Revision hip arthroplasty using a diaphyseal cementless fixating stem is a frequently performed revision procedure with very different outcome reports. Recent papers revealed rates of aseptic loosening between 4 and 16 % using the modular Revitan stem, Wagner stem and other porous-coated stems [1, 10–13]. In contrast, our revision rate using the MRP-TITAN stem is 6.8 %, with a Kaplan-Meier survival rate of 85.6 % after 9.75 years. These promising results were supported by findings of Wirtz et al. [5], showing a 15-year survival of 85 %, with a revision rate of 6 %. Many authors reported up to 10 % axial migration with subsidence as the main reason for revision stem failure [1]. The subsidence rate for the MRP stem is lower with a mean of ca. 4 % migrations [5, 14, 15]. Nevertheless, we could not find any stem subsidence or axial migration after a mean follow-up of 55 months. The main surgical factor to prevent any migration or subsidence is a perfect diaphyseal contact area of the implant to the bone over a distance of 70 mm [6] for the MRP stem and 30 mm for the Revitan stem. Compared with the clinical results of the MRP-TITAN stem, an increased failure was reported for the Revitan stem [1]. The specific geometry of the MRP-TITAN with longitudinal rips, a rough surface and a taper-shape bowed design seem to be the major key for the very encouraging outcome results. A study from Gravius et al. [16] reported no corrosion or fretting at all modular interfaces using the MRP stem because of a specific manufacturing process of the Morse taper junctions [17]. These data were supported by the findings of Wirtz et al. [5]. Also, we could not detect any osteolysis around the modular connections of the stem.
In the clinical outcome, our patients revealed very promising results with a Harris Hip score of 75.1 points and a Merle d’Aubigné and Postel score of 14.4 points. Different single and multicentre studies reported slightly lower results for the Harris Hip score in a larger patient cohort with 70–71.4 points, respectively, using the MRP stem [6, 15]. In contrast, Wirtz et al. [5] showed a Harris Hip score of 79 points in a large multicentre study with different designs of the MRP-TITAN stem. Our findings regarding the Merle d’Aubigné and Postel score are supported by 15.2 points in this score published by Schuh et al. [14]. Recurrent dislocation is one of the common problems after revision THA. In our study, we found a rate of 2.3 %. Wirtz et al. [18] reported in their multicentre study a rate of 4–12 % for the MRP stem equivalent to dislocations rates to other femoral stems [10, 19]. The persisting pain level after revision to an MRP-TITAN stem was 0.7 in our series. Van Diemen et al. [20] reported a level of 2.68 in the VAS using a modular femoral revision stem. The excellent outcome concerning pain supports the potential advantage of the MRP stem to properly reconstruct the hip [5].
We acknowledge the shortcomings of our study, including the design as a retrospective and descriptive study without a control group. Nonetheless, this is a large and monocentric study elucidating important issues related to revision hip surgery, and emphasises outcome and treatment in a demanding operative situation.
Conclusions
To the best of our knowledge, we are presenting a consecutive, monocentric and retrospective study with the largest sample sizes presently published using the 200-mm curved MRP-TITAN revision stem for using the advantages of a modular design with diaphyseal fixation. The MRP-TITAN stem is a promising option for patients with failed THA and Paprosky type I-III femoral defects.
References
Fink B, Grossmann A, Schubring S, Schulz MS, Fuerst M (2009) Short-term results of hip revisions with a curved cementless modular stem in association with the surgical approach. Arch Orthop Trauma Surg 129:65–73. doi:10.1007/s00402-008-0617-7
Berry DJ (2002) Femoral revision: distal fixation with fluted, tapered grit-blasted stems. J Arthroplast 17:142–146
Mumme T, Muller-Rath R, Weisskopf M, Andereya S, Neuss M, Wirtz DC (2004) The cement-free modular revision prosthesis MRP-hip revision stem prosthesis in clinical follow-up. Z Orthop Grenzgeb 142:314–321. doi:10.1055/s-2004-822795
Gravius S, Randau T, Wirtz DC (2011) What can be done when hip prostheses fail?:new trends in revision endoprosthetics. Orthopade 40:1084–1094. doi:10.1007/s00132-011-1844-0
Wirtz DC, Gravius S, Ascherl R, Forst R, Noeth U, Maus UM, Zeiler G, Moritz CD (2014) Uncemented femoral revision arthroplasty using a modular tapered, fluted titanium stem. Acta Orthop 85:562–569. doi:10.3109/17453674.2014.958809
Mumme T, Muller-Rath R, Andereya S, Wirtz DC (2007) Uncemented femoral revision arthroplasty using the modular revision prosthesis MRP-TITAN revision stem. Oper Orthop Traumatol 19:56–77. doi:10.1007/s00064-007-1195-5
Kavanagh BF, Fitzgerald RH Jr (1985) Clinical and roentgenographic assessment of total hip arthroplasty. A new hip score. Clin Orthop Relat Res (193):133–140
Pak JH, Paprosky WG, Jablonsky WS, Lawrence JM (1993) Femoral strut allografts in cementless revision total hip arthroplasty. Clin Orthop Relat Res (295):172–178
Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55:1629–1632
Wagner H, Wagner M (1993) Femur revision prosthesis. Z Orthop Grenzgeb 131:574–577. doi:10.1055/s-2008-1040074
Bohm P, Bischel O (2001) Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Joint Surg Am 83-A:1023–1031
Randhawa K, Hossain FS, Smith B, Mauffrey C, Lawrence T (2009) A prospective study of hip revision surgery using the Exeter long-stem prosthesis: function, subsidence, and complications for 57 patients. J Orthop Traumatol 10:159–165. doi:10.1007/s10195-009-0068-0
Kim YH, Park JW, Kim JS (2013) Behaviour of the ultra-short anatomic cementless femoral stem in young and elderly patients. Int Orthop 37:2323–2330. doi:10.1007/s00264-013-2044-9
Schuh A, Werber S, Holzwarth U, Zeiler G (2004) Cementless modular hip revision arthroplasty using the MRP Titan Revision Stem: outcome of 79 hips after an average of 4 years’ follow-up. Arch Orthop Trauma Surg 124:306–309. doi:10.1007/s00402-004-0656-7
Wimmer MD, Randau TM, Deml MC, Ascherl R, Noth U, Forst R, Gravius N, Wirtz D, Gravius S (2013) Impaction grafting in the femur in cementless modular revision total hip arthroplasty: a descriptive outcome analysis of 243 cases with the MRP-TITAN revision implant. BMC Musculoskelet Disord 14:19. doi:10.1186/1471-2474-14-19
Gravius S, Mumme T, Andereya S, Maus U, Muller-Rath R, Wirtz DC (2007) The morse taper junction in modular revision hip replacement. Z Orthop Unfallchirurgie 145:157–160. doi:10.1055/s-2007-965182
Hernigou P, Queinnec S, Flouzat Lachaniette CH (2013) One hundred and fifty years of history of the Morse taper: from Stephen A. Morse in 1864 to complications related to modularity in hip arthroplasty. Int Orthop 37:2081–2088. doi:10.1007/s00264-013-1927-0
Wirtz DC, Heller KD, Holzwarth U, Siebert C, Pitto RP, Zeiler G, Blencke BA, Forst R (2000) A modular femoral implant for uncemented stem revision in THR. Int Orthop 24:134–138
Gutierrez Del Alamo J, Garcia-Cimbrelo E, Castellanos V, Gil-Garay E (2007) Radiographic bone regeneration and clinical outcome with the Wagner SL revision stem: a 5-year to 12-year follow-up study. J Arthroplast 22:515–524. doi:10.1016/j.arth.2006.04.029
van Diemen MP, Colen S, Dalemans AA, Stuyck J, Mulier M (2013) Two-stage revision of an infected total hip arthroplasty: a follow-up of 136 patients. Hip Int 23:445–450. doi:10.5301/hipint.5000049
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hoberg, M., Konrads, C., Engelien, J. et al. Outcome of a modular tapered uncemented titanium femoral stem in revision hip arthroplasty. International Orthopaedics (SICOT) 39, 1709–1713 (2015). https://doi.org/10.1007/s00264-015-2699-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2699-5