Abstract
Purpose
Our aim was to evaluate quality of life (QoL) and functional outcome of patients with tibial nonunions after completion of surgical treatment with an average follow-up of five years.
Methods
The following data of 64 patients were retrospectively evaluated: fracture type, type and duration of surgical therapy, range of motion of the knee and ankle and American Orthopaedic Foot and Ankle Society (AOFAS) score. QoL was evaluated with the Short-Form Health Survey (SF-36) questionnaire; pain intensity, patient satisfaction and impairments of daily, professional and sport activities with a ten point visual analogue scale.
Results
QoL, even in cases with successfully completed treatment, was significantly reduced compared with the normal general population. Pain intensity and limited ankle dorsal extension, despite the absence of intra-articular fractures, were significantly correlated with inferior QoL.
Conclusions
This study emphasises the long-term negative impact of tibial nonunions on patient QoL, even after successful surgical treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Skeletal nonunions represent a major problem for patients, the treating orthopaedic surgeon, the public health system and society in general. Long treatment duration, high costs, and work and social implications for these patients can complicate fracture treatment [1, 2]. Nonunions are a possible complication in up to 5 % of all fractures, but the tibia represents the most common site for the development of nonunions [3].
Since managing nonunions can be a therapeutic challenge, a series of treatment options are thoroughly described in the literature [3–6]. The treatment regime aims at successful bone healing and adequate soft-tissue coverage, which may be achieved by a great variety of interventions [7–9]. The short- and midterm surgical outcome is being evaluated in most cases in terms of bone union, range of motion (ROM), infection rate and loss of strength. Several studies show the effectiveness of available treatment options in terms of outcome [10–12]. Nevertheless, over the long term, a certain degree of disability in terms of ROM, persistent pain and other functional limitations can remain, even in cases in which the primary treatment goal has been achieved.
While the existing treatment options and their midterm outcome are thoroughly described in the literature, limited data exist on the long-term quality of life (QoL) and functional outcome of patients after treatment for tibial nonunions.
The aim of our study was to evaluate the long-term health-related QoL (HR-QoL) of patients with tibial nonunions after completion of treatment and to evaluate their functional outcomes.
Methods
All patients with extra-articular tibial nonunions who were treated operatively in our institution over a ten year period (2002–2012) and whose treatment was considered completed were included and retrospectively evaluated. Inclusion criteria were patients with completed successful treatment who were older than 18 years and contractually capable. Completed successful treatment was defined as full bone consolidation with uneventful soft-tissue healing. A total of 72 patients with tibial nonunions were identified; 64 entered the study. For the remaining eight patients, treatment was either defined as not successful [persistent and constant soft-tissue fistula (n = 2), amputation (n = 4)] or not completed [no wish for further medical treatment (n = 2)]. Mean patient age was 42.8 [standard deviation (SD) 15.6; range 19–78) years, with a mean body mass index (BMI) of 26.1 (SD 4.1). The majority of patients were men [n = 49 (76.5 %) vs n = 15 (23.6 %)], with most being nonsmokers (n = 38; 59.3 %). Mean follow-up was 61.2 (SD 28.9; range 15–117) months. Nonunions were infectious in 30 cases (46.9 %), atrophic in 19 (29.7 %) and hypertrophic in 15 (23.4 %). The majority of fractures were initially open (56.3 %). An initial nerve lesion was present in four cases (6.3 %). The most common mechanisms of injury were motor vehicle accidents (37.6 %), falls from a significant height (15.6 %), falls from a standing height (14.1 %) and sports injuries (14.1 %). Most patients (n = 38; 59.4 %) were initially treated in another hospital and were then referred to our institute for further treatment. Left and right sides were equally affected. The following parameters were analysed: fracture classification according to the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA), implant initially used, type of osteosynthesis used to treat the nonunion, number of surgeries, duration of nonunion therapy, application of cancellous bone graft (autologous/allogenic), additional use of recombinant growth factor [bone morphogenetic protein (BMP)], soft-tissue coverage according to the reconstructive ladder, amputation, involved bacteria in cases of infectious nonunions, type and duration of antibiotic treatment and leg-length discrepancy. Knee and ankle-joint ROM and functional status of the ankle [American Orthopaedic Foot and Ankle Society (AOFAS) score; 0–100 points] was recorded. HR-QoL was evaluated using the Short-Form-36 Health Survey (SF-36) [13, 14]. Pain intensity, patient satisfaction with surgical outcome and overall treatment, as well as impared activities of daily living and of job or sports were further assessed using a the ten point visual analogue scale (VAS).
Continuous variables are expressed as mean ± SD and categorical variables as percentages (%). The Kolmogorov–Smirnov test was used to assess normality. For parametric variables, Student’s t test was used to compare groups; for nonparametric variables, the Mann–Whitney test was used. Differences for categorical variables were assessed using the χ2 or Fisher’s exact test between groups. Correlations were examined with either the Pearson product moment correlation coefficient or Spearman’s rank correlation coefficient. Differences were considered to be statistically significant if the null hypothesis could be rejected with >95 % confidence (p < 0.05).
Results
Surgical characteristics
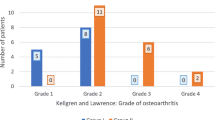
Fracture classification according to AO/OTA is depicted in Table 1. The most common initial surgical treatment was open reduction and internal fixation (ORIF) with plate osteosynthesis (n = 34/ 53.1 %), followed by clamp and rod internal fixation (CRIF) and intramedullary (IM) nailing (n = 28; 43.7 %). The final surgical treatments for nonunions were Ilizarov external fixator (n = 24; 37.5 %), plate osteosynthesis (n = 24; 37.5 %), IM nailing (n = 10/15.6 %) and debridement of the nonunion site with additional bone grafting but without interchanging fixation type (n = 6; 9.4 %). The mean number of surgeries was 4.85 (SD 4.8), with a mean therapy duration of 2.69 (SD 1.9) years—significantly longer for the infectious nonunion group [mean 3 (SD 1) years; p < 0.05]; mean number of operations was eight vs. three in the other groups; p < 0.05). In 40 cases (62.5 %), cancellous bone grafting was performed (autologous n = 28; 43.8 %; allogenic n = 12; 18.8 %), from which 22 cases (34.4 %) received additional application of growth factors (BMPs). In 30 cases (47 %), surgical soft-tissue coverage had to be performed (Meshgraft n = 17; 26.6 %; pedicled muscle flap n = 13; 20.3 %). The need for soft-tissue coverage was significantly higher for patients with infectious nonunions (p < 0.05), in which the most commonly involved bacteria were Staphylococcus aureus and S. epidermidis; in most cases, patients were treated with a combination of amoxicillin/sulbactam for a mean of 3.5 (SD 12.7) months.
Functional outcome
Mean leg-length discrepancy of the affected lower extremity was −1.45 cm (SD 0.7), mean knee flexion and extension was 117.5° (SD 21.7) and 5° (SD 3.3), respectively, and mean ankle dorsal extension and plantar flexion was 9.75° (SD 8.8) and 26° (SD 17), respectively. Mean AOFAS score was 74.9 points (SD 21). Patients with infectious nonunions showed the lowest mean AOFAS scores [68 points (SD 21)] compared with patients with atrophic [76 points (SD 13)] and hypertrophic [87 points (SD 25)] nonunions. However, these differences were not statistically significant.
Quality of life and patient satisfaction
The evaluation of HR-QoL issues in terms of the SF-36 questionnaire were compared to the age-matched (45–65 years), normal general population (Table 2) [14]; the study population showed statistically significantly inferior values. Mean pain intensity according to the VAS was 2.8 (SD 2.3) points, and mean VAS for patient satisfaction with the surgical outcome was 8.2 (SD 2.7) points and with overall treatment 8.2 (SD 2.4) points. Mean VAS for impairment in activities of daily living and professional and sport activities were 4 (SD 3.2) and 4.8 (SD 3.4) points, respectively.
Highly significant negative correlations (p < 0.001) were observed between pain intensity and all subgroups of the SF-36 questionnaire and with AOFAS and VAS scores for patient satisfaction and impairments in daily living and professional and sport activities. Additionally, a positive correlation between the degree of dorsal extension in the ankle and general health SF-36 subgroup was observed (rho 0.461; p = 0.035). SF-36 scores also showed negative correlations between overall therapy duration and patient satisfaction with surgical outcome (rho −0.448; p = 0.003), physical functioning (rho −0.349; p = 0.04) and role limitations due to emotional problems (rho −0.328; p = 0.032) (Table 3).
Discussion
Treating tibial nonunions is a therapeutic challenge for the orthopaedic surgeon. Several treatment options have been described in the literature, with rigid fixation and bone grafting being considered the gold standard [3, 4, 15]. By those means, bone union and adequate soft-tissue coverage can be achieved in the majority of cases, even in cases of infectious nonunions [2, 10, 16–18]. However, treatment is often highly time and resource consuming [19]. This study shows the long-term detrimental effects of tibial nonunions on patient QoL, even in cases of completed surgical treatment with supposedly successful outcome in terms of bone union and soft-tissue coverage. QoL of those patients was significantly inferior compared with the age-adjusted normal population [14]. VAS evaluation showed relatively mild pain, with acceptable patient satisfaction in terms of surgical outcome and overall treatment. Nevertheless, professional and sport activities were affected in everyday life for the majority of patients.
To our knowledge, this is the first study that evaluates the long-term effect of tibial nonunions on patient QoL at a mean follow-up of five years after completion of therapy. Every aspect of the QoL of the study population was decreased, as evaluated by the SF-36. Physical health-related and emotional problems were the main factors leading to the reduction in everyday QoL. Overall treatment duration correlated with lower patient satisfaction and increased limitations due to physical functioning and emotional problems. However, pain intensity seemed to be the main factor that correlated with decreased QoL. These results are in accordance with previous studies: Brinker et al. showed the detrimental effects on HR-QoL of tibial nonunions during treatment [11]. In a subpopulation of older patients treated with Ilizarov external fixation, there was a midterm improvement in QoL after completion of therapy; however, scores were still inferior compared with the normal population [20]. Zeckey et al. observed a deterioration in patient QoL after completed treatment of tibial nonunions [12], but the length of follow-up was not reported. Bowen et al. reported similar results to results of our study in a small population (eight patients) of infectious tibial nonunions [21].
While in our population knee ROM was not significantly affected, a certain limitation was observed in patient mobility in the ankle joint. Limitation of the dorsal extension in the ankle showed a significant negative correlation with general health, as evaluated with the SF-36. The decreased AOFAS scores confirmed limitations in ankle movement, even though no patient with intra-articular injuries was included in the study. Additionally, AOFAS score correlated with patient satisfaction, impairments of daily living and impairments associated with professional and sport activities, further emphasising the importance of the ankle joint for restoration of activities of activities of daily living. Shahid et al. reported higher AOFAS scores in the short-term follow-up compared with our study population [10]. This could be attributed to the lower number of surgeries and shorter overall treatment duration and follow-up.
Additionally, limitation in dorsal extension of the ankle further correlated with limitation of activities of daily living and with general health as assessed using the SF-36. These results emphasise the fact that bone union in combination with successful soft-tissue coverage should be the primary goal in treating such patients, despite the fact that this could result in long treatment duration and repeated surgeries. Moreover, limitation in ankle-joint ROM, possibly resulting from immobilisation and scar tissue formation, need to be addressed during postoperative care. Our patients showed a mean dorsal extension in the ankle of <10°. This seems to be a major limitation for everyday living, as simple activities, such as stair climbing and walking on uneven surfaces, is significantly adversely affected.
In conclusion, our study emphasises the long-term negative impact of tibial nonunions on patient HR-QoL, even in cases of successful surgical treatment. While the goal of treatment still is bony union and soft-tissue coverage, the importance of the initial treatment of tibia fractures, also aimed at reducing the risk of nonunion, should be a crucial part of the treatment strategy. Figs. 1 and 2
Health-related quality of life (HR-QoL) as evaluated with the Short-Form Health Questionnaire (SF-36) of patients, and the general normal population aged 45–65 years old. Study population QoL was significantly inferior, with the exception of pain. I Physical functioning, II role limitations due to physical health, III role limitations due to emotional problems, IV energy/fatigue, V emotional well-being, VI social functioning, VII pain, VIII general health
a Initial X-rays of a male patient, 50 years old, with an open tibia fracture of Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) type 42B3; b treatment with intramedullary (IM) nailing and open reduction and internal fixation (ORIF) of the fibula five days after initial treatent with external fixator (X-rays not shown); c dynamization of IM nailing due to delayed healing five months after treatment; d revision of the osteosynthesis 18 months after trauma, with nail removal, debridement, autologous cancellous bone graft, bone morphogenic protein (BMP)-7 application and plate and lag-screw osteosynthesis; d successful healing two years after trauma
References
Giannoudis PV, Harwood PJ, Kontakis G, Allami M, Macdonald D, Kay SP, Kind P (2009) Long-term quality of life in trauma patients following the full spectrum of tibial injury (fasciotomy, closed fracture, grade IIIB/IIIC open fracture and amputation). Injury 40(2):213–219. doi:10.1016/j.injury.2008.05.024
Pecina M, Haspl M, Jelic M, Vukicevic S (2003) Repair of a resistant tibial nonunion with a recombinant bone morphogenetic protein-7 (rh-BMP-7). Int Orthop 27(5):320–321. doi:10.1007/s00264-003-0475-4
Pneumaticos SG, Panteli M, Triantafyllopoulos GK, Papakostidis C, Giannoudis PV (2014) Management and outcome of diaphyseal aseptic nonunions of the lower limb: a systematic review. Surgeon 12(3):166–175. doi:10.1016/j.surge.2013.10.007
Said GZ, El-Sharkawi MM, Said HG, Refai OA (2011) Fibula-pro-tibia in plating tibial nonunions. Int Orthop 35(11):1713–1718. doi:10.1007/s00264-011-1211-0
Moghaddam A, Elleser C, Biglari B, Wentzensen A, Zimmermann G (2010) Clinical application of BMP 7 in long bone nonunions. Arch Orthop Trauma Surg 130(1):71–76. doi:10.1007/s00402-009-0982-x
Wu CC, Lee ZL (2008) Speeded gradual lengthening and secondary angled blade plate stabilisation for proximal tibial shaft nonunion with shortening. Int Orthop 32(5):693–696. doi:10.1007/s00264-007-0370-5
Mechrefe AP, Koh EY, Trafton PG, DiGiovanni CW (2006) Tibial nonunion. Foot Ankle Clin 11(1):1–18. doi:10.1016/j.fcl.2005.12.003, vii
Vukicevic S, Oppermann H, Verbanac D, Jankolija M, Popek I, Curak J, Brkljacic J, Pauk M, Erjavec I, Francetic I, Dumic-Cule I, Jelic M, Durdevic D, Vlahovic T, Novak R, Kufner V, Bordukalo Niksic T, Kozlovic M, Banic Tomisic Z, Bubic-Spoljar J, Bastalic I, Vikic-Topic S, Peric M, Pecina M, Grgurevic L (2014) The clinical use of bone morphogenetic proteins revisited: a novel biocompatible carrier device OSTEOGROW for bone healing. Int Orthop 38(3):635–647. doi:10.1007/s00264-013-2201-1
Lissenberg-Thunnissen SN, de Gorter DJ, Sier CF, Schipper IB (2011) Use and efficacy of bone morphogenetic proteins in fracture healing. Int Orthop 35(9):1271–1280. doi:10.1007/s00264-011-1301-z
Shahid M, Hussain A, Bridgeman P, Bose D (2013) Clinical outcomes of the Ilizarov method after an infected tibial non union. Arch Trauma Res 2(2):71–75. doi:10.5812/atr.11300
Brinker MR, Hanus BD, Sen M, O'Connor DP (2013) The devastating effects of tibial nonunion on health-related quality of life. J Bone Joint Surg Am 95(24):2170–2176. doi:10.2106/jbjs.l.00803
Zeckey C, Mommsen P, Andruszkow H, Macke C, Frink M, Stubig T, Hufner T, Krettek C, Hildebrand F (2011) The aseptic femoral and tibial shaft nonunion in healthy patients - an analysis of the health-related quality of life and the socioeconomic outcome. Open Orthop J 5:193–197. doi:10.2174/1874325001105010193
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36) I. Conceptual framework and item selection. Med Care 30(6):473–483
Kurth BM, Ellert U (2002) The SF-36 questionnaire and its usefulness in population studies: results of the German Health Interview and Examination Survey 1998. Soz Praventivmed 47(4):266–277
Zlowodzki M, Obremskey WT, Thomison JB, Kregor PJ (2005) Functional outcome after treatment of lower-extremity nonunions. J Trauma 58(2):312–317
Motsitsi NS (2008) Management of infected nonunion of long bones: the last decade (1996-2006). Injury 39(2):155–160. doi:10.1016/j.injury.2007.08.032
Bishop GB, Einhorn TA (2007) Current and future clinical applications of bone morphogenetic proteins in orthopaedic trauma surgery. Int Orthop 31(6):721–727. doi:10.1007/s00264-007-0424-8
Pecina M, Giltaij LR, Vukicevic S (2001) Orthopaedic applications of osteogenic protein-1 (BMP-7). Int Orthop 25(4):203–208
Antonova E, Le TK, Burge R, Mershon J (2013) Tibia shaft fractures: costly burden of nonunions. BMC Musculoskelet Disord 14:42. doi:10.1186/1471-2474-14-42
Brinker MR, O'Connor DP (2007) Outcomes of tibial nonunion in older adults following treatment using the Ilizarov method. J Orthop Trauma 21(9):634–642. doi:10.1097/BOT.0b013e318156c2a2
Bowen CV, Botsford DJ, Hudak PL, Evans PJ (1996) Microsurgical treatment of septic nonunion of the tibia. Quality of life results. Clin Orthop Relat Res 332:52–61
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wichlas, F., Tsitsilonis, S., Disch, A. et al. Long-term functional outcome and quality of life after successful surgical treatment of tibial nonunions. International Orthopaedics (SICOT) 39, 521–525 (2015). https://doi.org/10.1007/s00264-014-2629-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2629-y