Abstract
Purpose
Total knee arthroplasty (TKA) in limbs affected by poliomyelitis is a technically challenging procedure. These patients often demonstrate acquired articular and metaphyseal angular deformities, bone loss, narrowness of the intramedullary canals, impaired quadriceps strength, flexion contractures and ligamentous laxity producing painful hyperextension. Thus, using condylar knee designs in these patients will likely result in early failure because of instability and abnormal load distribution. The aim of this study was to assess the outcomes associated with use of the customised (SMILES) rotating-hinge knee system at our institution for TKA in poliomyelitis-affected limbs.
Methods
We retrospectively reviewed the outcome of 14 TKAs using the (SMILES) prosthesis in 13 patients with limbs affected by poliomyelitis. All patients had painful unstable knees with hyperextension. There were ten females and three males with a mean age of 66 years (range 51–84) at time of surgery. Patients were followed up clinically, radiologically and functionally with the Oxford knee score (OKS). Mean follow-up was 72 months (16–156).
Results
There were no immediate or early complications. One patient fell and sustained a peri-prosthetic fracture at seven months requiring revision to a longer stem. Radiological evaluation showed satisfactory alignment with no signs of loosening in all cases. Mean OKS improved from 11.6 (4–18) to 31.5 (18–40) postoperatively (p < 0.001).
Conclusion
The rotating hinge (SMILES) prosthesis is effective at relieving pain and improving function in patients with poliomyelitis. The device compensates well for ligamentous insufficiency as well as for any associated bony deformity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Poliomyelitis is a highly infectious viral disease, which predominantly affects young children but it can also affect adults. The virus is spread via the faeco-oral route and infects the central nervous system. It can cause paralysis within a week of infection. Initial symptoms are non-specific such as fever, headache, nausea and vomiting, pain in the limbs and neck stiffness. In less than 1 % of patients it causes paralysis, usually affecting the lower limbs. It can be fatal if the respiratory muscles are involved. Although there is no cure for polio, vaccination against it is highly effective. Introduction of the vaccine in the 1950s has almost eradicated polio in the developed world. In a few countries such as Nigeria, Pakistan and India, the disease is still endemic [1, 2].
Patients with limb paralysis develop abnormal alignment, generalized hypotonia and ligamentous laxity, which predispose to knee pathology at a young age. Early joint salvage options include soft tissue releases and corrective osteotomy to improve congruity, alignment and stability. However, when painful osteoarthritis (OA) develops, especially in the presence of ligamentous laxity producing painful hyperextension, total knee arthroplasty (TKA) is indicated. In these patients, TKA is often complicated by acquired articular and metaphyseal angular deformity, bone loss, narrowness of the femoral and tibial canals, impaired quadriceps strength, flexion contracture and ligamentous laxity. Furthermore, abnormal lower limb rotational profiles often predispose to a chronically subluxed or dislocated patella [3–6]. In the presence of these complicating factors, performing total knee arthroplasty using condylar designs will likely result in early failure as a result of instability and abnormal load distribution across the knee. Furthermore, addressing significant metaphyseal/diaphyseal angular deformities during TKA, when using off-the-shelf stemmed designs, may necessitate performing corrective osteotomies to accommodate the straight stems, which carries the inherent risk of non-union in addition to delaying weight bearing postoperatively. At our institution, we advocate use of the customised (SMILES) rotating hinge prosthesis for TKA in these challenging cases.
The aim of this study was to determine the functional and radiological outcomes in poliomyelitis patients following TKA using the (SMILES) system at our institution.
Materials and methods
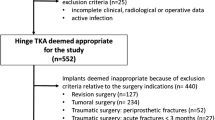
The study was registered with the Research & Development office at our institution (SE12.018). We identified the patients by searching through our Biomedical Engineering department (BME) database. A retrospective review was carried out on all consecutive poliomyelitis patients who had a custom hinged total knee replacement (SMILES) between 1996 and 2013. There were 13 patients in total. We obtained all relevant data through reviewing the patients’ case notes, outpatient assessments, telephone interviews/questionnaires and imaging studies. Functional analysis was performed using the Oxford knee scoring system (OKS) [7].
There were ten women and three men, with a mean age at surgery of 66.0 years (range 51–84). Mean follow-up was 72 months (16–156). Three patients died due to unrelated reasons during follow-up. For these patients we used the most recent OKS and last clinical follow up prior to their death.
The prosthesis
The Stanmore Modular Individualised Lower Extremity System (SMILES) prosthesis (Stanmore Implants Worldwide Ltd. Stanmore, United Kingdom) is a second-generation hinged design manufactured using CAD-CAM technology (Fig. 1). The femoral component is made of cobalt-chromium-molybdenum alloy with a titanium stem. It has an axle made of cobalt-chromium-molybdenum, a pair of ultra-high-molecular-weight polyethylene (UHMWPE) bushes and a titanium circlip. The tibial component is also made of cobalt-chromium-molybdenum alloy and a UHMWPE bearing surface and a titanium stem and casing. The prosthesis also has five degrees of hyperextension built into it. The length, diameter, curvature and angulation of the femoral and tibial stems are customised based on pre-operative biplanar radiographs to optimise fixation and to compensate for skeletal deformities and bone loss. The bearing surfaces are bevelled to constrain rotational movement and there is a hyperextension bumper pad. These design features compensate for ligamentous instability, which are a common feature of patients with polio. Customised plateau plates and wedges are also available if required. The SMILES prosthesis incorporates many of the design features of second-generation rotating-hinge devices to improve the biomechanics of the joint and provide better clinical outcomes.
Surgical technique
Senior surgeons in the joint reconstruction unit at our institution performed all operations. These were carried out with the patient in the supine position with a tourniquet, side support for the operated knee and a foot bolster. One dose of prophylactic intravenous antibiotic was given at induction of anaesthesia. After routine preparation and draping, a midline incision with a standard medial parapatellar approach was used to access the joint. The anterior cruciate ligament was either rudimentary or absent in all knees. Soft tissue balancing was achieved by medial, lateral and posterior releases as appropriate to address coronal and/or sagittal plane deformities. The tibial plateaus were resected with a saw using extra-medullary referencing (2 mm off the lower side). The tibial canal was then reamed to a depth of 140 mm for short stems and 180 mm for long stems using flexible reamers. The distal femoral cut was performed with aid of the customised intramedullary rod provided. This was inserted into the femoral canal with great care to avoid fracturing the cortex. A distal femoral cut (9–11 mm) was then made (5–7° valgus). After sizing, a femoral cutting block was used for the anterior, posterior and chamfer cuts. Rotation of the femoral component was set based on the anatomical landmarks and also looking at the flexion gap balance/orientation of the tibial cut with the knee in 90° flexion. Sequential flexible reamers were used to ream the femoral canal to a depth of 140 mm or 180 mm, and a diameter approximately 1 mm larger than the femoral stem. Supracondylar osteotomy was not required in any of our patients. The indication for patellar resurfacing was substantial patellofemoral arthritis in the presence of a sufficiently thick patella (>12 mm). A trial reduction was then carried out to ensure adequate balance, stability, range of motion and patellar tracking. We used cement to fill any bone defect <5 mm and metal augments for defects ≥5 mm. Once satisfied, all trial components were removed and the corresponding definitive components were selected. The femoral and tibial components were then cemented into the corresponding canals, ensuring the correct orientation. The tibial bearing components were then applied. Finally, assembly was completed by aligning the femoral and tibial components and inserting the axle, before securing it by inserting the circlip. Finally, a thorough washout with normal saline pulse lavage was performed prior to closure.
Patients were mobilised fully weight-bearing on the first postoperative day. Thromboprophylaxis consisted of thromboembolic deterrent stockings for four weeks and low molecular-weight heparin for two weeks. Patients were reviewed clinically and radiologically at six weeks, 12 weeks, six months, and annually thereafter. Function was evaluated using the Knee Society score pre-operatively and at final follow-up.
Serial anteroposterior and lateral radiographs were reviewed post-operatively, at six months, and on an annual basis thereafter using the Knee Society radiological score [8] for each component on the most recent radiograph. If radiolucent lines (RLLs) were present, all previous radiographs were compared to identify whether the RLL was progressing.
Results
Clinical outcomes and complications
There were no immediate postoperative complications in any of our patients. One patient had a fall at home sustaining a peri-prosthetic fracture of the tibia seven months after the index operation. This required revision of the prosthesis to a longer stem bypassing the fracture site. This fracture had fully healed up radiologically and clinically at last follow-up and the patient now has a well functioning knee at 45 months. One patient required a manipulation under anaesthesia four months after the original operation due to poor knee flexion. This improved from a pre manipulation flexion of 70 degrees to 100 degrees after the manipulation. To date, no revision surgery has been performed in our cohort at a mean of 72 months (range 16–156 months) following index surgery.
Functional outcome
The OKS improved from a pre-operative mean of 10.6 (range 4–18) to a postoperative mean of 30.7 (range 18–39) at 72 months follow-up. The OKS improved significantly in all patients following surgery (p < 0.001 using the two-tailed T-test). Mean hyperextension pre-operatively was 16.7° (10–30°) and decreased postoperatively to 1.4° (−5° to 0°). Only one of the patients had an extension lag of 5°.
Patient satisfaction
All patients in the cohort were asked about how satisfied they were with the results of their operation (Table 1). Out of the ten surviving patients, six patients indicated that they were very satisfied with the procedure, three patients were just satisfied and one patient was neither satisfied nor unsatisfied with the outcome. The mean quadriceps strength in our cohort of patients was 2.8 (range 1–4) with five patients with less than antigravity strength (1 or 2). Out of the 13 patients in our cohort, six patients used a wheelchair due to generalised immobility. Two patients used wheelchairs outdoors but were able to walk either unaided or with the use of a walking stick or crutches at home. Four patients used walking aids only. One patient in the cohort walked unaided. None of the patients wore callipers following surgery.
Radiological analysis
All radiographs were independently assessed by two authors (first and second authors) for component alignment, migration and the presence of loosening using the Knee Society radiological score. Two radiographic views (anteroposterior and lateral) were studied for each prosthesis. All the prostheses reviewed had satisfactory positioning on plain radiographs with no features of loosening or migration. The pre and postoperative radiographs of an example case in this study are shown in Fig. 2a–b.
Discussion
Our study reports encouraging results following TKA in a difficult and unique group of patients. We advocate the use of the custom (SMILES) rotating hinge system in poliomyelitis patients because the versatility of the device allows addressing the numerous structural and anatomical abnormalities frequently encountered in these patients. Furthermore, it is well recognised that patients with poor quadriceps function often rely on locking the knee in hyperextension or ‘back-kneeing’ for stability and walking, and this is why conventional condylar or semi constrained total knee replacements may actually cause deterioration in walking by eliminating the hyperextension. Patients may be prone to their knees buckling under their weight as the hyperextension is eliminated. With the (SMILES) custom-made device, this can be built into the prosthesis so that walking is not compromised.
We recognise that our study has limitations. First, this is a small study with somewhat limited follow-up. However, to our knowledge, this is the largest cohort of poliomyelitis patients with hinged knee prostheses reported in the literature so far, and the first using a custom device. Second, we did not have a control group or any previously published randomised control data to compare our results with. Finally, poliomyelitis patients have multiple joint and limb pathology that may restrict mobility and impair lifestyle. Interpreting functional outcomes in these patients is difficult. In the 13 patients that we studied, six patients used a wheelchair at some point during follow-up. This may have confounded our results.
The first generation of rotating hinge knee replacements were unsuccessful due to poor functional results and a high failure rate [9]. All these prostheses had early loosening due to the high force transmission across the bone–cement interface in both the tibial and femoral components. The second generation added design modifications to overcome these deficiencies. A mobile bearing was added to reduce forces across the bone cement interface; the hinge was made more congruent and the patello-femoral articulation has been improved which has reduced tracking problems. In addition, modular segments were added to fill in bony defects, making this prosthesis particularly attractive in the revision setting. It has been shown that the current generation of rotating hinged total knee systems have overcome many of the initial design faults, thereby offering better outcomes with lower revision rates [9]. The (SMILES) system used in this study is a second generation rotating hinge device incorporating all the above design modifications.
There is sparse literature on the outcome of TKA in polio-affected patients and most show poor results [3, 5, 10]. Giori et al. [3] demonstrated a high incidence of recurrence of instability and functional deterioration. They commented on the relationship between functional outcome and preoperative quadriceps strength, where patients with at least antigravity strength demonstrated a better outcome. The authors recommended the use of hinged devices in these patients due to poor pain relief, recurrence of hyperextension and poor long-term functional outcome when conventional devices were used. Jordan et al. [5] also reported progressive functional deterioration in all knees that had undergone TKA using semi-constrained devices after demonstrating good pain relief and stability initially. In a further study by Patterson and Insall [10], two out of nine patients developed a recurrent recurvatum deformity, both requiring revision surgery for their symptoms. They also found favourable results using more constrained devices. The mean follow-up in our study was 72 months with no patients developing recurrence of symptoms or deformity since surgery. The findings of all these studies are summarised in Table 2.
In summary, TKA is a technically challenging procedure in patients with poliomyelitis-affected limbs due to bony and soft tissue abnormalities. These patients frequently have weakness in their quadriceps muscles and rely on hyperextension of the knee for stability. Our data suggest that using a custom hinged knee device with built-in hyperextension potentially addresses the stability issue in the presence of poor quadriceps function. The mid-term clinical and functional outcomes, as shown in this report, are encouraging. In conclusion, we recommend use of the custom (SMILES) system for TKA in selected patients with limbs affected by poliomyelitis. The device appears to compensate well for instability and hyperextension seen in these patients, and is also able to address any associated bony deformities.
References
Nathanson N, Kew OM (2010) From emergence to eradication: the epidemiology of poliomyelitis deconstructed. Am J Epidemiol 172(11):1213–1229
WHO (2012) Poliomyelitis fact sheet N°114, October 2012, WHO. http://www.who.int/mediacentre/factsheets/fs114/en. Accessed 16 October 2014
Giori NJ, Lewallen DG (2002) Total knee arthroplasty in limbs affected by poliomyelitis. J Bone Joint Surg (Am) 84-A(7):1157–1161
Tigani D, Fosco M, Amendola L, Boriani L (2009) Total knee arthroplasty in patients with poliomyelitis. Knee 16(6):501–506
Jordan L, Klingman M, Sculco TP (2007) Total knee arthroplasty in patients with poliomyelitis. J Arthroplasty 22(4):543–548
Sewell MD, Hanna SA, Al-Khateeb H, Miles J, Pollock RC, Carrington RWJ, Skinner JA, Cannon SR, Briggs TWR (2012) Custom rotating-hinge primary total knee arthroplasty in patients with skeletal dysplasia. J Bone Joint Surg (Br) 94(3):339–343
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg (Br) 80(1):63–69
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res (248):9–12
Barrack RL (2001) Evolution of the rotating hinge for complex total knee arthroplasty. Clin Orthop Relat Res (392):292–299
Patterson BM, Insall JN (1992) Surgical management of gonarthrosis in patients with poliomyelitis. J Arthroplasty 7(Suppl):419–426
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rahman, J., Hanna, S.A., Kayani, B. et al. Custom rotating hinge total knee arthroplasty in patients with poliomyelitis affected limbs. International Orthopaedics (SICOT) 39, 833–838 (2015). https://doi.org/10.1007/s00264-014-2572-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2572-y