Abstract
Purpose
Active shoulder function after segmental tumour resection of the proximal humerus and endoprosthetic reconstruction is regularly compromised, while the overall arm function allows a satisfying use in daily activities. The main functional problem remains the loss of huge parts of the shoulder girdle musculature and its bony attachment. In revision arthroplasty inverse shoulder implants can improve the active range of motion significantly in comparison to anatomical shaped prostheses. The aim of this study was to investigate if these promising experiences are transferable to reconstructions after tumour resection of the proximal humerus by using a modular inverse tumour prosthesis.
Methods
In this study we observed the functional and oncological results of 18 inverse proximal humerus endoprosthetic replacements (IPHP) with the MUTARS system (Implantcast®) after resection of benign (1x giant cell) and malignant (11x primary bone sarcoma, 5x bone metastasis of carcinoma) bone tumours. Mean age at operation was 42 years. The mean postoperative follow-up was 33 months (range ten to 120).
Results
Resection margins were wide in 13 and marginal in five patients. Mean reconstruction length was 15.1 cm (range 6–25 cm). Mean operation time was 191 minutes. The axillary nerve was mostly preserved in 78 % (n = 14). At latest follow-up the patients presented a medium MSTS-score of 24.6/30. The mean active arm abduction in the shoulder joint was 78° and 88° active arm elevation for patients with intact axillary nerve function, but significantly reduced for the four patients with compromised deltoid function. One patient needed a surgical revision due to a deep implant infection.
Conclusions
The IPHP offers a significant improvement of active shoulder function in patients in whom the axillary nerve can be preserved in comparison to anatomically-shaped implants. However, for patients without any deltoid function there is no benefit regarding an improved active range of motion using an IPHP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The proximal humerus is the third most common site for primary bone tumours and secondary malignancies like bone metastasis of carcinoma [1]. Segmental resection of the tumour bearing bone and the enclosed soft tissues is imperative in primary bone sarcoma and is performed increasingly in patients with solitary bone metastasis of carcinoma to reduce tumour burden and improve the oncological outcome [2]. Nowadays limb reconstruction with modular tumor megaendoprostheses is a standard procedure [3–5]. In recent decades major complications like periprosthetic infections, aseptic loosening and luxations could be significantly reduced and good functional results in the lower limb are achieved [3, 6–8]. In the upper limb the implant-associated complications are low [9–12]. However, the functional results are poor because the axillary nerve has to be sacrificed in the majority of cases in high grade sarcoma in order to achieve a wide resection according to Enneking et al. [13]. Even if the nerve can be preserved, relevant parts of the rotator cuff have to be sacrificed resulting in a decentration of the humeral head and loss of function of the deltoid muscle. In our clinic the anatomically designed prosthesis was embedded in an attachment tube and the remaining muscles were fixed on it [14]. Thus, a stable positioning of the joint is possible, but the patient is not able to perform an active abduction and elevation of the arm [3]. Even techniques like the Bateman procedure in the case of axillary nerve resection were not successful with a conventional prosthesis because of the remaining decentration of the humeral head [15]. As the use of anatomical shaped implants is still the standard procedure for the majority of patients, there is an increasing number of studies presenting satisfying results using different types of reverse proximal humerus reconstructions [16].
Reversed shoulder arthroplasty is an established procedure in patients with loss of the function of the rotator cuff, which achieves good functional results. The medialised and semi-constrained artificial joint restores stability and motility [17]. In the past they were only used in older patients because of high complication rates, fear of early loosening of the glenoid component [18] and declining function after eight to ten years [19]. Reversed shoulder arthroplasty by using tumour prostheses often concerns younger patients with a major loss of muscles. The aim of this study was to transfer the improvements of function in primary and secondary shoulder arthroplasty towards younger tumour patients. We determined whether the implantation of an inverse tumour prosthesis after segmental resection of the proximal humerus can improve the active range of motion in the restored shoulder joint and if there are any contradictions or procedure-related complications in a short- to mid-term follow-up.
Patients and methods
We retrospectively reviewed 18 patients with aggressive or malignant bone tumours of the proximal humerus who underwent a segmental bone and soft tissue resection and who received an inverse proximal humerus tumor endoprosthesis (IPHP) (MUTARS Inverse, Implantcast). All patients had surgery at a single institution and were treated between 2003 and 2012. As a strong mechanical link between the musculature and the prosthesis is required to regain active function, a reattachment tube was used in all patients either for the reconstruction of the capsule to stabilize the joint and to avoid luxation, as well as for the reattachment of the soft tissues to the implant. The remaining muscular tendons of the mm. latissimus dorsi, subscapularis and the pectoralis were refixed in anatomical positioning at the tube to regain active rotation, and most importantly, the m. deltoideus attachment was reconstructed to the implant to assess active abduction and elevation.
After implantation of the inverse prosthesis the shoulder range of motion was restricted in a shoulder immobilizer for four to six weeks (depending on the extend of soft tissue reconstruction) and afterwards mobilization started. All patients were followed up clinically and by plain X-ray on a regular basis in three- to four-month intervals.
The medium follow up was 33.6 months (range four to 108) after implantation of the inverse prosthesis. The presented MSTS (Musculuskeletal Tumour Society) score as well as the functional assessment was collected at the latest follow-up examination of the patient. The MSTS score assigns numerical values (0–5) for each of six categories (pain, function, emotional acceptance, hand positioning, manual dexterity, lifting ability). It is a valid score to compare patients functional and emotional end-results after musculoskeletal reconstructions after tumour resection [20]. Thirty points is the highest reachable score, representing a functional outcome comparable to healthy people.
Results
Medium age of the patients was 42 years (11 male, seven female). Detailed information about the primary diagnosis and the tumour staging is presented in Table 1. In 16 of these patients the IPHP was implanted after tumour resection as a single step procedure. In two patients a cement spacer was implanted after tumour resection because of an assumed infection of the biopsy tract to prevent a deep implant infection. Six weeks after implantation of the cement spacer the patients underwent an exchange of the spacer towards an IPHP.
The main branches of the axillary nerve were preserved in 14 patients. Two patients had a partial transection of nerve branches, and a complete transection of the main nerve was present in two patients.
Intraarticular resection was carried out in 17/18 patients and extraarticular resection in one patient.
The mean time of operation was 191 minutes (range 116–305 minutes) for the primary tumour resection and reconstruction. For the two cases in which a conversion (spacer towards IHPH) was performed the time of the revision operation was 178 minutes on average. Only two patients required an infusion of pRBC (packed red blood cells) during the operation. No intra-operative complications were observed.
The mean length of resection and reconstruction of the proximal humerus was 15.1 cm (range 6–25 cm). In all but one patient the bony insertion of the deltoid muscle was detached completely in consequence of the tumour resection.
The achieved resection margins according to the Enneking classification [13] were wide in 13 and marginal in five. No local recurrence was observed. Two patients died of disease ten and 13 months after implantation of the inverse prostheses because of progressive systemic disease. One patient died in a car accident 37 months after surgery. Seven patients were alive with disease at latest follow up (medium of 20 months after IPHP). The remaining patients were free of disease an average of 50 months after IPHP.
Five (29 %) postoperative complications were observed. One patient developed a deep implant infection with an MRSA (methicillin resistant staphylococcus aureus) which led to the explantation of the implant and implantation of a cement spacer four weeks after the primary operation. Notably, before the tumour resection and endoprosthetic reconstruction this patient underwent local irradiation and three prior ostesynthesis due to pathological fracture of the humerus (in the case of renal cell carcinoma metastasis) and was operated on because of tumour recurrence and implant failure. In four patients a joint instability with luxation of the implant was observed. One patient presented with repetitive luxation and a significant instability of the shoulder joint seven months after implantation of the IPHP. She was then treated conservatively with a restriction of the shoulder joint mobility with an abduction pillow for six weeks and afterwards intensive physiotherapy to strengthen the shoulder musculature and re-stabilize the joint. In this patient the joint stability was regained and she presented with the best functional outcome of the series. A second patient presented a chronic cranial subluxation. Although shoulder joint function was strictly limited, he refused surgical intervention because of progressive systemic disease of prostate cancer. In the third patient, a chronic asymptomatic cranial dislocation was accepted without further treatment because of initial damage of the axillary nerve and non function of the deltoid muscle. The chance to regain joint stability or a functional improvement with a revision operation was expected to be low and therefore a second operation was rejected. The forth patient had one cranial luxation five months after the operation. Closed reposition was performed and intensive physiotherapy was recommended to strengthen the joint stability. No further dislocations were noticed. Also, this patient had a partial axillary nerve damage due to a prior operation. All other patients were without implant or procedure-related complications. Particularly, no loosening of the glenoid component was observed.
The functional outcome was significantly linked to whether the axillary nerve and therefore the deltoid function were intact or if it was compromised. Patients with intact deltoid function were superior to the others. Excluding patient 6 (refer to Table 2) because of the chronic dislocation, the mean active abduction for these patients was 80° (range, 40–180), elevation 84° (range, 30–160), and active internal and external rotation of 47° (range, 25–80) and 35° (range, 15–50), respectively. Due to the chronic joint dislocation patient 6 presented a limited active range of motion which was comparable to patients without deltoid function despite a preserved axillary nerve (refer to Table 2). The four patients with axillary nerve damage presented a reduced active range of motion, an average abduction of 37°, 25° retroversion, 35° elevation and 16° active external rotation. Although, the data analysis did not reach statistical significance (p = 0.21 anteversion, p = 0.26 abduction). Further, interestingly even in this subgroup there was a difference observed between patients with a complete loss of the axillary nerve compared to the two patients with a partial lesion (patients 10 and 16 compared to 13 and 15; Table 2).
To our amazement in the two patients treated with a cement spacer initially, the functional outcome was comparable in one (patient 13) and superior than average in the other one (patient 2) compared to patients with intact deltoid function.
The functional evaluation using the MSTS score did not reflect these differences regarding the active shoulder function. Medium MSTS score was 25.1/30 for patients with intact deltoid function and with a mean score of 24.5/30, just slightly inferior after complete or partial loss of the axillary nerve (p = 0.432).
Although the resection length varied from 6.5 cm to 25 cm there was no influence observed on the functional outcome, neither on the MSTS score nor on the active range of motion of the shoulder joint. The same result applies to the tumour size.
Seven patients received additional local irradiation treatment before (n = 3) and after (n = 4) IPHP implantation. Although there was a trend towards a reduced functional outcome in these patients in terms of active shoulder movement (refere to Table 2) the difference compared to patients without local radiation was not statistically significant (abduction p = 0.12; anteversion p = 0.109).
The only statistically significant parameter negatively influencing the functional outcome was the local tumour expansion. Tumours without soft tissue expansion did better than tumours with extraskeletal tumour involvement. Significant levels were reached for abduction (p = 0.021) and anteversion (p = 0.016) but were not significant for IRO (p = 0.23) and ERO (p = 0.76).
Discussion
After segmental resection of the proximal humerus because of malignoma, multiple forms of reconstruction have been reported with comparable oncological results in terms of survival and local recurrence rates [21]. Endoprosthetic reconstruction is described to have less procedure-related complications like implant failure, septic or aseptic loosening than other types of reconstruction. Although we are aware of the limitations of our study in terms of the short to medium follow-up of just 34 months and the limited number of 18 patients, our results are in concordance with data presented in the literature [12, 22, 23]. To mention, we did not see any loosening of the glenoid component, even in the patients with a longer follow-up and a good overall function, although this is a major concern in using inverse implants especially in young patients [18]. One concern of implant-related complications is the PE wear which can possibly cause aseptic loosening of the implant due to a wear-induced inflammatory reaction. Large articulating surfaces and a long leverage of the proximal humerus prostheses may cause a higher amount of PE wear in comparison to anatomical shaped implants as well as other reverse implant designs. Although an in-vitro study of our research group detected more PE particles in the inverse proximal humerus implant compared to anatomical-shaped shoulder prostheses, the amount of debris was within acceptable values and comparable to other inverse implants [24]. Other regularly seen complications, like acromial insufficiency, glenosphere disengagement or scapula fractures, which are described by Scarlat in his review investigating the complications with reverse shoulder arthroplasty [25], did not appear in our series. Key factors negatively influencing the rate of complications like revision arthroplasty, glenoid deformities or osteoporosis are more frequent in older patients with glenohumeral arthrosis compared to a younger tumour patient population. Therefore, it is difficult to match these different patient groups in terms of influencing factors on complications as the preconditions and indications for the implantation of the IPHP are diverse.
In surgical oncology large bone defects (average of 15.1 cm in this series), the loss of huge parts of the functional shoulder girdle musculature, the loss of the tendons attachment to the bone and the difficulty in the soft tissue reattachment are key factors causing joint instability and a strictly limited active range of motion of the shoulder joint. Hence, dislocation or subluxation of the PHP in up to 20 % due to insufficient soft tissue guidance is described as the main complication using anatomical shaped implants as well as using IPHP [11, 12, 16, 21, 23]. With two repetitive and two chronic dislocations we faced the same problem in our series. Two of them were treated successfully with conservative treatment only. The other two refused surgical intervention after failed conservative treatment. We assume that these complications were probably related to the weak muscular guidance after tumour resection but also caused by the intraoperative difficulty to achieve the correct adjustment of the soft tissue tension with the modular implant. As presented by several authors the correct adjustment of the soft tissue pretension is a decisive step in using inverse implants to gain joint stability but also to achieve a good functional outcome [26, 27]. A short arm lengthening from 0 to 2 cm seems to be favourable to gain a sufficient pretension of the deltoid muscle to achieve a better functional outcome and to avoid dislocation as Lädermann et al. presented. However, a misjudgment of the correct reconstruction length, particularly an arm overlength, may cause neurological lesions [28, 29] with a negative influence on the shoulder function. The IPHP used in our series allowed the adaption of the implant length in 2-cm steps only, which may lead to an insufficient pretension of the musculature with a consecutive joint instability and implant dislocation as seen in 4/17 patients. Modifications of the humerus cap component, by means of three different sizes, have been implemented recently to exclude this difficulty, allowing a more accurate adjustment of the reconstruction length and pretension.
Besides, the most serious problem using an anatomical EPHP remains the functional outcome of the restored shoulder joint [30]. The active range of motion is strictly limited and above shoulder activities are almost always precluded. Although numerous articles deal with this topic, few of them provide data of active range of motion or influencing parameters like resection length or the status of the axillary nerve [21]. Further, if presented, the influence of the axillary nerve status on the functional outcome seems to be non-significant using conventional PHP as, for example, Kumar et al. [11] present in their series. They report of a mean abduction of 44° and 55° flexion for all patients after implantation of a conventional PHP. However, they did not find a functional benefit in patients with preservation of the axillary nerve compared to patients without deltoid function. Besides, even in 83 patients with axillary nerve preservation, Cannon et al. [30] presented a mean active abduction of 41° and a mean active forward flexion of 42° using a conventional PHP. In contrast, with regard to our results, using the IPHP, the integrity of the axillary nerve is the key factor for the functional outcome. With a medium active abduction of 80° and 84° elevation for patients with axillary nerve preservation, the presented functional results are superior compared to conventional PHPs. To mention the patients with complete axillary nerve damage did not show any benefit of the IPHP. Besides, even the two patients with partial deltoid function presented a more superior function than Cannon et al. presented for patients using a conventional PHP and intact deltoid function. In our opinion, these data indicate that the use of an inverse implant is recommended for all patients in whom the axillary nerve can be preserved. The use of anatomically-designed implants in these patients should be avoided because one abandons the potential of the deltoid muscle function and the accessible larger active range of motion in the shoulder joint. Contrarily, in patients with loss of the deltoid innervation the use of an IPHP is not profitable in terms of a functional improvement.
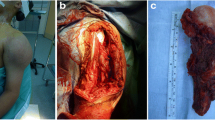
The resection length was a non-significant parameter on the functional outcome in our series. However, the larger the resection length, the more functional musculature is detached, leading to a more complex soft tissue reconstruction with a decreased functional outcome. De Wilde et al. [16] present in their series of 14 proximal humerus reconstructions using an composite autograft with a reverse shoulder prostheses an average active abduction of 157°, which is superior to our results, but a detachment of the deltoid muscle was performed in two cases only. Unfortunately they did not present the medium resection length. In our series we were able to preserve the deltoid muscle insertion at the proximal humerus in the one patient with a giant cell tumour (patient 1; Table 1; Fig. 1) only. She achieved a comparable functional outcome in terms of active range of motion (Fig. 2a and b).
Interestingly, as the increased active abduction, elevation and rotation ability in our series using the IPHP is, to our experience, a significant improvement of the functional use of the arm for the patients in daily use, the results of the MSTS-score evaluation do not reflect this improved function properly. Even in patients with conventional PHP or biological reconstructions, the elbow and hand function is regularly intact, providing an adequate use of the arm in daily activities represented by satisfying MSTS scores between 69 and 79 % [10, 11, 21, 22]. These values are comparable to our series. The medium MSTS score of all patients was 80 % (24/30). Interestingly, we observed no difference between patients with intact vs. compromised deltoid function. Therefore, one has to consider that the comparability between conventional PHP and the IPHP using this scoring system is not feasible as the severe restrictions of the shoulder function are not reflected by this score.
Conclusion
Our data emphasize that the use of the IPHP for the reconstruction of the proximal humerus after tumour resection and the restoration of the shoulder joint is favourable compared to anatomically-shaped implants even in young patients. Operational effort (operation length, blood loss), perioperative complications and oncological outcome are comparable to conventional PHP, at least after a short to midterm follow up. Even after implant failure the functional restriction is not inferior to a conventional PHP. We therefore recommend the use of an IPHP in all patients in whom the axillary nerve can be preserved completely and even partially, in consideration of the necessary oncological margins. For patients with deltoid impairment a functional benefit is not obvious and the use of an IPHP can therefore not be recommended.
References
Campanacci M (1999) Bone and soft tissue tumors, 2nd edn. Springer-Verlag, Wien
Fottner A, Szalantzy M, Wirthmann L et al (2010) Bone metastases from renal cell carcinoma: patient survival after surgical treatment. BMC Musculoskelet Disord 11:145
Gosheger G, Gebert C, Ahrens H et al (2006) Endoprosthetic reconstruction in 250 patients with sarcoma. Clin Orthop Relat Res 450:164–171
Mittermayer F, Krepler P, Dominkus M et al (2001) Long-term followup of uncemented tumor endoprostheses for the lower extremity. Clin Orthop Relat Res 388:167–177
Sluga M, Windhager R, Lang S et al (1999) Local and systemic control after ablative and limb sparing surgery in patients with osteosarcoma. Clin Orthop Relat Res 358:120–127
Gosheger G, Goetze C, Hardes J et al (2008) The influence of the alloy of megaprostheses on infection rate. J Arthroplasty 23:916–920
Hardes J, Ahrens H, Gebert C et al (2007) Lack of toxicological side-effects in silver-coated megaprostheses in humans. Biomaterials 28:2869–2875
Hardes J, von Eiff C, Streitbuerger A et al (2010) Reduction of periprosthetic infection with silver-coated megaprostheses in patients with bone sarcoma. J Surg Oncol 101:389–395
Streitburger A, Henrichs M, Hardes J et al (2012) Endoprosthetic reconstruction of the proximal humerus in malignoma. Oper Orthop Traumatol 24:174–185
Rodl RW, Gosheger G, Gebert C et al (2002) Reconstruction of the proximal humerus after wide resection of tumours. J Bone Joint Surg Br 84:1004–1008
Kumar D, Grimer RJ, Abudu A et al (2003) Endoprosthetic replacement of the proximal humerus. Long-term results. J Bone Joint Surg Br 85:717–722
Funovics PT, Dominkus M (2010) Modular tumor prostheses of the humerus. Orthopade 39:968–979
Enneking W, Dunham W, Gebhardt M et al (1990) A system for the classification of skeletal resections. Chir Organi Mov 75:217–240
Hardes J, Ahrens H, Nottrott M et al (2012) Attachment tube for soft tissue reconstruction after implantation of a mega-endoprosthesis. Oper Orthop Traumatol 24:227–234
Gosheger G, Hardes J, Ahrens H et al (2005) Endoprosthetic replacement of the humerus combined with trapezius and latissimus dorsi transfer: a report of three patients. Arch Orthop Trauma Surg 125:62–65
De Wilde L, Boileau P, Van der Bracht H (2011) Does reverse shoulder arthroplasty for tumors of the proximal humerus reduce impairment? Clin Orthop Relat Res 469:2489–2495
Boileau P, Watkinson D, Hatzidakis AM, Hovorka I (2006) Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 15:527–540
Zumstein MA, Pinedo M, Old J, Boileau P (2011) Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg Am Shoulder Elbow Surg 20:146–157
Favard L, Levigne C, Nerot C et al (2011) Reverse prostheses in arthropathies with cuff tear: are survivorship and function maintained over time? Clin Orthop Relat Res 469:2469–2475
Enneking WF, Dunham W, Gebhardt MC et al (1993) A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 286:241–246
van de Sande MA, Dijkstra PD, Taminiau AH (2011) Proximal humerus reconstruction after tumour resection: biological versus endoprosthetic reconstruction. Int Orthop 35:1375–1380
Potter BK, Adams SC, Pitcher JD Jr et al (2009) Proximal humerus reconstructions for tumors. Clin Orthop Relat Res 467:1035–1041
Raiss P, Kinkel S, Sauter U et al (2010) Replacement of the proximal humerus with MUTARS tumor endoprostheses. Eur J Surg Oncol 36:371–377
Dieckmann R, Liem D, Gosheger G et al (2013) Evaluation of a reconstruction reverse shoulder for tumour surgery and tribological comparision with an anatomical shoulder arthroplasty. Int Orthop 37:451–456
Scarlat MM (2013) Complications with reverse total shoulder arthroplasty and recent evolutions. Int Orthop 37:843–851
Boileau P, Gonzalez JF, Chuinard C et al (2009) Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg Am 18:600–606
Hsu SHG, Saifi M, Ahmad CS (2011) Reverse total shoulder arthroplasty—biomechanics and rationale. Oper Tech Orthop 21:52–59
Ladermann A, Walch G, Lubbeke A et al (2012) Influence of arm lengthening in reverse shoulder arthroplasty. J Shoulder Elbow Surg Am 21:336–341
Ladermann A, Williams MD, Melis B et al (2009) Objective evaluation of lengthening in reverse shoulder arthroplasty. J Shoulder Elbow Surg Am 18:588–595
Cannon CP, Paraliticci GU, Lin PP (2009) Functional outcome following endoprosthetic reconstruction of the proximal humerus. J Shoulder Elbow Surg Am Shoulder Elbow Surg 18:705–710
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Streitbuerger, A., Henrichs, M., Gosheger, G. et al. Improvement of the shoulder function after large segment resection of the proximal humerus with the use of an inverse tumour prosthesis. International Orthopaedics (SICOT) 39, 355–361 (2015). https://doi.org/10.1007/s00264-014-2560-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2560-2