Abstract
Purpose
The aim of this study was to compare the functional outcome of patients following unicompartmental knee replacement (UKR) using the Oxford domed lateral UKR to patients who underwent cruciate-retaining total knee replacement (TKR) for isolated osteoarthritis in the lateral compartment.
Methods
With the help of our institutional database, we retrospectively identified 22 matched pairs with regards to age, gender and body mass index (BMI). Functional outcome was measured using the Oxford Knee Score (OKS) and range of motion (ROM). Complications and revisions were recorded.
Results
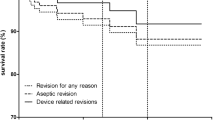
The mean follow-up was 22 (UKR) and 19 (TKR) months, respectively. Patients following UKR had a statistically significant higher mean postoperative OKS and ROM: mean OKS was 43 [standard deviation (SD) 4] for UKR and 37 (SD 9) for TKR, respectively (p = 0.023); ROM was 127° (SD 13) for UKR and 107° (SD 17) for TKR (p < 0.001). Additionally the change in score was statistically significant higher in patients following UKR in the OKS (14.3 (SD 6) vs. 9.6 (SD 8)) and in the range of motion (+12° (SD 19) vs. −3° (SD 20)), (p = 0.041 and p = 0.01 respectively). Survival at two years using revision for any reason as the endpoint was 96 % [95 % confidence interval (CI) 72–99] for UKR and 100 % for TKR (Log-rank test, p = 0.317).
Conclusion
The functional results of mobile-bearing UKR for isolated osteoarthritis in the lateral compartment compare favourably to those after cruciate-retaining TKR in the short term. To compare survival and complications after both procedures, longer-term follow-up is necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the clinical success of knee arthroplasty with significant improvement in function and reduction of pain level in patients with severe osteoarthritis [1], there is still a debate about the optimal surgical treatment of lateral unicompartmental osteoarthritis of the knee joint [2]. Unicompartmental knee replacement (UKR) is considered to have some valuable advantages in contrast to total knee replacement (TKR), such as the possibility of a minimal invasive surgical procedure with a small incision and limited exposure without dislocation of the patella, leading to less blood loss, a faster recovery and a decreased hospital admission as well as preservation of bone stock, ease of revision surgery and superior range of motion (ROM) with a more physiological knee kinematics due to preservation of the cruciate ligaments [2–12]. On the contrary, advocates of TKR refer to the lower cumulative survival rate for UKR in comparison with TKR, ranging from 82 % to 98 % at five to 22 years for UKR compared with 91 % to 98.9 % at five to 19 years for TKR [8, 13].
In the medial compartment, the Oxford UKR with mobile bearing is a widely acknowledged procedure for treating isolated osteoarthritis, with an excellent clinical outcome and high survival rates in the long term [14–16]. In contrast, early results of the Oxford UKR in the lateral compartment were disappointing, with high failure rates caused by dislocation of the bearing in up to 10 % of cases [17, 18]. Therefore, TKR was preferred for treating isolated osteoarthritis in the lateral compartment [17, 18].
To address the anatomical and biomechanical specifics of the lateral compartment, a modified lateral UKR was developed with a spherically convex, domed tibial plateau and a biconcave bearing, which should help to decrease the risk of dislocation [18, 19] (Fig. 1). Few clinical studies postulate a reduced dislocation rate of 0–6.2 % and excellent clinical outcome in the short term after implantation of the Oxford domed lateral tibial component for isolated osteoarthritis in the lateral compartment [18–22].
To date, there is no data published on the clinical outcome of patients after mobile-bearing UKR in comparison with patients with TKR for isolated osteoarthritis in the lateral compartment. Therefore, we performed a retrospective matched-pairs study to compare clinical results in patients after mobile-bearing UKR and cruciate-retaining TKR for isolated osteoarthritis in the lateral compartment.
Patients and methods
Between December 2006 and March 2009, 50 consecutive patients (group A) underwent lateral UKR at our institution with the Oxford domed lateral component (Biomet UK Limited, Swindon, UK) for isolated osteoarthritis of the lateral compartment and were followed prospectively. Previous osteotomy, an uncorrectable valgus deformity, insufficiency of the ACL and a flexion deformity > 15° were considered contraindications; patellofemoral osteoarthritis was not considered a contraindication unless there was deep eburnation and grooving. Patients underwent a standardised clinical and radiographic workup preoperatively, three and 12 months postoperatively and annually thereafter using the Oxford Knee Score (OKS) [23]. Pain was assessed using the visual analogue scale (VAS) ranging from 0 to 10 (0 = no pain; 10 = worst pain ever). Range of motion (ROM) and any necessary reoperations were recorded. In order to create equal conditions for the clinical assessment, we used standardised questionnaires and examination forms pre- and postoperatively for all patients.
With the help of our prospective institutional database, patients were matched with 254 consecutive patients (group B) who had undergone cruciate-retaining TKR for isolated osteoarthritis of the lateral compartment between 2001 and 2009. In all cases, the fixed-bearing cruciate-retaining PFC Sigma (DePuy, Kirkel, Germany) was implanted. Patients with an insufficiency of the posterior cruciate ligament (PCL) or collateral ligaments who required a posterior-stabilised implant were not included. The follow-up regimen was the same as in group A. Exclusion criteria for both groups were missing data or severe osteoarthritis in the medial compartment in order to create equal conditions. Patients were matched in terms of gender, age and body mass index (BMI). Patients were divided into six age groups: < 50, 50–54, 55–59, 60–64, 65–70, > 70 years, with a maximum difference of five years; for BMI they were divided into three groups: < 25, 25–30, > 30 kg/m2. To create matched pairs, patients had to be the same gender and in the same group for age and BMI [24].
We used a standardised operative technique with a midline incision and a medial parapatellar approach and patellar eversion for TKR, and the patella was selectively resurfaced when advanced degenerative changes with deep eburnation and grooving were seen intraoperatively. UKR was performed by a lateral parapatellar incision, and the anterior cruciate ligament (ACL) and medial compartment were inspected to ensure indication for UKR. In both groups components were fixed with cement (Refobacin bone cement R; Biomet, Berlin, Germany). Intravenously administered cefuroxime (1.5 g Zinacef; GlaxoSmith-Kline, London, UK) was administered perioperatively. Anticoagulation treatment consisted of low-molecular-weight heparin administered subcutaneously the day before surgery and was continued for five weeks postoperatively. Full weight bearing was allowed under supervision of a physiotherapist as soon as tolerated, and outpatient physiotherapy was carried on to ensure adequate ROM and strength.
All data were recorded and analysed using SPSS® Version 17.0 (SPSS Inc., Chicago, IL, USA) and Graphpad Prism® Version 5.0 (Graphpad Software, San Diego, CA, USA). Wilcoxon and Mann–Whitney tests were used to test statistical significance of the difference in clinical outcomes. We considered p values of < 0.05 to be significant. Kaplan–Maier survivorship analysis was performed, with the endpoint being revision for any reason (defined as operation with exchange of at least one of the components). To compare survival rates of both groups, the Log-rank test was used, and p <0.05 was considered significant.
Results
We were able to match 22 patients after mobile-bearing lateral UKR (group A) to patients after cruciate-retaining TKR (group B) for isolated osteoarthritis of the lateral compartment regarding parameters gender, age and BMI, as described. Patient demographic data are shown in Table 1.
While there were no statistically significant differences in mean preoperative OKS and ROM between groups, postoperative mean OKS and ROM were statistically significantly higher in group A (p < 0.05). Additionally, changes in OKS and ROM were statistically significantly higher in group A (p < 0.05) (Table 2, Figs. 2 and 3).
Pre- and postoperative Oxford Knee Score (OKS) of patients following unicompartmental knee replacement (UKR) and cruciate-retaining total knee replacement (TKR): patients following UKR had a statistically significantly higher postoperative mean OKS score, while there was no difference in preoperative score; *p < 0.05
Pre- and postoperative range of motion (ROM) of patients following unicompartmental knee replacement (UKR) and cruciate-retaining total knee replacement (TKR). Patients following UKR had a statistically significantly higher postoperative mean range of motion (ROM), while there was no difference in preoperative ROM; ***p < 0.001
Regarding postoperative pain level, we found no statistically significant difference (p = 0.055). Mean pain level in patients in group A was 1.2 ± 2 (range 0–9) and in patients in group B 2.5 ± 2.3 (range 0–7). In group A, one patient had early wound dehiscence and positive cultures for methicillin-resistant Staphylococcus aureus (MRSA); multiple lavages were performed, and the bearing was finally exchanged. This was the only patient in group A with a revision and exchange of one component. No revision was necessary in group B. Kaplan–Maier survival at two years, with revision for any reason as the endpoint, was 96 % [95 % confidence interval (CI) 72–99] in group A and 100 % in group B. There was no statistically significant difference in survival rates (Log-rank test, p = 0.317).
Discussion
Our study is the first comparing functional outcome of patients following UKR and cruciate-retaining TKR for isolated osteoarthritis in the lateral compartment. As previous studies mostly refer to absolute postoperative clinical outcome scores, ignoring the often higher preoperative clinical scores in patients with UKR, our data demonstrates a significantly higher change in OKS and ROM, as this is seen as determining the effectiveness of such a procedure [8]. As our patients were matched regarding age, gender and BMI, it is legal to assume that there was no influence on differences regarding the clinical outcome between both groups by these parameters.
The optimal treatment of isolated osteoarthritis of the knee joint remains controversial [8, 25]. TKR has been considered an effective treatment regarding predictability, durability, pain reduction and restoration of function, with high survival rates ranging from 91 % to 98.9 % at five to 19 years [8]. Despite its success, TKR can be associated with high postoperative morbidity and complications, such as postoperative pain, extensive rehabilitation, cardiac and pulmonary complications, infection, venous thromboembolic disease, admission to an intermediate care unit, higher risk for blood transfusion or manipulation under anaesthetic, longer hospital stay and joint stiffness [7, 26–28]. Moreover, several trials report a high percentage of unsure or dissatisfied patients after TKR (up to 20 %), most of them with seemingly well-fixed and well-positioned components [29–33]. UKR is considered to have some potential advantages, including less bone resection, preservation of the cruciate ligaments, greater ROM, faster recovery and a lower postoperative morbidity rate [3–7, 10–12, 15, 26]. On the contrary, there are also disadvantages of UKR, such as the risk of disease progression in the contralateral or retropatellar compartment and risk of dislocation of the mobile bearing [3, 8]. Further, there are some important contraindications to UKR, such as inflammatory arthritis, flexion or varus deformity >15° and damage to the cruciate mechanism. In general, revision rates after lateral UKR might be higher when compared with TKR [8, 18, 19, 34–36]. There are several retrospective and prospective studies comparing the clinical results of TKR with UKR, mainly of the medial compartment, demonstrating a superiority of UKR [2, 3, 8, 25, 37]. Newman et al. demonstrated a statistically significant greater ROM following medial UKR in a prospective randomised study of 102 knees suitable for UKR and TKR. Nevertheless, there was no statistically significant difference in the Bristol scoring system [2]. In a database analysis by Lyons et al. of 5,606 TKR and 279 UKR, patients with UKR had higher postoperative function according to the Western Ontario McMaster Universities Osteoarthritis Index (WOMAC) as well as the SF-12 Health Survey score. Regarding change of scores alone, there was no statistically significant difference between groups, as preoperative scores were higher in patients with UKR [8]. As the change in score determines the effect of the treatment, both interventions were considered equally effective by those authors [8]. In a matched-pairs study of 54 TKR and UKR, Amin et al. demonstrated a greater active ROM after UKR than after TKR [3]. As these patients were matched for preoperative ROM and OKS, UKR seemed to be more effective regarding postoperative knee function [3]. Similar results were demonstrated by Manzotti et al. In their matched-pair study of 34 patients after medial UKR and TKR, the postoperative Knee Society functional score was significantly higher in patients following UKR while the preoperative score was not [25].
In our study, patients after cruciate-retaining TKR achieved a mean postoperative OKS of 37 ± 9 and ROM of 107° ± 17, which is consistent with previous published data for the device used in this series. Keenan et al. reported a mean OKS of 36 5 years after TKR using the PFC prosthesis [32] and Hanusch et al. a mean OKS of 38.6 and ROM of 100.8° one year after implantation of the PFC prosthesis [34]. As previously described, we used a cruciate-retaining TKR in our study. There are several studies comparing functional outcome after posterior-stabilised TKR and cruciate-retaining TKR. Maruyama et al. reported the results of 20 patients with a cruciate-retaining TKR in one knee and a posterior-stabilised TKR in the other. While there were no significant differences in postoperative knee scores, ROM improvement was significantly superior in the posterior-stabilised group [38]. Similar results were described by Bercik et al. [39]. In their meta-analysis of 12 studies with 1,265 knees, a significant difference in flexion and ROM in favour of posterior-stabilised TKR was reported [39]. In a Cochrane review, 17 randomised controlled trials (with 1,810 patients and 2,206 knees) were analysed. Again, ROM was statistically significantly higher in posterior-stabilised patients. Nevertheless, the conclusion by the authors was that this difference is not clinically relevant [40].
For patients following UKR, we demonstrated a mean postoperative OKS of 43 ± 4 and ROM of 127° ± 13. Again, these results are consistent with previously published data. Altuntas et al. reported a mean OKS of 42 at two years, Schelfaut et al. a mean OKS of 42 and ROM of 127° at 20 months, Weston-Simons et al. a mean OKS of 40 at four years and Pandit et al. a mean OKS of 41 and ROM of 125° 2.3 years after surgery [18, 20–22].
We demonstrated that patients following Oxford UKR for isolated osteoarthritis in the lateral compartment achieved a statistically significantly higher mean score postoperatively on the OKS as well as a higher ROM (Figs. 2 and 3) than a matched group of patients following cruciate-retaining TKR, although there were no statistically significant differences in preoperative scores. Additionally, changes in score—seen as the determination of effectiveness of such treatment [8]—for OKS and ROM were significantly higher in patients after UKR than cruciate-retaining TKR.
Advocates of TKR often refer to the higher revision rate in patients following UKR. In a database search by Lyons et al., a higher cumulative revision rate for UKR in general with a survival rate ranging from 82 % to 98 % at five to 22 years compared with a survival rate ranging from 91 % to 98.9 % at five to 19 years after TKR is reported [8]. For the PFC Sigma, which was used in our study, Arthur et al. reported a survival rate of 95.9 % in 203 patients after ten years with the endpoint being revision for any reason [33], Zaki et al. a survival rate of 99.4 % after eight years in 156 patients [36] and Dalury et al. a survival rate of 99.6 % seven years after surgery in 207 patients [35]. For the Oxford UKR used in the lateral compartment, we demonstrated a survival rate at three years with revision for any reason of 94 % in 50 patients [19], Pandit et al. a survival rate of 98 % at four years in a series of 101 implants [18] and Marson et al. a survival rate of 90 % at four years in a small series of 12 implants [41]. Schelfaut et al. demonstrated a revision rate of 8 % in 25 procedures with a minimum follow-up of one year [20], and Altuntas et al. demonstrated a revision rate of 3.1 % in 64 implants with a mean follow-up of 38 months [21]. At eight years, Weston-Simons et al. demonstrated a survival rate of 92.1 % in a consecutive series of 265 patients [22]. However, long-term studies for this procedure are not available at present. We demonstrated a survival rate with the endpoint being revision for any reason and exchange of one of the components of 96 % for UKR and 100 % for cruciate-retaining TKR after two years, showing no statistically significant difference. Our findings are consistent with contemporary data in the literature, as described above.
There are several limitations to this study: the short follow-up with a mean of 22 months and 19 months, respectively, as well as the relatively small group of patients. Additionally, patients after TKR had to be reviewed at our institution at least once after operation for inclusion in this study. Even if all patients after knee arthroplasty were invited to regular clinical and radiological follow-up as standard practice, patients with an unsatisfying result are more likely to attend these regular follow-ups than patients who are completely free of complaints. This could cause a potential bias to worse results in the group of patients following TKR.
In conclusion, mobile-bearing UKR in the lateral compartment seems to provide a superior functional outcome compared with a cruciate-retaining TKR for isolated osteoarthritis of the lateral compartment. While short-term survival with the endpoint being revision for any reason at two years was not significantly different in this series, longer-term follow-up is needed to compare survival and complications of both procedures and assess their safety. From the data available, we expect a slightly higher revision rate after UKR. However, lateral UKR could be considered especially in patients with a high demand for postoperative function of the knee joint, regardless of age and gender.
References
Parsch D, Kruger M, Moser MT, Geiger F (2009) Follow-up of 11–16 years after modular fixed-bearing TKA. Int Orthop 33(2):431–435. doi:10.1007/s00264-008-0543-x
Newman JH, Ackroyd CE, Shah NA (1998) Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg (Br) 80(5):862–865
Amin AK, Patton JT, Cook RE, Gaston M, Brenkel IJ (2006) Unicompartmental or total knee arthroplasty?: Results from a matched study. Clin Orthop Relat Res 451:101–106. doi:10.1097/01.blo.0000224052.01873.20
Servien E, Aitsiselmi T, Neyret P, Verdonk P (2008) How to select candidates for lateral unicompartmental prosthesis. Curr Orthop Pract 19 (4):451–458 410.1097
Heyse TJ, Tibesku CO (2010) Lateral unicompartmental knee arthroplasty: a review. Arch Orthop Trauma Surg 130(12):1539–1548. doi:10.1007/s00402-010-1137-9
Knutson K, Robertsson O (2010) The Swedish Knee Arthroplasty Register. Acta Orthop 81(1):5–7. doi:10.3109/17453671003667267
Robertsson O, Borgquist L, Knutson K, Lewold S, Lidgren L (1999) Use of unicompartmental instead of tricompartmental prostheses for unicompartmental arthrosis in the knee is a cost-effective alternative. 15,437 primary tricompartmental prostheses were compared with 10,624 primary medial or lateral unicompartmental prostheses. Acta Orthop Scand 70(2):170–175
Lyons MC, MacDonald SJ, Somerville LE, Naudie DD, McCalden RW (2012) Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res 470(1):84–90. doi:10.1007/s11999-011-2144-z
Price AJ, Webb J, Topf H, Dodd CA, Goodfellow JW, Murray DW, Oxford H, Knee G (2001) Rapid recovery after oxford unicompartmental arthroplasty through a short incision. J Arthroplasty 16(8):970–976
Walton NP, Jahromi I, Lewis PL, Dobson PJ, Angel KR, Campbell DG (2006) Patient-perceived outcomes and return to sport and work: TKA versus mini-incision unicompartmental knee arthroplasty. J Knee Surg 19(2):112–116
Newman J, Pydisetty RV, Ackroyd C (2009) Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg (Br) 91(1):52–57. doi:10.1302/0301-620X.91B1.20899
Ollivier M, Abdel MP, Parratte S, Argenson JN (2014) Lateral unicondylar knee arthroplasty (UKA): contemporary indications, surgical technique, and results. Int Orthop 38(2):449–455. doi:10.1007/s00264-013-2222-9
Victor J, Ghijselings S, Tajdar F, Van Damme G, Deprez P, Arnout N, Van Der Straeten C (2014) Total knee arthroplasty at 15–17 years: does implant design affect outcome? Int Orthop 38(2):235–241. doi:10.1007/s00264-013-2231-8
Pandit H, Jenkins C, Barker K, Dodd CA, Murray DW (2006) The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg (Br) 88(1):54–60. doi:10.1302/0301-620X.88B1.17114
Price AJ, Svard U (2011) A second decade lifetable survival analysis of the Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res 469(1):174–179. doi:10.1007/s11999-010-1506-2
Svard UC, Price AJ (2001) Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg Br 83(2):191–194
Gunther TV, Murray DW, Miller R, Wallace DA, Carr AJ, O'Connor JJ, McLardy-Smith P, Goodfellow JW (1996) Lateral unicompartmental arthroplasty with the Oxford meniscal knee. Knee 3(1–2):33–39
Pandit H, Jenkins C, Beard DJ, Price AJ, Gill HS, Dodd CA, Murray DW (2010) Mobile bearing dislocation in lateral unicompartmental knee replacement. Knee 17(6):392–397. doi:10.1016/j.knee.2009.10.007
Streit MR, Walker T, Bruckner T, Merle C, Kretzer JP, Clarius M, Aldinger PR, Gotterbarm T (2012) Mobile-bearing lateral unicompartmental knee replacement with the Oxford domed tibial component: an independent series. J Bone Joint Surg (Br) 94(10):1356–1361. doi:10.1302/0301-620X.94B10.29119
Schelfaut S, Beckers L, Verdonk P, Bellemans J, Victor J (2013) The risk of bearing dislocation in lateral unicompartmental knee arthroplasty using a mobile biconcave design. Knee Surg Sports Traumatol Arthrosc 21(11):2487–2494. doi:10.1007/s00167-012-2171-7
Altuntas AO, Alsop H, Cobb JP (2013) Early results of a domed tibia, mobile bearing lateral unicompartmental knee arthroplasty from an independent centre. Knee 20(6):466–470. doi:10.1016/j.knee.2012.11.008
Weston-Simons JS, Pandit H, Kendrick BJ, Jenkins C, Barker K, Dodd CA, Murray DW (2014) The mid-term outcomes of the Oxford Domed Lateral unicompartmental knee replacement. Bone Joint J 96-B(1):59–64. doi:10.1302/0301-620X.96B1.31630
Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ, Dawson J (2007) The use of the Oxford hip and knee scores. J Bone Joint Surg (Br) 89(8):1010–1014. doi:10.1302/0301-620X.89B8.19424
Duwelius PJ, Burkhart RL, Hayhurst JO, Moller H, Butler JB (2007) Comparison of the 2-incision and mini-incision posterior total hip arthroplasty technique: a retrospective match-pair controlled study. J Arthroplasty 22(1):48–56. doi:10.1016/j.arth.2006.09.012
Manzotti A, Confalonieri N, Pullen C (2007) Unicompartmental versus computer-assisted total knee replacement for medial compartment knee arthritis: a matched paired study. Int Orthop 31(3):315–319. doi:10.1007/s00264-006-0184-x
Brown NM, Sheth NP, Davis K, Berend ME, Lombardi AV, Berend KR, Della Valle CJ (2012) Total knee arthroplasty has higher postoperative morbidity than unicompartmental knee arthroplasty: a multicenter analysis. J Arthroplasty 27(8 Suppl):86–90. doi:10.1016/j.arth.2012.03.022
Lombardi AV Jr, Berend KR, Walter CA, Aziz-Jacobo J, Cheney NA (2009) Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop Relat Res 467(6):1450–1457. doi:10.1007/s11999-009-0731-z
Yang KY, Wang MC, Yeo SJ, Lo NN (2003) Minimally invasive unicondylar versus total condylar knee arthroplasty–early results of a matched-pair comparison. Singap Med J 44(11):559–562
Scott CE, Howie CR, MacDonald D, Biant LC (2010) Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg (Br) 92(9):1253–1258. doi:10.1302/0301-620X.92B9.24394
Parvizi J, Nunley RM, Berend KR, Lombardi AV Jr, Ruh EL, Clohisy JC, Hamilton WG, Della Valle CJ, Barrack RL (2014) High level of residual symptoms in young patients after total knee arthroplasty. Clin Orthop Relat Res 472(1):133–137. doi:10.1007/s11999-013-3229-7
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63. doi:10.1007/s11999-009-1119-9
Keenan AC, Wood AM, Arthur CA, Jenkins PJ, Brenkel IJ, Walmsley PJ (2012) Ten-year survival of cemented total knee replacement in patients aged less than 55 years. J Bone Joint Surg (Br) 94(7):928–931. doi:10.1302/0301-620X.94B7.27031
Arthur CH, Wood AM, Keenan AC, Clayton RA, Walmsley P, Brenkel I (2013) Ten-year results of the Press Fit Condylar Sigma total knee replacement. Bone Joint J 95-B(2):177–180. doi:10.1302/0301-620X.95B2.29695
Hanusch B, Lou TN, Warriner G, Hui A, Gregg P (2010) Functional outcome of PFC Sigma fixed and rotating-platform total knee arthroplasty. A prospective randomised controlled trial. Int Orthop 34(3):349–354. doi:10.1007/s00264-009-0901-3
Dalury DF, Gonzales RA, Adams MJ, Gruen TA, Trier K (2008) Midterm results with the PFC Sigma total knee arthroplasty system. J Arthroplasty 23(2):175–181. doi:10.1016/j.arth.2007.03.039
Zaki SH, Rafiq I, Kapoor A, Raut V, Gambhir AK, Porter ML (2007) Medium-term results with the Press Fit Condylar (PFC) Sigma knee prosthesis the Wrightington experience. Acta Orthop Belg 73(1):55–59
Laurencin CT, Zelicof SB, Scott RD, Ewald FC (1991) Unicompartmental versus total knee arthroplasty in the same patient. A comparative study. Clin Orthop Relat Res 273:151–156
Maruyama S, Yoshiya S, Matsui N, Kuroda R, Kurosaka M (2004) Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty 19(3):349–353
Bercik MJ, Joshi A, Parvizi J (2013) Posterior cruciate-retaining versus posterior-stabilized total knee arthroplasty: a meta-analysis. J Arthroplasty 28(3):439–444. doi:10.1016/j.arth.2012.08.008
Verra WC, van den Boom LG, Jacobs W, Clement DJ, Wymenga AA, Nelissen RG (2013) Retention versus sacrifice of the posterior cruciate ligament in total knee arthroplasty for treating osteoarthritis. Cochrane Database Syst Rev 10, CD004803. doi:10.1002/14651858.CD004803.pub3
Marson B, Prasad N, Jenkins R, Lewis M (2013) Lateral unicompartmental knee replacements: early results from a District General Hospital. Eur J Orthop Surg Traumatol. doi:10.1007/s00590-013-1277-z
Conflict of interest
MRS was supported by the noncommercial research fund of Deutsche-Arthrose-Hilfe e.v. In addition, benefits were directed to a research fund by Biomet, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walker, T., Gotterbarm, T., Bruckner, T. et al. Total versus unicompartmental knee replacement for isolated lateral osteoarthritis: a matched-pairs study. International Orthopaedics (SICOT) 38, 2259–2264 (2014). https://doi.org/10.1007/s00264-014-2473-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2473-0