Abstract
Purpose
Desmoid tumours of the extremity have a high recurrence rate. The purpose of this study was to analyse the outcome after resection of these tumours with special emphasis on recurrent disease and adjuvant therapeutic strategies.
Methods
In this retrospective study we evaluated prognostic factors for recurrence-free survival after surgical treatment of desmoid tumours of the extremity in 27 patients with an average age of 41 years treated from 1997 to 2009. Adjuvant radiotherapy (50–60 Gy) was given in five cases with primary and in nine patients with recurrent disease. The average follow-up was 64 months.
Results
The five-year recurrence-free survival in patients with primary disease was 33 %. Patients with negative resection margins tended to have a better outcome than patients with positive resection margins, but the difference between both groups was not significant (56 vs 14 %, p = 0.145). In patients with positive margins, adjuvant radiotherapy did not significantly improve recurrence-free survival (40 vs 14 %, p = 0.523). Patients with local recurrence had a five-year further recurrence-free survival of 47 %. In those patients further recurrence-free survival was significantly better after adjuvant radiation (89 vs 25 %, p = 0.015). Two thirds of all patients suffered moderate or severe complications due to the treatment regimen.
Conclusions
Compared to desmoids of the trunk or the head and neck region, desmoids affecting the limbs show by far the worst outcome in terms of relapse or treatment-related morbidity. The importance of negative resection margins is still not clear. Particularly in recurrent desmoids adjuvant radiotherapy appears to reduce the further recurrence rate. Therefore, a general use of radiation should be considered for this high-risk group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Desmoid tumours (synonym: desmoids, aggressive fibromatosis) are slowly growing neoplasms that arise from deep musculo-aponeurotic structures. The incidence of the tumour is 2–5 cases per 1,000,000 per year [1, 2]; most patients are between 25 and 35 years old and approximately two thirds of them are female [3–7]. Desmoids lack cytological features of malignancy and have basically no metastatic potential, but they do show locally aggressive and infiltrative behaviour, resulting in a remarkable propensity to cause local recurrence [1, 8].
Treatment strategies include surgical resection, adjuvant or exclusive radiotherapy and systemic medical treatment including non-steroidal anti-inflammatory drugs (NSAIDs), hormonal agents, cytotoxic chemotherapy, interferons and tyrosine kinase inhibitors [9]. As aggressive fibromatosis was reported to occasionally show spontaneous stabilisation or regression [10], even watchful waiting seems to be applicable under certain circumstances. To date, the rarity of the tumour and the heterogenic biological behaviour precluded identification of standardised treatment protocols. Whether negative resection margins reduce the risk of recurrence remains unclear [11]. However, a wide and local resection of the tumour is still the preferred treatment modality. Radiotherapy is mostly used as an adjunct, providing beneficial results especially in recurrent disease [7, 12].
A significant proportion of patients suffer from local recurrence after initial surgery. With the evolution of combined treatment modalities recurrence rates have improved over the last few decades and have been reported to be 17–30 % (overall five-year recurrence rate) [3–7, 13]. The localisation of the tumour seems to have a major impact on the likelihood of local recurrence. Analyses of subgroups unveiled favourable outcomes for patients with trunk-localised tumours, whereas the recurrence rate of desmoids located in the extremities is still dramatically higher, reaching up to 80 % [3, 4, 14].
Bearing in mind that surgery of desmoids of the extremities, which are frequently located in close proximity to neurovascular structures and muscles, is especially mutilating [14, 15], more attention should be paid to this group of tumours. Therefore, the purpose of this study was to exclusively analyse the outcome of patients with extremity desmoids with special regard to adjuvant radiation and recurrent disease.
Patients and methods
Institutional Review Board approval had been obtained before initiation of the study. From the unit’s tumour database we identified 58 patients referred to our institution between 1997 and 2009 under the initial diagnosis of either a desmoid tumour or aggressive fibromatosis. Of those, 31 patients had a tumour of the upper or lower limb and were enrolled in the study. Since four patients were lost to follow-up a total of 27 patients were investigated (Table 1).
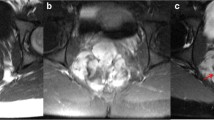
Patient demographics, including gender and age, history of trauma or previous operations in the tumour affected area instead of in the affected area and predisposing or concomitant diseases were prospectively collected and saved in our tumour database. Other factors analysed included the characteristics of the tumour, clinical presentation, surgical resection margins, pre- and post-operative morbidity, surgical complications and use of adjuvant therapies. Tumour characteristics examined included the location, size and depth of the tumour. Tumour size was determined by the greatest dimension of the tumour in the preoperative magnetic resonance imaging (MRI) scan. Resection margins of the tumour were assessed by histopathological examination (microscopic margins) and were considered as follows: R0 if the margin of the resected specimen was free of tumour, R1 if the tumour was identified at the inked margin of the specimen (microscopic margins positive) and R2 if the macroscopically detectable tumour reached the margins of the specimen [16]. If radiation was administered, the total dose and the technique were assessed and adjuvant drug treatment was documented. The indication for adjuvant radiotherapy was discussed before the intervention with the collaborating radiotherapist and the patient. Desmoids close to functionally important structures and with expected positive resection margins after surgery were more likely to undergo adjuvant radiotherapy especially in recurrent disease. Complication rates, e.g. treatment-associated morbidity, and satisfaction of the patients were evaluated. Complications were classified according to Goy et al. [15]: mild (oedema, pain without the need for analgesics, restriction of movement, paraesthesia), moderate (need for plastic surgery, use of analgesics, restriction of movement affecting everyday life) and severe (amputation, reduction of earning capacity).
Patients were divided into primary and recurrent disease groups and each group was analysed separately. All patients were followed up by MRI and recurrence was defined as a detectable tumour mass. Recurrence-free survival was calculated by the Kaplan-Meier method. If no relapse occurred, survival was calculated from the time of surgery to the last day of data acquisition. In cases of recurrence and reoperation in primary disease, the new operation date was set to zero, the patient changed to recurrent disease and further recurrence-free survival was determined accordingly. The log-rank test was used to determine whether the differences in survival between groups were significantly different. The level of significance was set at p ≤ 0.05.
Results
Of 27 patients, 21 presented with a primary lesion without any previous treatment and six with recurrent disease previously treated elsewhere. The average age of the patients was 41 years, 16 patients were male (59 %). The median follow-up for the entire group of patients was 65 months. All 27 patients underwent resection of the desmoids in our institution. In total 16 patients received adjuvant radiation with a cumulative dose between 50 and 60 Gy, and one patient was treated by intraoperative radiation therapy with 12 Gy. The initial clinical manifestation of the disease was pain in 14 patients, restriction of movement in eight or both in five patients and nine patients reported a previous history of trauma or surgery at the location of the later tumour.
Twenty-one patients with primary lesions were allocated to the primary therapy group. Of those, 11 patients suffered recurrent disease and were analysed within the recurrent disease group after reoperation (Fig. 1).
Primary patients treated for a primary lesion, Recurrence patients treated suffering recurrent disease. Of the 21 patients with primary lesions, 11 had a relapse. Those 11 patients were added to the recurrence group after reoperation. Six patients initially presented with recurrent disease after resection in another institution
Primary disease
Of the 21 patients with primary lesions, 12 (57 %) were male. The five-year disease-free survival of the whole group was 33 % (95 % confidence interval 22 – 44 %, Fig. 2). Macroscopically, all tumours were resected in toto; nine patients revealed negative margins (R0), whereas in 12 cases the histopathological evaluation revealed positive margins (R1). Of the nine R0-resected patients none underwent adjuvant radiation. Five patients stayed disease free during follow-up, and four had a local recurrence and underwent reoperation at our institution.
Of the 12 patients with R1 resection, seven patients underwent no further treatment. Only one of them remained disease free during follow-up (14 %). Adjuvant radiation was given in the remaining five patients. Of those, two patients (40 %) stayed disease free.
Summarising the results of patients treated by surgery without adjuvant radiation (16 patients, nine R0, seven R1), ten patients (63 %, composed of four R0 and six R1) developed a local recurrence. Patients with R0 status had a higher recurrence-free survival rate than patients with R1 resection status; however, the difference was not significant (p = 0.145).
Comparing the results of patients with R1-resected tumours with and without radiation of the primary tumour, adjuvant radiation seemed to improve the recurrence-free survival (recurrence-free survival of 40 vs 14 %), although these results were not statistically significant (p = 0.523). There was no statistically significant difference in survival rates between male or female patients (female 67 vs male 58 %, p = 0.53). A summary of the results of patients after primary treatment is displayed in Table 2. Overall, 13 of the 21 patients with primary disease sustained recurrence; 11 of them underwent repeated surgery at our institution. Two patients chose a medical treatment without surgery (both sulindac and tamoxifen). One desmoid was stable at follow-up for 26 months, and the other one showed progression in the control MRI scan after five months.
Recurrent disease
In 11 patients of the recurrent disease group the primary surgical intervention was performed at our institution, whereas six were primarily treated elsewhere (total of 17 patients). Ten patients (59 %) were male. In this group the five-year re-recurrence-free survival was 47 % (95 % confidence interval 31 – 63 %, Fig. 3). Eight patients in the recurrent disease group were treated by re-operation without adjuvant radiation (four R0, four R1). Adjuvant radiation was given in nine cases (two R0, seven R1).
Adjuvant radiotherapy led to a significantly lower rate of further recurrence (further recurrence-free survival 25 vs 89 %, p = 0.015). As seen in the primary treatment group, no gender differences were evident (43 vs 50 % further recurrences, p = 0.617). Of all 17 patients with relapse, eight suffered re-recurrence. Three patients had three relapses and one patient even four. Six of the eight further recurrences underwent subsequent resections and have now been free of disease for at least 12 months. A summary of the results of the recurrent disease group is displayed in Table 3.
Treatment-associated morbidity
Of 27 patients, 18 (67 %) experienced treatment-associated complications (Table 4); 7 % of them were classified as severe. Most commonly (in 12 patients) there was a restriction of movement of the operated limb, which was disabling in everyday life in nine cases. In one patient amputation of the lower leg was necessary due to extensive growth of the tumour that also affected the neurovascular bundle. In two patients a plastic surgeon was involved to cover larger skin lesions with a local flap.
Discussion
Treatment of desmoid tumours remains challenging. As therapeutic options extend from “watchful waiting” to radical resection, radiation and administration of chemotherapy, it is difficult to recommend one standard therapeutic strategy. Surgical resection still represents the therapeutic mainstay [6, 14], but due to the high propensity to develop local recurrence in combination with severe functional and aesthetic consequences, doubts have been raised whether every desmoid should be resected. Moreover, the observation of spontaneous regression in some rare cases and the tumour’s lack of metastatic potential lead surgeons to reconsider traditional treatment modalities [10, 17]. Efforts to identify prognostic factors have been the subject of recent research [3, 6, 14] and might be helpful in finding out whom and how to treat. Tumour location as a prognostic factor, with tumours of the extremities showing the worst outcome, has already been demonstrated [10, 14, 18–20]. While the five-year overall recurrence rate, including tumours located in the trunk, has improved and has been described to be between 17 and 30 % [4, 6, 7, 21], the recurrence rate of limb desmoids is nearly twice as high [3, 4]. Desmoids of the extremities commonly grow near functionally relevant structures including nerves or vessels or even infiltrate them. To avoid morbidity, resection might be less radical with the potential for higher recurrence rates. Whether the extent of surgery itself has an impact on recurrence rates is still unclear. Some authors found significant advantages for R0-resected patients [3, 7]; other series concerning primary disease have not found any differences [4, 6]. Interestingly, Salas et al. were able to show a highly significant disadvantage for patients after R2 resection (macroscopic residual tumour), with patients after R0 and R1 resection having the same outcome [14]. The results are probably due to the fact that desmoid tumours readily infiltrate locally, causing difficulties in properly assessing microscopic margins [4]. Thus, function-sparing surgery should be preferred to tumour-free resection margins. In general, 66 % of all patients suffering from aggressive fibromatosis are female [3, 4, 6]. Women tend to develop desmoids of the abdominal wall during or soon after pregnancy or under contraceptive medication, which frequently show spontaneous regression after menopause and easier surgical accessibility [22, 23]. In consequence, women were supposed to have a better outcomes [22]. Concerning limb localisation and recurrence rates, the majority of studies did not find any sex-related differences [3, 6, 7]. In our patients the male portion was remarkably high. This might have influenced the conclusions based on our findings. Age as a prognostic factor has been studied in several publications, basically without any prognostic influence [3–6]. Evidence for negative outcome in younger patients is sparse [7, 14, 19]; one survey associated higher age with poor outcome [10]. Furthermore, the efficacy of radiation therapy is still unclear. Though local control rates of 76–100 % in primary tumours have been reported in small series [3, 5, 7], most authors see radiation as an adjunct to surgery. In two large retrospective studies the idea of enhancing local control via adjuvant radiation did not result in any significant advantage compared to surgery alone [5, 6]; notably both series showed comparatively low recurrence rates in cases of R1 status without radiation (between 17 and 23 %). In our study, adjuvant radiation led to a significant benefit in patients with recurrent disease. As mentioned before, neither resection status nor adjuvant radiation seem to alter the outcome significantly in primary disease, but at least secondarily could play important roles in the treatment of recurrent tumours.
In the literature, there are no standard recommendations for the use of radiotherapy as an adjuvant therapeutic strategy. Most authors favour the use of radiotherapy in cases where the tumour grows in close proximity to neurovascular structures and where the resection results in tumour-positive margins. Some recommend radiotherapy also in cases where the tumour shows a multifocal and highly infiltrative growth pattern. However, the benefit remains controversial with difficulties in implementing unequivocally articulated indications and variations of energy sources and dosages [5]. Finally, the surgeon has to reconcile his arguments with the attitude of the patient towards an adjuvant therapeutic regimen. In our patient cohort, no R0-resected patient received radiation therapy. In recurrent disease, our decision to use radiation therapy was influenced more by the tumour location than the expected resection status. Therefore, some R0-resected patients with recurrent disease received radiotherapy.
Further resection is the most common treatment option for recurrent desmoids. It has been shown that control rates are similar or lower than in patients with primary disease [6, 24, 25]. This was confirmed by our results.
More than two thirds of our patients suffered treatment-associated complications, mostly graded as moderate or severe. Due to the close relationship between tumour and neurovascular structures in limb-affecting desmoids the risk for treatment-associated complications is relatively high. To date, only Goy et al. have considered this aspect and described complications in one third of their patients [15]. Being aware that only 28 % of their patients showed limb-affecting desmoids, the difficulty in treating aggressive fibromatosis of the extremities is compounded by an increased treatment-associated morbidity.
In summary, desmoids of the extremities have a high rate of recurrence and surgical treatment of these tumours is associated with a high rate of complications. Bearing in mind that most patients are under 35 years of age and the tumour shows no metastatic potential and in some rare cases stabilises without treatment, the main question of how the primary disease should be managed is still not answered. A wait and see policy, primary radiation or medical treatment include the risk of reducing the surgical resectability and are of doubtful value. In cases of recurrent disease, adjuvant radiotherapy seems to help irrespective of the resection margin. In primary disease the benefit of radiotherapy has yet to be proven. In conclusion, the therapeutic decision has to integrate the attitude of the patient and the morbidity associated with the surgical treatment. Prospective, randomised clinical studies with a higher number of patients must follow to develop general therapeutic recommendations.
References
Escobar C, Munker R, Thomas JO, Li BD, Burton GV (2012) Update on desmoid tumors. Ann Oncol 23:562–569
Piza-Katzer H, Rhomberg M (2000) Extra-abdominal fibromatosis–extra-abdominal desmoid. Review and personal experiences. Chirurg 71:904–911
Ballo MT, Zagars GK, Pollack A, Pisters PW, Pollack RA (1999) Desmoid tumor: prognostic factors and outcome after surgery, radiation therapy, or combined surgery and radiation therapy. J Clin Oncol 17:158–167
Gronchi A, Casali PG, Mariani L, Lo Vullo S, Colecchia M, Lozza L, Bertulli R, Fiore M, Olmi P, Santinami M, Rosai J (2003) Quality of surgery and outcome in extra-abdominal aggressive fibromatosis: a series of patients surgically treated at a single institution. J Clin Oncol 21:1390–1397
Lev D, Kotilingam D, Wei C, Ballo MT, Zagars GK, Pisters PW, Lazar AA, Patel SR, Benjamin RS, Pollock RE (2007) Optimizing treatment of desmoid tumors. J Clin Oncol 25:1785–1791
Merchant NB, Lewis JJ, Woodruff JM, Leung DH, Brennan MF (1999) Extremity and trunk desmoid tumors: a multifactorial analysis of outcome. Cancer 86:2045–2052
Spear MA, Jennings LC, Mankin HJ, Spiro IJ, Springfield DS, Gebhardt MC, Rosenberg AE, Efird JT, Suit HD (1998) Individualizing management of aggressive fibromatoses. Int J Radiat Oncol Biol Phys 40:637–645
Fletcher CD (2006) The evolving classification of soft tissue tumours: an update based on the new WHO classification. Histopathology 48:3–12
Janinis J, Patriki M, Vini L, Aravantinos G, Whelan JS (2003) The pharmacological treatment of aggressive fibromatosis: a systematic review. Ann Oncol 14:181–190
Rock MG, Pritchard DJ, Reiman HM, Soule EH, Brewster RC (1984) Extra-abdominal desmoid tumors. J Bone Joint Surg Am 66:1369–1374
Melis M, Zager JS, Sondak VK (2008) Multimodality management of desmoid tumors: how important is a negative surgical margin? J Surg Oncol 98:594–602
Nuyttens JJ, Rust PF, Thomas CR Jr, Turrisi AT 3rd (2000) Surgery versus radiation therapy for patients with aggressive fibromatosis or desmoid tumors: a comparative review of 22 articles. Cancer 88:1517–1523
Mankin HJ, Hornicek FJ, Springfield DS (2010) Extra-abdominal desmoid tumors: a report of 234 cases. J Surg Oncol 102:380–384
Salas S, Dufresne A, Bui B, Blay JY, Terrier P, Ranchere-Vince D, Bonvalot S, Stoeckle E, Guillou L, Le Cesne A, Oberlin O, Brouste V, Coindre JM (2011) Prognostic factors influencing progression-free survival determined from a series of sporadic desmoid tumors: a wait-and-see policy according to tumor presentation. J Clin Oncol 29:3553–3558
Goy BW, Lee SP, Eilber F, Dorey F, Eckardt J, Fu YS, Juillard GJ, Selch MT (1997) The role of adjuvant radiotherapy in the treatment of resectable desmoid tumors. Int J Radiat Oncol Biol Phys 39:659–665
Compton CC (2012) Soft tissue sarcoma. In: Compton CC, Byrd DR, Garcia-Aguilar J, Kurtzmann SH, Olawaiye A, Washington MK (eds) AJCC cancer staging atlas. A companion to the seventh editions of the AJCC cancer staging manual and handbook. Springer, New York
Barbier O, Anract P, Pluot E, Larouserie F, Sailhan F, Babinet A, Tomeno B (2010) Primary or recurring extra-abdominal desmoid fibromatosis: assessment of treatment by observation only. Orthop Traumatol Surg Res 96:884–889
Bonvalot S, Eldweny H, Haddad V, Rimareix F, Missenard G, Oberlin O, Vanel D, Terrier P, Blay JY, Le Cesne A, Le Pechoux C (2008) Extra-abdominal primary fibromatosis: aggressive management could be avoided in a subgroup of patients. Eur J Surg Oncol 34:462–468
Sørensen A, Keller J, Nielsen OS, Jensen OM (2002) Treatment of aggressive fibromatosis: a retrospective study of 72 patients followed for 1–27 years. Acta Orthop Scand 73:213–219
Stoeckle E, Coindre JM, Longy M, Binh MB, Kantor G, Kind M, de Lara CT, Avril A, Bonichon F, Bui BN (2009) A critical analysis of treatment strategies in desmoid tumours: a review of a series of 106 cases. Eur J Surg Oncol 35:129–134
Pritchard DJ, Nascimento AG, Petersen IA (1996) Local control of extra-abdominal desmoid tumors. J Bone Joint Surg Am 78:848–854
Huang K, Fu H, Shi YQ, Zhou Y, Du CY (2009) Prognostic factors for extra-abdominal and abdominal wall desmoids: a 20-year experience at a single institution. J Surg Oncol 100:563–569
Lewis JJ, Boland PJ, Leung DH, Woodruff JM, Brennan MF (1999) The enigma of desmoid tumors. Ann Surg 229:866–872, discussion 872–863
Posner MC, Shiu MH, Newsome JL, Hajdu SI, Gaynor JJ, Brennan MF (1989) The desmoid tumor. Not a benign disease. Arch Surg 124:191–196
Reitamo JJ, Scheinin TM, Häyry P (1986) The desmoid syndrome. New aspects in the cause, pathogenesis and treatment of the desmoid tumor. Am J Surg 151:230–237
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Prodinger, P.M., Rechl, H., Keller, M. et al. Surgical resection and radiation therapy of desmoid tumours of the extremities: results of a supra-regional tumour centre. International Orthopaedics (SICOT) 37, 1987–1993 (2013). https://doi.org/10.1007/s00264-013-1942-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-1942-1