Abstract
Purpose
The purpose of this study was to assess the safety and preliminary clinical results of platelet-rich plasma (PRP) injections for treating chronic plantar fasciitis.
Methods
Fourteen consecutive patients with chronic plantar fasciitis receiving three injections of PRP into the plantar fascia were assessed 12 months after the procedure. The modified Roles and Maudsley score and a visual analogue scale (VAS) for pain were used to evaluate the clinical results.
Results
According to criteria of the Roles and Maudsley score, at 12 months of follow-up, results were rated as excellent in nine (64.3 %), good in two (14.3 %), acceptable in two (14.3 %) and poor in one (7.1 %) patient. VAS for pain was significantly decreased from 7.1 ± 1.1 before treatment to 1.9 ± 1.5 at the last follow-up (p < 0.01).
Conclusions
In this single-centre, uncontrolled, prospective, preliminary study, results indicate that treating chronic plantar fasciitis with PRP injections is safe and has the potential to reduce pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic plantar fasciitis is a common problem that affects sport participants as well as inactive middle-aged individuals [6, 19]. In general, the condition is self-limiting, and the majority of cases spontaneously resolve regardless of type of intervention received (including placebo) [4]. Increasing knowledge of the pathology has led to the widespread application of a large number of conservative treatments for recalcitrant plantar fasciitis [16], including physiotherapy, plantar-fascia-stretching exercises [8], icepacks, night splints, prefabricated and custom-made insert, shoe modification, nonsteroidal anti-inflammatory drugs (NSAIDs) and extracorporeal shock-wave therapy (ESWT) when conventional physical therapy is not effective [23]. Although the effect of ESWT remains controversial, reliable evidence supports the use of this approach for treating chronic plantar fasciitis [12, 18]. However, adverse effects such as pain during treatment, soft-tissue damage (bleeding, hematoma, paresthesia), nausea, the need for peripheral nerve block and costs should be considered when proposing this procedure [26].
Recently, promising results were reported with the use of platelet-rich plasma (PRP) injections for treating muscle and tendon injuries and degeneration [9–13, 15, 21]. The rationale for using PRP is to increase tendon regenerative abilities with a high content of cytokines and cells, in hyperphysiologic doses, which should promote cellular chemotaxis, matrix synthesis, and proliferation [20]. Degranulation of the alpha granules in platelets releases many different growth factors that can play a role in tissue regeneration processes. PRP represents a treatment option for many foot and ankle pathologies, including tendinopathy (Achilles, peroneal, posterior tibial, flexor hallucis longus, anterior tibial) and chronic ligamentous injury, such as plantar fasciitis.
The purpose of this study was to assess the safety of PRP injections for treating chronic plantar fasciitis and provide initial clinical assessment of its effectiveness.
Material and methods
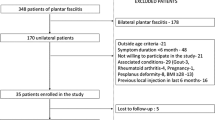
Fourteen consecutive patients (nine women, five men; mean age 49.2 ± 8.8 years) admitted to our hospital between 2008 and 2009 were enrolled in this study. Five patients were athletes at recreational levels and were forced to quit sport participation because of pain at the heel. All patients gave informed consent to participate in the study, which was carried out in accordance with the World Medical Association Declaration of Helsinki. Patients were included if they were ≥18 years, experienced heel pain felt maximally over the plantar aspect for at least six months continuously and had radiographic evidence of calcaneal spur. Patients were treated in the prior three months with conservative therapies, such as icepacks, stretching of the Achilles tendon and NSAID medication, which provided inadequate improvement of pain and functionality. Exclusion criteria included generalised inflammatory arthritis, including ankylosing spondylitis; Reiter syndrome, rheumatoid arthritis or psoriatic arthritis; any wound or skin lesion at the plantar aspect of the foot; pregnancy; severe infection; known malignancy; bleeding disorder; previous surgery, ESWT or corticosteroid injection into the heel, including Achilles tendon; nerve-related symptoms such as radiculopathy, tarsal tunnel syndrome or tarsi sinus syndrome; foot and ankle osteoarthritis.
The Arthrex ACP Double Syringe System™ was used to obtain PRP. This system includes one outer 10-ml syringe. Within this outer syringe, a commercially available 5-ml syringe is connected. Ten millilitres of autologous blood was taken from the antecubital vein with the outer syringe and placed into the Arthrex Centrifuge (Rotofix) and centrifuged for five minutes at 1,500 rpm. During the extracorporeal blood processing, 2 ml of anticoagulant citrate dextrose solution was used to prevent clotting. The system allows supernatant (PRP) transfer from the 10-ml outer syringe into the 5-ml syringe under aseptic conditions. All patients received three injections at the plantar fascia once per week. All injections were performed by one of the authors (SC) on an outpatient basis. The injection point was at the origin of the plantar fascia on the medial tubercle of the calcaneus, as described by Cyriax and Cyriax [5]. The origin of the plantar fascia was approached from the medial side of the foot but near the plantar surface. After injection, all patients were allowed to immediately walk but were advised to avoid weight-bearing sport activities, such as running or jumping, for at least four weeks after the last injection. After PRP injection, patients remained in the outpatient clinic until pain was considered tolerable and were followed in the outpatient clinic at three month intervals or by telephone interview after the last injection to detect possible side effects. NSAIDs were prescribed for no more than three days after injection, and ice packs were allowed for postinjection pain. Physiotherapy treatments were not prescribed during recovery from the injections.
Before treatment and during the follow-up visit, patients were asked to rate their pain on a visual analogue scale (VAS), with zero indicating no pain and ten the worst pain imaginable. Furthermore, modified criteria of the Roles and Maudsley score [14, 24] were used to define the outcome of the procedure: excellent (no pain, patient satisfied with the treatment outcome and unlimited walking without pain), good (symptoms substantially decreased, patient satisfied with the treatment outcome and ability to walk without pain for >one hour), acceptable (symptoms somewhat decreased, pain at a more tolerable level than before treatment and patient slightly satisfied with the treatment outcome) or poor (symptoms identical or worse and patient not satisfied with the treatment outcome). Treatment was considered successful when the patient had an excellent or good score. Patients were examined clinically at 12 months after the index procedure. Data were analyzed using SPSS 13.0 (SPSS Inc., Chicago, IL, USA), with a paired t test after checking normal distribution of samples with the Kolmogorov–Smirnoff z test. The level of significance was considered as p < 0.05.
Results
Mean symptom duration, from the beginning of symptoms to enrolment in the study, was 9.9 ± 2.6 months. No systemic or local complications were noted at any time. Postprocedural pain was reported by almost all patients (78.5 %), with an average VAS score of 8.1, which required icepack treatment and NSAIDs. Posttreatment pain resolved about two hours after infiltration. At the end of the cycle, all 14 patients reported improvement in pain and functionality. Four of five athletic patients were able to resume sport activity at the same level as before the onset of the pain at the heel within three months after the last injection; one was able to resume the same sport at a lower level. According to criteria of the Roles and Maudsley score, at 12 months of follow-up, results were rated as excellent in nine (64.3 %), good in two (14.3 %), acceptable in two (14.3 %) and poor in one (7.1 %) patient. VAS decreased significantly from 7.1 ± 1.1 before treatment to 1.9 ± 1.5 at the last follow-up (p < 0.01).
Discussion
The aim of the study was to evaluate this novel biological approach of treating chronic plantar fasciitis using PRP in order to assess safety and potential outcome measures that can be used in larger, randomised clinical trials to determine its effectiveness treating this pathology. We acknowledge that the limitations of this study, including lack of a randomised control group, small number of patients and short follow-up period, do not allow drawing final conclusions about the role of PRP injection for treating recalcitrant plantar fasciitis, and well-designed prospective randomised studies are warranted.
Although limited by many factors, results of our series showed that three PRP injections provided improvement in VAS for pain, with symptom resolution in 78.6 % of the patients. This confirms reports by other authors that suggest an improved healing process of tendons following local administration of growth factors through PRP injections [1, 3]. Although there are many studies in the literature that examine PRP administration for treating chronic tendinopathy, evidence to date showing the benefit of PRP injections is controversial. De Vos et al. performed a randomised placebo-controlled trial of 54 patients with Achilles tendinopathy treated at a single centre with exercise (usual care) and injection of either PRP or saline solution (placebo group) [7]. The authors concluded that PRP injection did not provide greater pain relief or improvement of nonfunctional activities compared with placebo. In a prospective study of 15 patients with chronic elbow tendinosis, Mishra et al. found significant pain decrease two years after PRP injection [22].
An injection of autologous blood for managing chronic plantar fasciitis has been reported. A prospective randomised study by Lee et al. compared autologous blood injection with corticosteroid injection [17]. Although intralesional autologous blood significantly decreased pain levels and increased tenderness thresholds over the six month follow-up period, corticosteroid was considered superior in terms of speed and, probably, extent of improvement. The authors suggest that administration of intralesional autologous blood injection could be used for patients in whom first-line noninvasive treatment failed to decrease pain levels and when corticosteroid injection fails or is contraindicated. Barrett et al. applied a single injection of PRP in a pilot study of nine patients and reported 78 % symptom resolution at short-term follow-up of two months [2]. However, direct comparison with previous studies is difficult because of the different methodologies used to prepare PRP. Several systems are commercially available that allow efficient preparation for outpatient use. When selecting a preparation system, many factors must be taken into account, such as volume of autologous blood drawn, centrifuge rate/time, leukocyte concentration, delivery method, activating agent, final PRP volume and final platelet and growth-factor concentration. Due to differences in PRP characteristics, reported evidence for clinical effectiveness of PRP cannot be generalised to all of these systems. Furthermore, variation of haematologic parameters (e.g. leukocyte count, platelet count) between patients may also affect the final PRP preparation. Controversies regarding the optimal quantity of platelets and growth factors required for muscle and tendon healing still persist [25]. Although in previous studies clinically effective PRP is defined as having at least four times the normal platelet concentration [20], PRP’s effectiveness is demonstrated with less concentrated preparations [2, 9].
In the study reported here, the Arthrex ACP Double Syringe System™ was used to extract PRP from patients’ peripheral blood, achieving a ≥2× platelet count [26]. Due to low platelet concentration in PRP obtained with this system, three injections were given to maximise PRP’s regenerative effect.
One limitation of this study is the lack of a control group with patients treated with a plantar-fascia-specific stretching protocol. Di Giovanni et al. reported a significant decrease in pain at two years of follow-up and improved functional limitations in 92 % of 66 patients treated with a plantar-fascia-specific stretching exercise [8]. However, because that long-term trial did not compare patients who were stretching to a control group, the authors could not conclude that the changes in symptoms were related to the exercise performed. Consequently, despite the limitations of our study, the protocol presented here could potentially be useful to inspire larger randomised clinical trials to determine whether PRP is effective for treating recalcitrant plantar fasciitis.
References
Andia I, Sanchez M, Maffulli N (2010) Tendon healing and platelet-rich plasma therapies. Expert Opin Biol Ther 10:1415–1426
Barrett S, Erredge S (2004) Growth factors for chronic plantar fasciitis. Podiatr Today 17:37
Bosch G, van Schie HT, de Groot MW et al (2010) Effects of platelet-rich plasma on the quality of repair of mechanically induced core lesions in equine superficial digital flexor tendons: a placebo-controlled experimental study. J Orthop Res 28:211–217
Crawford F, Thomson C (2003) Interventions for treating plantar heel pain. Cochrane Database Syst Rev 3 CD000416
Cyriax JH, Cyriax PJ (1983) Illustrated manual of orthopaedic medicine. Butterworth, London
Davis PF, Severud E, Baxter DE (1994) Painful heel syndrome: results of nonoperative treatment. Foot Ankle Int 15:531–535
de Vos RJ, Weir A, van Schie HT et al (2010) Platelet-rich plasma injection for chronic Achilles tendinopathy: a randomized controlled trial. JAMA 303:144–149
DiGiovanni BF, Nawoczenski DA, Lintal ME et al (2006) Plantar Fascia-Specific Stretching Exercise Improves Outcomes in Patients with Chronic Plantar Fasciitis. A prospective clinical trial with two-year follow-up. J Bone Joint Surg 88A:1775–1881
Eppley BL, Woodell JE, Higgins J (2004) Platelet quantification and growth factor analysis from platelet-rich plasma: Implications for wound healing. Plast Reconstr Surg 114:1502–1508
Filardo G, Kon E, Della Villa S, Vincentelli F, Fornasari PM, Marcacci M (2010) Use of platelet-rich plasma for the treatment of refractory jumper’s knee. Int Orthop 34:909–915
Foster TE, Puskas BL, Mandelbaum BR et al (2009) Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med 37:2259–2272
Gollwitzer H, Diehl P, von Korff A et al (2007) Extracorporeal shock wave therapy for chronic painful heel syndrome: a prospective, double blind, randomized trial assessing the e& cacy of a new electromagnetic shock wave device. J Foot Ankle Surg 46:348–357
Gosens T, Den Oudsten BL, Fievez E, van’t Spijker P, Fievez A (2012) Pain and activity levels before and after platelet-rich plasma injection treatment of patellar tendinopathy: a prospective cohort study and the influence of previous treatments. Int Orthop 36:1941–1946
Haake M, Buch M, Schoellner C et al (2003) Extracorporeal shock wave therapy for plantar fasciitis: randomised controlled multicentre trial. BMJ 327:75
Hall MP, Band PA, Meislin RJ et al (2009) Platelet-rich plasma: current concepts and application in sports medicine. J Am Acad Orthop Surg 17:602–608
Healey K, Chen K (2010) Plantar fasciitis: current diagnostic modalities and treatments. Clin Podiatr Med Surg 27:369–380
Lee TG, Ahmad TS (2007) Intralesional autologous blood injection compared to corticosteroid injection for treatment of chronic plantar fasciitis. A prospective, randomized, controlled trial. Foot Ankle Int 28:984–990
Malay DS, Pressman MM, Assili A et al (2006) Extracorporeal shockwave therapy versus placebo for the treatment of chronic proximal plantar fasciitis: results of a randomized, placebo-controlled, double-blinded, multicenter intervention trial. J Foot Ankle Surg 45:196–210
Martin RL, Irrgang JJ, Conti SF (1998) Outcome study of subjects with insertional plantar fasciitis. Foot Ankle Int 19:803–811
Marx RE (2004) Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg 62:489–496
Mishra A, Pavelko T (2006) Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med 34:1774–1778
Mishra A, Woodall J Jr, Vieira A (2009) Treatment of tendon and muscle using platelet-rich plasma. Clin Sports Med 28:113–125
Ogden JA, Alvarez RG, Marlow M (2002) Shockwave therapy for chronic proximal plantar fasciitis: a meta-analysis. Foot Ankle Int 23:301–308
Roles NC, Maudsley RH (1972) Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J Bone Joint Surg 54B:499–508
Sánchez M, Anitua E, Azofra J, Andía I, Padilla S, Mujika I (2007) Comparison of surgically repaired Achilles tendon tears using platelet-rich fibrin matrices. Am J Sports Med 35:245–251
Speed CA (2004) Extracorporeal shock-wave therapy in the management of chronic soft-tissue conditions. J Bone Joint Surg 86B:165–171
Acknowledgments
Authors thank Mrs. Valentina Albi for her help in preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martinelli, N., Marinozzi, A., Carnì, S. et al. Platelet-rich plasma injections for chronic plantar fasciitis. International Orthopaedics (SICOT) 37, 839–842 (2013). https://doi.org/10.1007/s00264-012-1741-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1741-0