Abstract
Purpose
Tuberculosis of the osteoarticular system usually manifests as joint arthritis. There is no available English literature on the tubercular involvement of the enthesis (tendon-bone junction).
Methods
We performed a retrospective analysis on 14 patients with tuberculosis of the tendon-bone junction. Patients presenting with a sinus with or without presence of radiological evidence of bone destruction around the enthesis, and pain unresponsive to a trial of analgesics and physical therapy, were evaluated by closed or open biopsy for tuberculosis. A staging system is proposed for biopsy-proven tuberculosis of the enthesis.
Results
Between 2006 and 2010, we treated 14 patients with tuberculosis of the tendon-bone junction. Biopsy-proven cases of tuberculosis of the enthesis were administered anti-tubercular drugs for a period of one year. Sequestrectomy was performed in advanced lesions. The tendon-bone junction was rested until the features of its healing were clinically evident. The patients aged between 18 and 52 years were followed up for an average of 1.7 years after cessation of anti-tubercular drug therapy. They responded favourably, and none had recurrence of the disease.
Conclusions
This study describes the tubercular involvement of the entheses, which heretofore has not been described in the literature. The rarity of its occurrence and lack of suspicion of an infectious aetiology in these locations frequently results in late diagnosis and incorrect initial treatment. This study also supports the “microtrauma theory” in the genesis of osteoarticular tuberculosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traction epiphyses (apophyses) develop due to the contraction forces of strong muscle-tendon units [1]. These tendon-bone junctions of apophyses are subjected to strain in everyday life. Although attrition, degenerative and inflammatory lesions have been common, tuberculosis involving the entheses has not been reported. This study describes the clinical progression and radiological picture of tuberculosis at the tendon-bone junction. All of the patients were treated initially for muscle sprains or sports injuries, and the diagnosis was missed on an average for four months. Tuberculosis can mimic many clinical and radiological diagnoses. The infection begins as enthesitis and progresses to entheso-osteomyelitis with sequestrum formation. The diagnosis may be made early if suspicion of an infectious aetiology is considered, after the failure of conventional treatment with anti-inflammatory medications and physical therapy.
Patients and methods
Pain at the tendon-bone interface is commonly related to sports or overuse. Between 2006 and 2010, 97 patients were referred to our unit for symptoms localised to the tendon-bone interface, unresponsive to conventional treatment of analgesics and physical therapy. Further examination and investigations diagnosed seropositive rheumatoid arthritis in 13 patients, 32 patients had pain associated with hyperuricaemia (serum uric acid levels more than 7 mg/dl), ankylosing spondylitis was diagnosed in four patients, seven patients were diagnosed with calcific tendinitis and four patients with Osgood-Schlatter disease. Lack of diagnosis and persistence of symptoms in 37 patients were the criteria for further evaluation, including tissue biopsy. Biopsy results revealed chronic inflammation in 20 cases, low-grade pyogenic infection in three patients and tubercular infection in 14. These 14 patients with the diagnosis of tuberculosis of the entheses form the basis of this article.
Prior to the tissue diagnosis, all of the patients were initially treated on the suspicion of overuse or sports-related injuries (Table 1). When the discomfort persisted despite analgesics and physical therapy, haematological investigations and radiographs of the involved area were ordered. For a tuberculosis screening, a chest radiograph, sputum for acid-fast bacilli (AFB) and tuberculin test were done in addition. In the presence of increasing disability and pain, an open or closed (core) biopsy from the area of involved bone was done to establish the diagnosis of tuberculosis. Computed tomography (CT) scans were advised to all patients with suspicion of a sequestrum on plain radiographs. These were done by three patients. Magnetic resonance imaging (MRI) was not done in any case.
The prolonged duration of the disease, persistence of signs and symptoms, failure to respond to previous treatment modalities and the radiographic evidence of an erosive lesion in the symptomatic bone led to a decision to perform a tissue biopsy. Core biopsy was done in suspected lesions without the evidence of a sinus or excessive bone destruction. Open biopsy with debridement was performed in lesions with a sinus and a sequestrum as a part of the diagnostic and disease-debulking procedure.
The patients who were eventually diagnosed as having tuberculosis of the entheses could retrospectively be divided into three stages. Stage 1 patients presented clinically with pain, increasing on use of the involved muscle-tendon unit with or without swelling. Radiographs showed no evidence of bone involvement. Stage 2 patients presented with persistent pain, unrelated to activity. Movement of the involved tendon was avoided by the patient, and joint movements were restricted in juxta-articular lesions. Swelling was present with or without a draining sinus. Radiographs showed erosion or lucent lesion at the site of the tendon attachment to bone (Fig. 1). Stage 3 patients presented with the clinical features of stage 2 lesions, a progressively increasing swelling and usually a draining sinus. Radiographs showed an erosive lesion in the bone, with a sequestrum (Fig. 2).
The biopsy specimen was submitted for histopathological diagnosis. Presence of chronic inflammation, tubercles with Langhans giant cells and granulomatous inflammation with evidence of central caseation were considered to be consistent with the diagnosis of tuberculosis.
Results
The average age of the patients in this study was 32 years (18–52 years). There were seven male and seven female patients. There was an average delay of four months (two to eight months) before tuberculosis was diagnosed and treatment was started. Haematological investigations were inconsistent with the diagnosis of tuberculosis. Erythrocyte sedimentation rate (ESR) was elevated (more than 20 mm/h) in eight of 14 patients (57.1 %). Total leukocyte count was elevated (more than 11,000/mm3) in nine of 14 patients (64.3 %). Chest radiographs were suspicious for tuberculosis in four of 14 patients (28.6 %). Sputum AFB was positive only in two of 14 cases (14.3 %). Tuberculin test was positive (more than 15 mm) in ten of 14 patients (71.4 %). No patient tested positive for a concomitant human immunodeficiency virus (HIV) infection.
Seven patients (50 %) had extensive bone involvement at presentation and required sequestrectomy and debridement for control of infection and to establish a diagnosis. We were initially unaware of the occurrence of tuberculosis in the entheses. As our experience increased with the diagnosis of tuberculosis in these locations, we maintained a low threshold for early biopsy from the suspicious lesions.
The patients presenting with a draining sinus underwent excision of the sinus tract, drainage of the abscess and curettage of the involved bone. Stage 3 lesions were managed by removal of the sequestrum in addition to the above procedures (Fig. 3a, b). In both situations the tendon attachment site to the bone was carefully examined. It was found to be discoloured (ivory-yellow) and frayed at the site of attachment to bone. The diseased area was carefully debrided and the tendon was preserved in continuity with the bone. Streptomycin powder was instilled in the bony cavity post-curettage. Lesions around the knee, foot and ankle were rested in a plaster-of-Paris splint for six weeks. The upper limb lesions were rested for six weeks in a sling support.
Tissue diagnosis of tuberculous infection combined with the indicative blood parameters and tuberculin test reports were used to start the treatment. Anti-tubercular chemotherapy consisted of an intensive phase of four drugs. Isoniazid (5–10 mg/kg), rifampicin (10 mg/kg), pyrazinamide (20–40 mg/kg) and ethambutol (15–25 mg/kg) for a period of two months, followed by a continuation phase with two drugs (isoniazid and rifampicin) for the next ten months. Improvement of clinical symptoms and blood parameters (total leukocyte count and ESR) at two months were selected as an arbitrary time for conversion from a four-drug regimen to the continuation phase.
The patients were evaluated clinically every two weeks in the intensive phase of anti-tubercular drugs and every two months in the continuation phase to observe for pain, swelling, disability and drug-related side effects until discontinuation of medications at one year. Subsequently, follow-up visits were advised every three months to observe for recurrence of the lesion or appearance of disability at the tendon-bone junction. Gradual mobilisation of the involved tendon and joint was started at six weeks. Graduated loading of the extremity was permitted at three months as per pain tolerance of the patient. Vigorous physiotherapy was avoided to prevent avulsion of the tendon from the diseased tendon-bone junction.
The condition of the patients progressively improved after starting anti-tubercular drugs. None of the patients developed resistance to the medications, and no side effects were reported. In the first two months, pain and swelling subsided and the sinuses healed. Joint stiffness was the most common complaint in the healing period. The range of movement of the joints continued to improve for up to six months and was pain free. The radiographs also showed evidence of healing of the disease. This manifested as appearance of bony trabeculae in the curetted lesions and by appearance of sclerosis in the erosive lesions (Fig. 4a, b). The anti-tubercular therapy was discontinued at 12 months. No tendon avulsions occurred. The juxta-articular lesions which were diagnosed as stage 3 at presentation had some residual restriction of joint motion, which persisted even at the last follow-up. This caused no functional impairment to the patient.
Discussion
Tuberculosis of the bone and joints is not common in the developed countries, and it accounts for only 1–3 % of all cases of tuberculosis reported worldwide [2, 3]. This may be the reason why in the initial stages the diagnosis of a lesion is not considered to be tubercular. Recently, tuberculosis with its diverse clinical and radiological manifestations is reappearing in Western countries. This is due to the emergence of resistant strains, emigration of workers from endemic areas and association of tuberculosis with patients on immunosuppressant medications and HIV infection [2, 3].
The tendon-bone junction (enthesis) has unique properties of stress dissipation as it is a transition zone between a dense osseous tissue and a more pliable tendinous tissue [4, 5]. The tendon-bone junction is a location for constant traction forces and microavulsions occur alongside stress shielding at this interface. The location has a slow healing response, takes longer to remodel and even longer for its mechanical properties to be restored [5]. Traction epiphyses or apophyses have been described as metaphyseal-equivalent locations. There is developmental similarity in vascular supply to the metaphyses of long bones and the apophyses, and pyogenic infections have been described in these locations [6]. This “repeated microtrauma” environment may cause the bacteria to proliferate at the site of inflammation and repair, in the presence of bacteraemia [6].
Isolated incidence of tuberculosis in the flat bones or in the tendons has been sporadically reported in the literature [7–10]. It has not been described at the tendon-bone interface. It is not clear whether the tubercular infection of the enthesis starts on the tendon side or in the bone. Taking analogy from the disc and vertebral body tuberculosis, it is probably the bone which develops the first lesion due to its better vascularity, and spread to the tendon is secondary [6]. The disease proliferation eventually affects both sides of the junction.
The tubercular lesion of enthesis probably begins as an enthesitis (stage 1), progressing to entheso-osteitis (stage 2) and entheso-osteomyelitis (stage 3). Many reported cases in the literature were diagnosed at the osteomyelitis stage; 50 % of our cases were also diagnosed when chronic osteomyelitic changes had taken place around the enthesis. It is very difficult to diagnose lesions in the stage of enthesitis unless the suspicion is in favour of an infectious aetiology.
Diagnosing tuberculosis in these locations is a big challenge for the clinician. Most of the time, the common diagnoses in these locations may lead to a delayed correct assessment and hence may contribute towards the progression of the disease (Table 2). We found this to be true in all of our cases, which were later diagnosed as tuberculosis. Early presentation is with pain and sometimes with localised swelling. These early lesions are most often misdiagnosed, as the duration of symptoms is less, blood reports are inconclusive and radiographic evidence is not pronounced [11]. Late presentation is with a progressively enlarging swelling, discharging sinus, bony erosion and sequestrum formation.
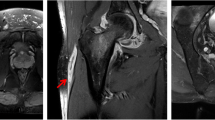
The lesion at the tendon-bone interface is not apparent on radiographs until osteitis or osteomyelitis has developed. MRI may be helpful in the early diagnosis of a suspicious lesion. Inflammatory enthesopathies and apophysitis are difficult to distinguish from infectious lesions in these locations even on an MRI scan [12]. A CT scan clearly defines the presence of a sequestrum in the osteomyelitic cavity. It may be helpful in staging the disease and in planning the surgical approach to sequestrectomy around a diseased tendon attachment (Fig. 5b).
a Plain anteroposterior radiographs of the proximal tibia showing presence of lucencies in the proximal tibia. A metaphyseal sequestrum can be poorly delineated. b CT scan of the proximal left tibia shows a well-defined sequestrum in the metaphyseal region, underlying the attachment of the patellar tendon. The sequestrum has a thin cortical shell over its lateral aspect. The lateral paratendinous approach was used for sequestrectomy
Tissue obtained by core or open biopsy which demonstrates evidence of tubercular infection is essential in establishing the diagnosis in these rare locations for this disease. The osteoarticular lesions respond to medical management and a 90 % cure rate has been reported with anti-tubercular chemotherapy [13]. Surgical intervention may be reserved for non-healing lesions with the presence of a sequestrum and in patients with a doubtful diagnosis.
The tendon-bone junction is a specialised architectural advancement in biological anchorage. Studies in the literature on Achilles tendon, partial patellectomy and extensor reconstruction, and anterior cruciate ligament repair have repeatedly mentioned the difficulty and unpredictability in obtaining the histological similarity and biomechanical properties of surgical reconstructions to the natural tendon-bone interface [5]. Increased vascularity of underlying bone following anti-tubercular chemotherapy, prolonged disease duration and tendon damage may predispose the junction to avulsion with early vigorous attempts at rehabilitation. Tendon avulsion from an infected bone may bring about a very difficult scenario which necessitates infection control, tendon reattachment, delayed rehabilitation and combating residual disability. Hence, we believe that a “healing” enthesis needs to be rested for the initial phase of anti-tubercular chemotherapy to avoid complications.
The limitations of this retrospective study happen to be a limited number of patients with this disease, and therefore a lack of uniformity in diagnostic evaluations. A tubercular sequestrum may not always be clearly definable on a plain radiograph (Fig. 5a, b). A CT scan of the lesion could not be done in all patients. We feel that the presence of a CT-defined sequestrum could have categorised certain stage 2 lesions as stage 3. In this study, the entheses were rested during the healing period to prevent tendon avulsion, and this may have been a contributory factor for some residual disability in periarticular lesions. A control group is needed to further investigate the strength of the healing enthesis. This is to establish whether the tendon-bone junction requires movement or rest during the initial period of chemotherapy and to note the incidence of tendon avulsions and joint disability in either group.
References
Salter RB, Harris WR (1963) Injuries involving the epiphyseal plate. J Bone Joint Surg Am 45A(3):587–622
García S, Combalía A, Serra A, Segur J-M, Ramón R (1997) Unusual locations of osteoarticular tuberculosis. Arch Orthop Trauma Surg 116:321–323
Tuli SM (2002) General principles of osteoarticular tuberculosis. Clin Orthop Relat Res 398:11–19
Lui PPY, Zhang P, Chan KM, Qin L (2010) Biology and augmentation of tendon-bone insertion repair. J Orthop Surg Res 5:59
Benjamin M, Toumi H, Ralphs JR, Bydder G, Best TM, Milz S (2006) Where tendons and ligaments meet bone: attachment sites (‘entheses’) in relation to exercise and/or mechanical load. J Anat 208:471–490
Nixon GW (1978) Hematogenous osteomyelitis of metaphyseal-equivalent locations. AJR Am J Roentgenol 130:123–129
Chaudhary IA, Samiullah MAA (2005) An unusual presentation of tuberculosis of Iliac bone. Pak J Med Sci Q 21(4):489–490
Krishnan H, Yoon TR, Park KS, Cho YJ (2010) Ischial tuberosity tuberculosis: an unusual location and presented as chronic gluteal abscess. Malays Orthop J 4(1):42–45
Oğut T, Gökçe A, Kesmezacar H, Durak H, Botanlioğlu H, Erginer R (2007) Isolated tuberculous tenosynovitis of the Achilles tendon: a report of two cases. Acta Orthop Traumatol Turc 41(4):314–320
Franceschi F, Longo UG, Ruzzini L, Denaro V (2007) Isolated tuberculosis of the patellar tendon. J Bone Joint Surg Br 89(11):1525–1526
Longo UG, Marinozzi A, Cazzato L, Rabitti C, Maffulli N, Denaro V (2011) Tuberculosis of the shoulder. J Shoulder Elbow Surg 20(4):e19–e21
Arnaiz J, Piedra T, de Lucas EM, Arnaiz AM, Pelaz M, Gomez-Dermit V, Canga A (2011) Imaging findings of lower limb apophysitis. AJR Am J Roentgenol 196:W316–W325
Shembekar A, Babhulkar S (2002) Chemotherapy for osteoarticular tuberculosis. Clin Orthop Relat Res 398:20–26
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Narang, S. Tuberculosis of the entheses. International Orthopaedics (SICOT) 36, 2373–2378 (2012). https://doi.org/10.1007/s00264-012-1657-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1657-8