Abstract
Purpose
Postoperative maintenance of high haemoglobin (Hb) levels and avoidance of homologous blood transfusions is important in total hip arthroplasty (THA). The introduction of a postoperative drainage autologous blood transfusion (ABT) system or no drainage following THA has resulted in reduction of homologous blood transfusion requirements compared with closed-suction drains. The purpose of this study was to examine which regimen is superior following THA.
Methods
A randomised controlled blinded prospective single-centre study was conducted in which 100 THA patients were randomly allocated to ABT or no drainage. The primary endpoint was the Hb level on the first postoperative day.
Results
The postoperative collected drained blood loss was 274 (±154) ml in the ABT group, of which 129 (±119) ml was retransfused (0–400). There was no statistical difference in Hb levels on the first postoperative day (ABT vs no drainage: Hb 11.0 vs 10.9 g/dl), on consecutive days (day 3: Hb 10.7 vs 10.2, p = 0.08) or in total blood loss (1,506 vs 1,633 ml), homologous transfusions, pain scores, Harris Hip Score, SF-36 scores, length of hospital stay or adverse events.
Conclusions
The use of a postoperative autologous blood retransfusion drain did not result in significantly higher postoperative Hb levels or in less total blood loss or fewer homologous blood transfusions compared with no drain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty (THA) is associated with a large amount of blood loss, intraoperatively and postoperatively, including “hidden” blood loss, totalling 1,500 ml and a mean postoperative decline in haemoglobin (Hb) levels of 3.0 g/dl [1]. Higher pre- and postoperative Hb levels are correlated with better early functional recovery, higher SF-36 score, higher patient satisfaction and shorter hospital stay following THA [2, 3], although not substantiated in every study [4], and with a reduced homologous blood transfusion rate [2–5]. THA are frequently complicated by the need for homologous blood transfusions, with their concomitant disadvantages [6–9]. The introduction of postoperative autologous blood transfusion (ABT) systems has resulted in a reduction of perioperative net blood loss and homologous blood transfusion rates, compared with closed-suction drains [10–14]. The use of drains of any kind might however be questioned, as no drainage following total hip implantation has also been shown to result in reduced homologous transfusion rates when compared to regular closed-suction drains [15]. It was therefore stated in a Cochrane review on this subject that further studies were needed comparing autotransfusion with no drainage, examining Hb levels, blood loss and homologous blood transfusion requirement [15]. This has never been tested in THA in a blinded randomised controlled trial. The purpose of this study was to conduct a blinded prospective randomised controlled trial evaluating the effects of a postoperative low-vacuum ABT system compared with no drainage following THA. The primary endpoint of our study was the Hb level on the first postoperative day.
Materials and methods
The study is an open double-blind randomised controlled prospective single-centre study with two parallel groups. Approval of our Institutional Medical Ethics Committee was obtained for this study, in which 100 patients scheduled for primary total hip surgery were randomised to either the postoperative autologous transfusion group (Bellovac ABT, autologous blood salvage, low vacuum, 60–90 mm Hg, Astra Tech, Mölndal, Sweden) or the no drainage group. Patients were enrolled based on the following inclusion criteria: provision of written informed consent, subjected to primary total hip surgery and if not meeting any of the exclusion criteria: coagulation disorders including deep venous thrombosis and pulmonary embolism, malignancy, ongoing infections, untreated hypertension, unstable angina pectoris, myocardial infarction within the past 12 months, coronary bypass operation within the past 12 months, intake of anticoagulants or participation in other clinical trials dealing with any drugs that affect blood loss.
Formal randomisation and concealed allocation took place prior to the operation. Numbered sealed opaque envelopes containing pre-randomised cards with either “autologous transfusion group” or “no drainage group” were available in the operating room. The surgeons were blinded for group allocation until the end of surgery, just before closure of the wound, at which time the envelope was opened and the patient’s group allocation was disclosed to the surgeon.
All patients were operated upon at Isala Clinics, Zwolle, The Netherlands. Cemented hip prostheses (SP-2 stem, Fal cup, Link, Hamburg, Germany), uncemented prostheses (Bi-Metric stem, Recap cup, Biomet, Warsaw, IN, USA) and reversed hybrid prostheses (cemented cup, uncemented stem) of these components were included in the study. Cefazolin was used as routine prophylactic antibiotic treatment. Surgeons used either the posterolateral or anterolateral approach according to their preference. A drain was inserted in the autotransfusion group. Low suction was started and the drained blood was retransfused within 6 h of surgery. Retransfusion of more than 1,500 ml was not allowed. Drains were removed 24 h postoperatively.
Patients attended the outpatient clinic preoperatively and were reviewed during hospital stay and at 6 weeks and 3 months postoperatively. The primary endpoint of this study was the Hb level on the first postoperative day. Secondary endpoints included Hb levels on the second and third postoperative days, the lowest postoperative Hb level, blood loss during surgery, homologous blood transfusions, incidence of haematomas, amount of drained retransfused wound blood, wound healing disturbances, postoperative pain, length of hospital stay, adverse events, Harris Hip Scores (HHS) [16], physical and mental SF-36 [17] scores, and total blood loss. Total blood loss was calculated according to Gross [18], based on the maximum perioperative decrease in Hb level and the patients’ preoperative blood volume: blood loss = preoperative blood volume × (Hb preoperative − Hb lowest)/Hb average. Preoperative blood volume was calculated as 65 ml/kg. Hb average is the average of preoperative Hb level and lowest postoperative Hb level.
Operation time, type of anaesthesia and patients’ body temperature at the end of surgery were also recorded because of their effect on blood loss. Haematomas were recorded. Wound healing disturbances were recorded when redness of the skin was observed at more than 1 cm from the incision wound. Other potential wound healing problems such as discharge from the wound were recorded. Wound discharge was scored when any discharge of wound fluid was seen. Deep infection, suspected on clinical grounds, was diagnosed based on a positive culture at reoperation. Pain at rest and during exercise was scored on a visual analogue scale (VAS). Adverse events were registered during hospital stay and at the first 3 months postoperative visit. The doctors who performed the postoperative examinations in the outpatient clinic were blinded for group allocation. A standardised blood management protocol was implemented for this study:
-
Venous thromboembolism prophylaxis was carried out using fondaparinux (Arixtra®, 2.5 mg/0.5 ml) subcutaneously once daily. The first dose was administered on the evening of the day of surgery and prophylaxis was continued for 5 weeks.
-
Administration of non-selective non-steroidal anti-inflammatory drugs (NSAIDs) was stopped 1 day before surgery. The COX-2 selective NSAID meloxicam 15 mg once daily was used in all patients.
-
Administration of acenocoumarol was stopped 3 days before surgery and acetylsalicylates 7 days before surgery.
-
Additional homologous blood transfusions were given based on the Dutch homologous blood transfusion guidelines [19]. The trigger for homologous transfusions was an Hb level of 6.4 g/dl in American Society of Anesthesiologists (ASA) 1 patients, 8.0 g/dl in ASA 2/3 patients and 9.6 g/dl in ASA 4 patients and in patients that failed to increase their cardiac output to compensate for dilution [19].
Statistical analysis
Based on a clinically relevant difference in Hb levels on the first postoperative day of 0.8 g/dl (10.2 vs 11.0 g/dl, SD 1.4 [13]), alpha of 0.05 and a power of 80.8 %, a sample size of 50 patients per group was calculated for this study. Study data were collected using customised case report forms and entered into a computerised database that allowed unbiased and reliable data management. Statistical analysis was conducted with SPSS v. 17.0 (SPSS Inc., Chicago, IL, USA) statistical software. Categorical data were expressed as percentages. Continuous data were expressed as means and SD. Differences were analysed using chi-square tests for categorical data and Student’s t tests for continuous data. The Levene test was used to check for test assumptions. A two-sided p < 0.05 was considered to be statistically significant. All 50 patients in the autotransfusion group were subjected to the efficacy analysis, regardless of whether an autotransfusion was actually performed, because of the intention-to-treat principle.
Results
Patients were enrolled between February 2007 and April 2008. In total, 100 patients were included, equally divided over the postoperative autotransfusion group and the no drainage group. The groups were statistically homogeneous with respect to gender, age, body mass index (BMI), medical history, Charnley osteoarthritis classification and indication for operative treatment (Table 1). There were no significant differences between the two groups regarding anaesthetic and surgical parameters that could affect blood loss, such as type of anaesthesia, body temperature, surgeon, surgical approach or fixation of the prosthesis, except for operation time, which was 9 min longer in the autotransfusion group, p = 0.004 (Table 1).
Perioperative blood loss, autologous transfusion and Hb levels
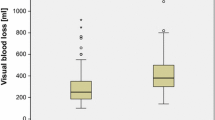
The intraoperative blood loss, 529 (± 280) and 469 (± 163) ml, was not significantly different between the two groups. The collected drain fluid in the first 24 h amounted to 274 (± 154) ml in the low-vacuum drainage autotransfusion group. In the first 6 h postoperatively, 172 (±98) ml was collected from which, on average, 129 (±119) ml was retransfused (0–400). In 17 of the 50 patients (34 %) in the autotransfusion group, in whom a low-vacuum retransfusion drain was inserted, the collected drain fluid was not retransfused due to small volumes of drained wound blood, substantial blood clot formation in the drained blood, technical failures or fever. The average retransfusion volume in 33 of the 50 patients on whom retransfusion was performed was 199 (± 88) ml.
There was no difference in the primary endpoint of the study, Hb levels on the first postoperative day, 11.0 and 10.9 g/dl, respectively, p = 0.72. During hospital stay, Hb levels in the ABT group were not significantly higher than in the no drainage group, 10.7 vs 10.2 g/dl, p = 0.08 at the third postoperative day. There was no significant difference in lowest postoperative Hb levels. Homologous blood transfusions were needed equally in both groups, in two patients in the retransfusion group and in four patients in the no drainage group, p = 0.41. Two units of homologous blood were given to those patients. Preoperative blood volume was 5,161 (±866) ml in the ABT group and 5,139 (±943) ml in the no drainage group, NS. Calculated net total blood loss was not significantly different, 1,506 (±564) ml in the ABT group and 1,633 (±645) in the no drainage group, p = 0.30.
Pain, HHS and SF-36 scores
Pain scores were similar between the groups preoperatively, during hospital stay, and 6 weeks and 3 months postoperatively, except for exercise pain scores at 6 weeks which were higher in the autotransfusion group (Table 2). The HHS was similar before surgery and 6 weeks and 3 months after surgery in the autotransfusion and no drainage groups. There was no statistical difference in the physical, mental and total SF-36 scores preoperatively and 6 weeks postoperatively between the two groups.
Wound healing
Wound healing disturbances occurred equally often in both groups during hospital stay (Table 3). There was no statistical difference in the number of haematomas. Wound leakage was seen more often in the group without drainage system than in the ABT group on the third postoperative day, 62 vs 32 %, p = 0.003, and at discharge (day), 48 vs 20 %, p = 0.003.
Adverse events
Adverse events on recovery, on the ward during the rest of hospital stay and afterwards until 3 months postoperatively were equally frequent in both groups (Table 3). One intraoperative complication was seen: a fissure of the femoral shaft in the autotransfusion group. There were four deep infections of the hip prostheses, two in each group, all revised within 5 weeks (range 2–5 weeks) of the index operation. All patients had positive cultures on lavage and were treated with antibiotics postoperatively. At follow-up, no signs of infection were observed at about 10 months (range 5–19 months). In the no drainage group, three patients reported persistent wound discharge 2 weeks after surgery, one requiring readmission. Symptoms of venous thrombosis or pulmonary embolism were not diagnosed during hospital stay or 3 months postoperatively.
Hospital stay
Length of hospital stay was not significantly different, 4.3 ± 0.7 days in the retransfusion group and 4.6 ± 1.3 days in the no drainage group, p = 0.16. Most patients were discharged on the predetermined discharge date.
Discussion
To the best of our knowledge, no blinded randomised controlled trial has been published comparing a postoperative drainage ABT system with no drainage following THA. In this study, the use of a postoperative drainage autotransfusion system (ABT) did not result in a difference in Hb levels on the first postoperative day, the primary endpoint of the study, compared to no drainage following primary THA.
The postoperative maintenance of high Hb levels and the avoidance of homologous blood transfusions is important after surgery and are associated with a better early functional postoperative recovery following THA [2, 3].
A recent Cochrane review reported that the use of perioperative autotransfusion reduced the rate of exposure to homologous blood transfusions by 54 % in orthopaedic surgery, compared with closed-suction drainage [10]. One of the advantages of autologous retransfusion is the good quality and the direct contribution of the retransfused red blood cells to oxygen transport, delivery and consumption in the patient [20–24]. This is in contrast to red blood cells in homologous transfusions from a blood bank, in which optimal contribution to the oxygen consumption may take several hours because of so-called storage lesions [25, 26].
In THA, the use of a postoperative ABT system reduced homologous blood transfusions from 47 to 34 % and from 21 to 11 % when compared with a closed-suction drainage system [13, 14].
However, another Cochrane review showed that the use of no drainage in THA, compared with closed-suction drainage, decreased the number of patients who required transfusion following THA significantly from 40 to 31 % [15]. The authors stated there is now a need for studies comparing retransfusion with no drain.
Our study compared these two regimens that were superior to closed-suction drainage following THA, i.e. no drainage and the use of a postoperative ABT system. Our study showed no significant differences in postoperative Hb levels on the first, second or third days, or in total blood loss or homologous transfusions. Length of hospital stay was similar, although this is probably influenced by the fact that most patients were discharged on a predetermined date. One study found a positive correlation between Hb levels on discharge and change in SF-36 score from preoperatively to 2 months postoperatively in patients after primary hip arthroplasty [3]. In our study, with no difference in postoperative Hb levels detected, there was no difference in the HHS and SF-36 scores 6 weeks and 3 months postoperatively between the autotransfusion group and the no drainage group.
In surgery, drains are commonly used in order to reduce haematomas and wound leakage. Our study found no significant difference in haematomas. A meta-analysis on closed-suction drainage against no drainage in total hip and knee replacement reported that reinforcement of wound dressings was required significantly 60 % more often in the group managed without drains [15]. In our study there was a significant 50 % reduction of wound leakage on day 3 (32 vs 62 % of patients) and at discharge at approximately day 4 (20 vs 48 %) in the ABT drainage group compared with the no drainage group. Scoring wound discharge is clearly subjective though. Three patients in the no drainage group suffered from profound persistent wound leakage 2 weeks after surgery, one requiring rehospitalisation. Profound postoperative wound discharge might be an argument in favour of the use of drains following THA.
The strength of our study is its blinded prospective randomised setup. The surgeons were blinded to group allocation until the end of surgery, as were the researchers during follow-up. Other factors that could affect perioperative blood loss were examined and proven to be similar for both groups. The weakness of the study is the relatively limited number of patients who were retransfused. Because retransfusion was not performed in 34 % (17) of patients for various reasons, only 33 of 50 patients benefited from autotransfusion. In our opinion this reflects daily practice.
In conclusion, in this prospective randomised blinded study on 100 patients for primary hip arthroplasty the use of a postoperative autologous blood retransfusion drain did not result in significant differences in postoperative Hb levels, total blood loss or homologous blood transfusions compared with no drain.
References
Sehat KR, Evans RL, Newman JH (2004) Hidden blood loss following hip and knee arthroplasty. Correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br 86:561–565
Husted H, Holm G, Jacobsen S (2008) Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 79:168–173
Conlon NP, Bale EP, Herbison GP, McCarroll M (2008) Postoperative anemia and quality of life after primary hip arthroplasty in patients over 65 years old. Anesth Analg 106:1056–1061
Vuille-Lessard E, Boudreault D, Girard F, Ruel M, Chagnon M, Hardy JF (2012) Postoperative anemia does not impede functional outcome and quality of life early after hip and knee arthroplasties. Transfusion 52:261–270
Saleh E, McClelland DB, Hay A, Semple D, Walsh TS (2007) Prevalence of anaemia before major joint arthroplasty and the potential impact of preoperative investigation and correction on perioperative blood transfusions. Br J Anaesth 99:801–808
Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB (1999) An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am 81:2–10
Blumberg N (1997) Allogeneic transfusion and infection: economic and clinical implications. Semin Hematol 34:34–40
Innerhofer P, Klingler A, Klimmer C, Fries D, Nussbaumer W (2005) Risk for postoperative infection after transfusion of white blood cell-filtered allogeneic or autologous blood components in orthopedic patients undergoing primary arthroplasty. Transfusion 45:103–110
Murphy P, Heal JM, Blumberg N (1991) Infection or suspected infection after hip replacement surgery with autologous or homologous blood transfusions. Transfusion 31:212–217
Carless PA, Henry DA, Moxey AJ, O’Connell D, Brown T, Fergusson DA (2010) Cell salvage for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev 3:CD001888
Zacharopoulos A, Apostolopoulos A, Kyriakidis A (2007) The effectiveness of reinfusion after total knee replacement. A prospective randomised controlled study. Int Orthop 31:303–308
Sinha A, Sinha M, Burgert S (2001) Reinfusion of drained blood as an alternative to homologous blood transfusion after total knee replacement. Int Orthop 25:257–259
Strümper D, Weber EW, Gielen-Wijffels S, Van Drumpf R, Bulstra S, Slappendel R, Durieux ME, Marcus MA (2004) Clinical efficacy of postoperative autologous transfusion of filtered shed blood in hip and knee arthroplasty. Transfusion 44:1567–1571
Moonen AF, Knoors NT, van Os JJ, Verburg AD, Pilot P (2007) Retransfusion of filtered shed blood in primary total hip and knee arthroplasty: a prospective randomized clinical trial. Transfusion 47:379–384
Parker MJ, Livingstone V, Clifton R, McKee A (2007) Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev 3:CD001825
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755
Ware JE Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A (1995) Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care 33:AS264–AS279
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anesthesiology 58:277–280
The Dutch Institute for Healthcare Improvement (CBO) Allogenic Blood Transfusion Guideline, p 109. http://www.cbo.nl/Downloads/96/bloedrl2004.pdf
Colwell CW Jr, Beutler E, West C, Hardwick ME, Morris BA (2002) Erythrocyte viability in blood salvaged during total joint arthroplasty with cement. J Bone Joint Surg Am 84-A:23–25
Stachura A, Król R, Poplawski T, Michalik D, Pomianowski S, Jacobsson M, Aberg M, Bengtsson A (2011) Transfusion of intra-operative autologous whole blood: influence on complement activation and interleukin formation. Vox Sang 100:239–246
Elawad AA, Ohlin AK, Berntorp E, Nilsson IM, Fredin H (1991) Intraoperative autotransfusion in primary hip arthroplasty. A randomized comparison with homologous blood. Acta Orthop Scand 62:557–562
Gharehbaghian A, Haque KM, Truman C, Evans R, Morse R, Newman J, Bannister G, Rogers C, Bradley BA (2004) Effect of autologous salvaged blood on postoperative natural killer cell precursor frequency. Lancet 363:1025–1030
Sinardi D, Marino A, Chillemi S, Irrera M, Labruto G, Mondello E (2005) Composition of the blood sampled from surgical drainage after joint arthroplasty: quality of return. Transfusion 45:202–207
Sparrow RL (2010) Red blood cell storage and transfusion-related immunomodulation. Blood Transfus 8(Suppl 3):s26–s30
Johnson BA, Weil MH (1991) Redefining ischemia due to circulatory failure as dual defects of oxygen deficits and of carbon dioxide excesses. Crit Care Med 19:1432–1438
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Horstmann, W.G., Kuipers, B.M., Slappendel, R. et al. Postoperative autologous blood transfusion drain or no drain in primary total hip arthroplasty? A randomised controlled trial. International Orthopaedics (SICOT) 36, 2033–2039 (2012). https://doi.org/10.1007/s00264-012-1613-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1613-7