Abstract
Purpose
Smartphones have gained widespread use in the healthcare field to fulfill a variety of tasks. We developed a small iPhone application to take advantage of the built-in position sensor to measure angles in a variety of spinal deformities. We present a reliability study of this tool in measuring kyphotic angles.
Methods
Radiographs taken from 20 different patients' charts were presented to a panel of six operators at two different times. Radiographs were measured with the protractor and the iPhone application and statistical analysis was applied to measure intraclass correlation coefficients between both measurement methods, and to measure intra- and interobserver reliability
Results
The intraclass correlation coefficient calculated between methods (i.e. CobbMeter application on the iPhone versus standard method with the protractor) was 0.963 for all measures, indicating excellent correlation was obtained between the CobbMeter application and the standard method. The interobserver correlation coefficient was 0.965. The intraobserver ICC was 0.977, indicating excellent reproductibility of measurements at different times for all operators. The interobserver ICC between fellowship trained senior surgeons and general orthopaedic residents was 0.989. Consistently, the ICC for intraobserver and interobserver correlations was higher with the CobbMeter application than with the regular protractor method. This difference was not statistically significant.
Conclusion
Measuring kyphotic angles with the iPhone application appears to be a valid procedure and is in no way inferior to the standard way of measuring the Cobb angle in kyphotic deformities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the first description by John Cobb in 1948 [1], the Cobb angle [2] has been the gold standard for evaluating frontal and sagittal spinal deformities. Even though it has become a daily routine for spine surgeons, the Cobb angle measurement process is still the same as the one developed more than 60 years ago, namely, drawing lines on vertical radiographs and measuring the resulting angle using a specially designed protractor. This process has proved to be reliable, although the precision of the resulting measurement is not very high [3, 4].
However, physicians can no longer ignore the growing integration between smartphone technology and their clinical practice [5]. Smartphones can save significant time and are a powerful tool to keep physicians connected to patient information outside the clinic. An added feature, the embedded positioning sensors make them powerful measuring stations, combined with real-time computing capabilities.
Recently, Shaw et al. [6] proved that measuring the Cobb angle using a non dedicated, consumer-grade iPhone application yielded results similar in quality to the regular protractor process, although the non specific iPhone application could be criticised in that it does not allow storage of the measurement results, nor does it create a database reference for further comparison within patients [6].
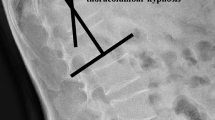
To try to improve on this new technology for measuring Cobb angles, in 2009 we developed a specific iPhone application (CobbMeter, Altavi, Luxembourg) designed to make better use of the position sensor built into the device and its computing capabilities. This application was made available to the public through the iTunes Store in September 2009; it simply measures the angular difference between two positions of the handheld device in the vertical plane. The measurement process consists of two sequential steps: (1) the physician aligns the edge of the device with the edge of the upper vertebra to the deformity and validates the position by clicking on the screen; (2) the handheld device is aligned with the edge of the lower vertebra and is validated again (Figs. 1 and 2). The resulting angle is then printed onto the screen (Fig. 3). Results are stored in a database and can be exported by e-mail to the user.
The precision of the position sensor is 1/10th of a degree, much higher than reading a transparent protractor and tracing lines on radiographs [7]. However, the process of aligning the edge of the device with the vertebral plateau may introduce distortions, since the phone is not transparent, it may interfere with the positioning by hiding part of the information to the eye of the operator. Thus the precision and the reliability of the Cobbmeter need to be measured and proven. Performing such studies concerning the efficiency of new tools is mandatory in obtaining the certifications necessary for everyday clinical use in human health care. Recently, Qiao et al. [8] provided solid evidence to support the use of the application in the clinical field in measuring Cobb angles in scolioses. We provide here similar results in measuring angular kyphoses as a reliability study. Thanks to these studies and declarations of conformities with a quality-based design and decision process, CobbMeter has obtained the CE mark for clinical use in Europe. Obtaining FDA approval is a next and desirable step in its development.
Material and methods
Conventional radiographs were extracted from the records of 20 different patients treated at our institution for thoracic or lumbar fractures. A set of 20 radiographs showing thoracic or lumbar localised kyphoses was offered to a panel of six operators comprising three senior surgeons with fellowship training in spine surgery, and three orthopaedic residents undergoing training in general orthopedics. Radiographs were presented to each operator in a random order and the complete set was randomly measured by each operator a total of four times, using the two different methods twice at two different moments. The line drawing and protractor method was used as standard and described by John Cobb, drawing the superior and inferior endplates of the vertebrae with a dedicated pen and measuring the angle between those two lines after drawing the perpendiculars. Wiping of the drawn lines was done with alcohol immediately after the measurement procedure to allow for further processes. The iPhone method required the operators to select the CobbMeter iPhone application, apply the body of the smartphone vertically on the radiograph plane, align the superior edge of the smartphone accurately to the superior endplate of the superior vertebra of the deformity, then clicking anywhere on the phone’s screen to validate the position. Once the position validated, the smartphone’s superior edge was aligned with the inferior endplate of the lower vertebra to the deformity, and the operator validated the new position by clicking anywhere on the phone’s screen. The dedicated software then computed the angle difference between the two positions in the vertical plane as the measured Cobb angle and displayed it on the smartphone’s screen. A dedicated speech synthesizer would then tell announce measured angle. This process was conducted again at a different time using the same set of radiographs in a different order to measure intraobserver reliability.
Data were collected in a spreadsheet and the statistical analyses were performed using SPSS 16.0 and STATA 11.0. Intra-class correlation coefficients were computed to compare the iPhone application and the standard method using a protractor in Cobb Angle measurement and to assess the intra- and interobserver reliability for both tools.
Results
The mean angle was 17.26° with a standard deviation of 8.798. The descriptive statistics are available for all patients in Table 1.
Results for the intra-class correlation coefficients (ICC) are indicated in Table 2. The ICC is the proportion of variance of a measure due to between-patient variability. It ranges from 0 to 1. An ICC above 0.80 is considered very high and shows a very high reliability among raters [9]. The table reports coefficients with their respective 95 % confidence interval as well as standard deviations.
The ICC between Cobbmeter and protractor for all measures was 0.963, indicating excellent concordance between the two rating tools. The standard deviation for the iPhone measurements was 8.961°, versus 8.650° for the protractor measurements. This difference was not statistically significant. Figure 4 provides a visual representation of the agreement between methods (Cobbmeter vs. protractor).
The intra-observer ICC was 0.977, indicating excellent reproducibility of measurements at different times for all operators. The ICC of the iPhone measurements was 0.983 whereas the ICC for the protractor measurements was 0.970. Figure 5 provides a display of intraobserver variability for both tools.
The interobserver correlation coefficient was 0.965, indicating excellent agreement between all operators throughout the measurement process. The interobserver ICC was 0.973 for the iPhone measurements and 0.958 for the protractor measurements.
The interobserver ICC between fellowship-trained surgeons and general orthopedic residents was 0.989, indicating excellent reliability. The ICC between senior and junior surgeons was 0.992 for the iPhone measurements and 0.985 for the standard protractor measurements.
Consistently, the coefficients for intraobserver and interobserver correlations were higher with the iPhone application than with the regular protractor method. These differences were not statistically significant.
Discussion
Handheld digital devices have invaded the market and the clinical field [10]. These devices are powerful measuring and computing stations that may be put to use to help fulfill clinical tasks [11–14]. Using such a computer appeared to us as a way to improve the everyday practicability of Cobb angle measurement. Shaw et al. [6] already proved that using iPhone measurement in scolioses is a sound process.
Introducing a new way to gather medical information warrants the new method to be confronted with standard practice and prove its usefulness. Reliability studies require a precise process and careful planning to maximise the likelihood of detecting systematic differences [15]. According to calculations the more efficient design in our setting would require an optimum number of 30 radiographs taken from different patients to maximise power. However, we wished to highlight the effects of measuring the Cobb angle with different tools in a rather large panel of different surgeons and to be able to determine the effects of the different operators and differences in training among them (namely, senior versus junior effects), leading to a relatively complicated design as choices had to be made in allocating time and constraint resources efficiently [16]. Each of six different operators has thus had to measure each set of radiographs a total of four times as 480 measures were studied. The design functioned well as the ICC was very high between methods, between operators and levels of training.
The study we conducted shows that using specially developed software in a consumer grade handheld device ensures angle measurements in the kyphotic spine comparable to and highly correlated with the measurements obtained by the standard protractor method first described by John Cobb. Thus the use of the small iPhone for measuring kyphosis angles is supported by our study in terms of precision and reliability, which is added to the convenience of the handheld device, i.e. angles are measured with the same device used to manage one’s schedule and perform phone calls and e-mail communication, thus being always at hand. This virtually alleviates the need for finding a pen and protractor, and drawing lines on radiographs. Shaw et al. [6] and Qiao et al. [8] showed that the iPhone solution quicker.
We need to emphasise at this point that changing the tool used to perform the measurement does not change the spirit and the purpose, which is to provide a point of reference in the course of a treatment and a basis for evaluation of the techniques [17]. New tools appear but the general principles of measurements and the spirit of the process remain [1].
Only the use of the application in measuring kyphosis angles has been evaluated in our study, and in scolioses by Shaw et al. [6] and Qiao et al. [8]. The device may be used for measuring different kinds of angles and the whole range of measurements routinely used in the field of spine and orthopaedic surgery. Although the results of the study are encouraging, further studies are needed to evaluate the performance of the device in different clinical situations.
The application was designed with measuring the Cobb angle in vertical radiographs in mind. Technology evolves and more and more radiographs are presented over computer screens to clinicians. Software tools are not always intuitive or easy to use in the clinical setting; a few software tools have been validated against the standard method of measurement [18]. The use of the iPhone application for measuring Cobb angles on radiographs presented on vertical computer screens is a possible clinical application of the software, although the reliability of the measurement is outside the scope of this study and no assumption can be made at this point concerning the reliability of the measures, as for any comparable software used on screen, in the clinical setting.
Conclusion
New software was developed permitting the use of a simple computer handheld device for clinical measurements in vertebral kyphoses. The reliability analysis shows that measurements are highly correlated with the measurements obtained using the standard method. Further studies are needed to obtain results in other clinical situations such as scoliosis measurement and other spine and non-spine situations. We did a reliability study using the small iPhone application to measure its performance in measuring Cobb angles in kyphoses against the standard procedure using the protractor.
References
Cobb JR (1948) Outline for the study of scoliosis. AAOS Instr Course Lect 5:261–275
Cobb JR (1947) Progress in orthopedic surgery for 1945; conditions involving the spine and thorax, exclusive of those in the lower part of the back. Arch Surg 55(1):76–87
Keynan O, Fisher CG, Vaccaro A, Fehlings MG, Oner FC, Dietz J, Kwon B, Rampersaud R, Bono C, France J, Dvorak M (2006) Radiographic measurement parameters in thoracolumbar fractures: a systematic review and consensus statement of the spine trauma study group. Spine (Phila Pa 1976) 31(5):E156–E165. doi:10.1097/01.brs.0000201261.94907.0d
Ulmar B, Brunner A, Guhring M, Schmalzle T, Weise K, Badke A (2009) Inter- and intraobserver reliability of the vertebral, local and segmental kyphosis in 120 traumatic lumbar and thoracic burst fractures: evaluation in lateral X-rays and sagittal computed tomographies. Eur Spine J 19(4):558–566. doi:10.1007/s00586-009-1231-2
Al-Hadithy N, Gikas PD, Al-Nammari SS (2012) Smartphones in orthopaedics. Int Orthop. doi:10.1007/s00264-012-1527-4
Shaw M, Adam CJ, Izatt MT, Licina P, Askin GN (2011) Use of the iPhone for Cobb angle measurement in scoliosis. Eur Spine J. doi:10.1007/s00586-011-2059-0
Street J, Lenehan B, Albietz J, Bishop P, Dvorak M, Fisher C (2009) Intraobserver and interobserver reliability of measures of kyphosis in thoracolumbar fractures. Spine J 9(6):464–469. doi:10.1016/j.spinee.2009.02.007
Qiao J, Liu Z, Xu L, Wu T, Zheng X, Zhu Z, Zhu F, Qian B, Qiu Y (2012) Reliability analysis of a smartphone-aided measurement method for the Cobb angle of scoliosis. J Spinal Disord Tech. doi:10.1097/BSD.0b013e3182463964
Fleiss JL, Levin BA, Paik MC (2003) Statistical methods for rates and proportions. Wiley series in probability and statistics, 3rd edn. J. Wiley, Hoboken, NJ
Editorial (2010) Mobile computing platforms such as the iPhone are beginning to make inroads into the laboratory-serious prospect or fairy tale? Nat Methods 7(2):87
Choudhri AF, Radvany MG (2010) Initial experience with a handheld device digital imaging and communications in medicine viewer: OsiriX mobile on the iPhone. J Digit Imaging 24(2):184–189. doi:10.1007/s10278-010-9312-7
Ciemins E, Coon P, Sorli C (2010) An analysis of data management tools for diabetes self-management: can smart phone technology keep up? J Diabetes Sci Technol 4(4):958–960
Colvard MD, Naiman M, Danziger L, Hanley L (2010) Handheld directed energy sensor for environmental monitoring and clinician safety. Aviat Space Environ Med 81(6):602–604
Gamble KH Wireless Tech Trends (2010) Trend: smartphones. Healthc Inform 27(2):24, 26–27
Shoukri MM, Asyali MH, Donner A (2004) Sample size requirements for the design of reliability study: review and new results. Stat Methods Med Res 13(4):251–271. doi:10.1191/0962280204sm365ra
Shoukri MM, Asyali MH, Walter SD (2003) Issues of cost and efficiency in the design of reliability studies. Biometrics 59(4):1107–1112
Cobb JR (1960) The problem of the primary curve. J Bone Joint Surg Am 42-A:1413–1425
Tanure MC, Pinheiro AP, Oliveira AS (2010) Reliability assessment of Cobb angle measurements using manual and digital methods. Spine J 10(9):769–774
Acknowledgments
With special thanks to Allen Cobb for his help and comments in developing this computer application.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jacquot, F., Charpentier, A., Khelifi, S. et al. Measuring the Cobb angle with the iPhone in kyphoses: a reliability study. International Orthopaedics (SICOT) 36, 1655–1660 (2012). https://doi.org/10.1007/s00264-012-1579-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1579-5