Abstract
Purpose
The purpose of our study is to evaluate the clinical results of anatomical reconstruction of the lateral ligaments with semitendinosus allograft.
Methods
Thirty-six patients with chronic lateral instability underwent anatomical reconstruction of the lateral ligaments of the ankle with semitendinosus allograft. The American Orthopaedic Foot and Ankle Society Ankle-Hindfoot Scale score (AOFAS score) and the Karlsson score were used to evaluate the clinical results before and after surgery.
Results
A total of 35 patients (97.2 %) (36 ankles) were followed up for a mean of 37.9 months. The mean AOFAS score improved from 42.3 ± 4.9 points preoperatively to 90.4 ± 6.7 postoperatively. The mean Karlsson score improved from 38.5 ± 3.2 preoperatively to 90.1 ± 7.8 postoperatively.
Conclusions
Anatomical reconstruction of the lateral ligaments with semitendinosus allograft achieves a satisfactory surgical outcome for chronic ankle instability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Ankle sprains are reported to be the most common sports injury and account for 10∼15 % of sports-related injuries [1–3]. Although the majority of the patients have successful results after conservative treatment, up to 20-40 % have mechanical instability requiring operative intervention [4, 5].
There are various operative procedures to treat chronic lateral ankle instability. If the patient has a weak remnant of the lateral ligament, generalised joint laxity or previous failed operation for lateral ankle instability, anatomical lateral ligament reconstruction is always suggested [6].
Several kinds of graft are used for the anatomical ligament reconstruction. Compared to the autograft, an allograft has the advantages of no donor site morbidity, shorter operation time and less postoperative pain [7]. Furthermore, with the improvement of the sterilisation technique, some potential complications, for example, the potential for disease transmission, osteolytic reactions, etc., have been markedly decreased [7, 8]. Up to now, there have been few reports about the use of allograft for lateral ankle ligament reconstruction. We use a semitendinosus allograft in lateral ankle ligament reconstruction and propose that anatomical reconstruction of the lateral ligaments with this allograft can achieve a satisfactory surgical outcome for chronic ankle instability. The purpose of this study was to evaluate our results of this reconstructive surgery using a semitendinosus allograft.
Materials and methods
Patients
From April 2007 to September 2009, a total of 36 patients (37 ankles) who were diagnosed with chronic lateral ankle instability underwent anatomical lateral ligament reconstruction using semitendinosus allograft. There were 24 male patients (24 ankles) and 12 female patients (13 ankles) with a mean age of 29.2 years (range 18–52 years). The mean time from initial injury to surgery was 6.7 years (range 3–14 years). Preoperative magnetic resonance imaging was performed to assess intra-articular lesions and bone bruises. Preoperative stress radiography was not routinely applied because of its poor relevance in evaluating chronic ankle instability [9].
The criteria for the patients with chronic ankle instability to undergo ligament reconstruction were [6]: (1) previous failed ligament repair; (2)severe attenuation of the ligament stump found during the operation; (3) generalised joint laxity, which was defined by the criteria of Beighton et al. [10]; (4) high-demand, strenuous workers or athletes; and (5) overweight.
The first author performed the surgery on all patients. The study received ethical approval from the Human Ethics Research Board of our hospital.
The surgery was performed under spinal anaesthesia. The patients were placed in the supine position. A tourniquet was applied at the thigh. An ankle arthroscopic procedure was performed first. With noninvasive ankle traction, a 2.7-mm, 30° arthroscope was inserted through a standard anteromedial portal to examine the ankle joint. Any intra-articular disorders were assessed and managed, with debridement for grade I or II cartilage injuries, microfracture for grade III or IV cartilage injuries, excision of the osteophytes, impinged soft tissue, synovitis or fibrous tissue adherent to the lateral gutter and removal of loose bodies [11].
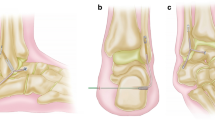
The anatomical reconstruction of the lateral ankle ligament was performed after the arthroscopic procedure. A straight skin incision was made from the tip of the distal fibula to the talus insertion of the anterior talofibular ligament (ATFL). The anterior edge of the distal fibula was exposed to show the insertion of the ATFL and calcaneofibular ligament (CFL). A second straight incision was made posterior to the fibula, and then two oblique 3.5-mm tunnels were created in the fibula beginning seven and 13 mm proximal to the tip of the fibular, respectively, and drilled in the superior posterior direction. Another two 3.5-mm converging tunnels just distal to the edge of the cartilage and 18 mm proximal to the subtalar joint were made the talus [12]. A third straight incision was made parallel and below the first incision to expose the tubercle of the calcaneus. A Bill’s pin was drilled just at the tubercle of the calcaneus and passed to the medial aspect. The fifth tunnel was made with a six millimetre reamer 25 mm in length (Figs. 1 and 2).
The skin incisions. a The first incision was from the tip of the distal fibula to the talus insertion of the ATFL. b The second incision was posterior to the fibula to show the proximal ends of the fibular tunnels. c The third incision was parallel and below the first incision to show the tubercle of the calcaneus
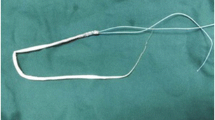
A semitendinosus allograft (Osteolink Biomaterial Co., Ltd. Hubei, China) of 20 cm length was used. The graft was reconstituted in sterile saline with antibiotics for 15 min at room temperature and trimmed to 3.5 mm in diameter. After pretension for 15 min at a force of 15 N, one end of the graft was pulled into the bone tunnel of the calcaneus and fixed with a bioabsorbable screw (Smith & Nephew, Andover, MA, USA) with a diameter of 7 mm. The other end of the graft was routed across, beneath the peroneal tendons, though the posterior tunnel in the fibula from the anterior inferior to posterior superior direction. The graft was then routed back through the anterior tunnel in the fibula; after that, the graft passed though the two tunnels in the talus. Full range ankle movements were performed 20 times to confirm the isometricity and adjust the tension of the graft. The free end of the graft was sutured to the tendon itself with the ankle joint in a neutral position. The capsule was sutured back to cover the graft, and the incision was closed (Fig. 2).
After the operation, the ankle was immobilised in a neutral position using a short leg cast. Rehabilitation exercises including isometric contraction of muscle groups around the ankle joint were started from the day after surgery. Six weeks after the surgery, the cast was changed to an ankle orthosis and passive range of motion was encouraged. Eight weeks after the surgery, weight-bearing was permitted. Strenuous activity and contact sports were not allowed until 12 months after the surgery.
The patients were clinically evaluated before the operation and at follow-up using the American Orthopaedic Foot and Ankle Society (AOFAS) score and Karlsson score. The hindfoot motion was measured using a goniometer with the patient prone and the knee in 90° of flexion and the ankle in 0° of dorsiflexion. The range of motion for dorsiflexion and plantar flexion were also recorded at both ankle joints. A manual anterior drawer test and inversion tests were also performed in all patients.
Paired-sample t tests were used for statistical analysis. The significance level was defined as P < 0.05. Analysis was performed by a statistician using SPSS software, version 18.0 (SPSS, Chicago, IL, USA).
Results
No vascular or nerve complication occurred during or after the operation in any patients. Two patients had poor wound healing, which resolved after changing the dressing. Another patient had discomfort at the site of 4 cm above the tip of the fibula, where the graft was routed across the fibula, but this did not affect his activities of daily living or sports activities.
A total of 35 patients (97.2 %) (36 ankles) were followed up for a mean of 37.9 months (range 24–54 months). The mean AOFAS score improved from 42.3 ± 4.9 points preoperatively to 90.4 ± 6.7 postoperatively (P = 0.000). The mean Karlsson score improved from 38.5 ± 3.2 preoperatively to 90.1 ± 7.8 postoperatively (P = 0.000).
In the 34 patients with unilateral ankle ligament reconstruction, average dorsiflexion, as measured with a goniometer, was 14.8 ± 1.8°, compared with 15.1 ± 1.7° in the non-operated ankle (P = 0.092), and average plantar flexion was 45.0 ± 4.7°, compared with 46.7 ± 2.6 in the non-operated ankle (P = 0.073). The average hindfoot motion was 18.9 ± 2.4°, compared with 19.0 ± 2.4° in the non-operated ankle (P = 0.240). The differences between the results of the operated ankle and the non-operated ankle were not statistically significant. For the patient with reconstruction of both ankle ligaments, the dorsiflexions were 17.0 and 17.2°, respectively, the plantar flexions were 48.1 and 48.3°, respectively, and the hindfoot motions were 21.0 and 20.7°, respectively.
Manual stress testing showed that 33 patients (34 ankles) were stable in both the anterior drawer and the inversion tests. Two patients (two ankles) showed a mild positive anterior drawer test of the talus. One patient was found to have excessive generalised joint laxity. The results of the patient were excellent (AOFAS score of 95 and Karlsson score of 97). The other patient returned to fiercely competitive sports at five months after the operation and felt progressive relaxation of the ankle joint. Then he gave up the sports activity until the follow-up. The results of the patient were fair (AOFAS score of 80 and Karlsson score of 72).
Discussion
Allografts have been used widely in primary and revision ligament reconstruction [13, 14]. Several kinds of allograft, including tibiotalar bone-tendon allograft, allogeneic fascia lata, toe flexor and/or extensor tendon allograft or semitendinosus allograft, have been used in lateral ankle ligament reconstruction [8, 15–18]. Our study used semitendinosus allograft and achieved a satisfactory result. As far as we know, until now there have been two articles describing the use of semitendinosus allograft for reconstruction of the lateral ankle ligament. Caprio et al. reported on 11 patients who underwent ligament reconstruction using allogeneic semitendinosus tendon allograft. The average AOFAS scores improved from 29.6 to 55.4 points at an average follow-up of 14.1 months [8]. Jung et al. reported a better results than those of Caprio et al. In their study, 27 patients (28 ankles) underwent anatomical reconstruction of the ATFL and CFL using a semitendinosus tendon allograft and then repair of the ATFL and capsule. The results showed that the median visual analogue scale (VAS) pain score decreased from 6 to 2 (P < 0.05), the median AOFAS score improved from 63 to 91 and the median Karlsson-Peterson score also significantly improved from 55 to 80. Eighty-eight per cent of the patients were satisfied with the surgery and were significantly improved [18]. Our results are similar to that of the latter. There might be several factors that would induce this difference.
Firstly, Caprio et al. used the tip of the distal fibula as the new insertion of the CFL; Burks and Morgan reported that the centres of the insertion of the ATFL and the CFL at the fibula are reported to be on average 10.1 and 8.5 mm proximal to the tip of the fibula, respectively, and the attachments of the two ligaments are overlapped [19]. Therefore, it is suggested that procedures that use the tip of the fibula as the new insertion of the CFL are not anatomical and do not reproduce the correct anatomy of the ligaments, and thus might not reproduce the normal biomechanics of the ankle and subtalar joint [20]. To achieve an anatomical reconstruction, one should drill the two holes very close in the fibular side or drill one hole for both ligaments [21–23].
Our study and the study of Jung et al. both used a two-tunnel technique to reconstruct the anatomical attachments in the fibula. The graft in the fibular tunnel was fixed by the suspension on the bone bridge at the posterior side; this method permits the holes in the fibula for the ATFL and CFL to be very close. Bahr et al. showed that the graft force patterns observed during loading after this anatomical reconstruction procedure resemble those observed in the intact ankle [24]. In both studies, the patients have a similar range of motion as that of a normal hindfoot joint and subjective satisfaction about the range of motion.
Secondly, the time when the patients were permitted to go back to sports in this study (three to four months) was earlier than that of our study (12 months). It has been reported that allografts have a slower reincorporation rate and remodelling when compared with autografts [25, 26]. Therefore, if the patient goes back to high-activity sports too early, it might increase the load of the allograft, which has not yet completed remodelling, and then affect the results at the follow-up. We justify 12 months postoperatively as the time to go back to sports based on the experience of anterior cruciate ligament (ACL) reconstruction and the healing characteristics of allografts [7, 27, 28]. Although Jung et al. did not report the time when their patients returned to sports, one patient in our study went back to fiercely competitive sports at five months after the operation and a fair result with a mild anterior drawer test was found. So we believe it is necessary for patients who undergo ligament reconstruction by tendon allograft to start sports at a later time.
Thirdly, the study by Caprio et al. contained 11 patients; the small number of patients might affect the results of the study. The study by Jung et al. had 27 patients (28 ankles) and our study had 35 patients (36 ankles). The relatively larger number of the patients would be prone to have a more reliable result.
There are still some disadvantages in our study. Firstly, there is no objective quantified method to evaluate ankle stability. Some articles employ stress X-ray to approach this issue; we did not select X-ray because of its poor correlation with ankle stability. We believe the subjective feeling of the patient together with the manual test can evaluate ankle stability sufficiently. Secondly, we did not evaluate the maturity and reincorporation of the graft at the follow-up. To clarify these issues, additional research, including special methods such as contrast-enhanced magnetic resonance imaging or biopsy, is required.
Conclusions
Based on the results of our study, we believe that anatomical reconstruction of the lateral ligaments with semitendinosus allograft achieves a satisfactory surgical outcome for chronic ankle instability.
References
Lassiter TE Jr, Malone TR, Garrett WE Jr (1989) Injury to the lateral ligaments of the ankle. Orthop Clin North Am 20:629–640
McConkey JP (1987) Ankle sprains, consequences and mimics. Med Sport Sci 23:39–55
MacAuley D (1999) Ankle injuries: same joint, different sports. Med Sci Sports Exerc 31:S409–S411
Jackson W, McGarvey W (2006) Update on the treatment of chronic ankle instability and syndesmotic injuries. Curr Opin Orthop 17:97–102
Karlsson J, Lansinger O (1993) Chronic lateral instability of the ankle in athletes. Sports Med 16:355–365
Baumhauer JF, O’Brien T (2002) Surgical considerations in the treatment of ankle instability. J Athl Train 37:458–462
Carey JL, Dunn WR, Dahm DL, Zeger SL, Spindler KP (2009) A systematic review of anterior cruciate ligament reconstruction with autograft compared with allograft. J Bone Joint Surg Am 91:2242–2250
Caprio A, Oliva F, Treia F, Maffulli N (2006) Reconstruction of the lateral ankle ligaments with allograft in patients with chronic ankle instability. Foot Ankle Clin 11:597–605
Frost SC, Amendola A (1999) Is stress radiography necessary in the diagnosis of acute or chronic ankle instability? Clin J Sport Med 9:40–45
Beighton P, Solomon L, Soskolne CL (1973) Articular mobility in an African population. Ann Rheum Dis 32:413–418
Hua Y, Chen S, Li Y, Chen J, Li H (2010) Combination of modified Broström procedure with ankle arthroscopy for chronic ankle instability accompanied by intra-articular symptoms. Arthroscopy 26:524–528
van den Bekerom MP, Oostra RJ, Alvarez PG, van Dijk CN (2008) The anatomy in relation to injury of the lateral collateral ligaments of the ankle: a current concepts review. Clin Anat 21:619–626
Fanelli GC, Tomaszewski DJ (2007) Allograft use in the treatment of the multiple ligament injured knee. Sports Med Arthrosc 15:139–148
Sikka RS, Narvy SJ, Vangsness CT Jr (2011) Anterior cruciate ligament allograft surgery: underreporting of graft source, graft processing, and donor age. Am J Sports Med 39:649–655
Horibe S, Shino K, Taga I, Inoue M, Ono K (1991) Reconstruction of lateral ligaments of the ankle with allogeneic tendon grafts. J Bone Joint Surg Br 73:802–805
Nakata K, Shino K, Horibe S, Natsu-ume T, Mae T, Ochi T (2000) Reconstruction of the lateral ligaments of the ankle using solvent-dried and gamma-irradiated allogeneic fascia lata. J Bone Joint Surg Br 82:579–582
Su EP, Healey JH (2003) Salvage reconstruction for lateral ankle instability using a tendon allograft. Clin Orthop Relat Res 415:232–238
Jung HG, Kim TH, Park JY, Bae EJ (2011) Anatomic reconstruction of the anterior talofibular and calcaneofibular ligaments using a semitendinosus tendon allograft and interference screws. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-011-1666-y
Burks RT, Morgan J (1994) Anatomy of the lateral ankle ligaments. Am J Sports Med 22:72–77
Pagenstert GI, Valderrabano V, Hintermann B (2005) Lateral ankle ligament reconstruction with free plantaris tendon graft. Tech Foot Ankle Surg 4:104–112
Sugimoto K, Takakura Y, Kumai T, Iwai M, Tanaka Y (2002) Reconstruction of the lateral ankle ligaments with bone-patellar tendon graft in patients with chronic ankle instability: a preliminary report. Am J Sports Med 30:340–346
Takao M, Oae K, Uchio Y, Ochi M, Yamamoto H (2005) Anatomical reconstruction of the lateral ligaments of the ankle with a gracilis autograft: a new technique using an interference fit anchoring system. Am J Sports Med 33:814–823
Ahn JH, Choy WS, Kim HY (2011) Reconstruction of the lateral ankle ligament with a long extensor tendon graft of the fourth toe. Am J Sports Med 39:637–644
Bahr R, Pena F, Shine J, Lew WD, Tyrdal S, Engebretsen L (1997) Biomechanics of ankle ligament reconstruction. An in vitro comparison of the Broström repair, Watson-Jones reconstruction, and a new anatomic reconstruction technique. Am J Sports Med 25:424–432
Muramatsu K, Hachiya Y, Izawa H (2008) Serial evaluation of human anterior cruciate ligament grafts by contrast-enhanced magnetic resonance imaging: comparison of allografts and autografts. Arthroscopy 24:1038–1044
Malinin TI, Levitt RL, Bashore C, Temple HT, Mnaymneh W (2002) A study of retrieved allografts used to replace anterior cruciate ligaments. Arthroscopy 18:163–170
Horibe S, Shino K, Nagano J, Nakamura H, Tanaka M, Ono K (1990) Replacing the medial collateral ligament with an allogenic tendon graft. An experimental canine study. J Bone Joint Surg Br 72:1044–1049
Barrett GR, Luber K, Replogle WH, Manley JL (2010) Allograft anterior cruciate ligament reconstruction in the young, active patient: Tegner activity level and failure rate. Arthroscopy 26:1593–1601
Author information
Authors and Affiliations
Corresponding author
Additional information
The research was supported by the National Natural Science Foundation of China (Grant No. 81101391)
Rights and permissions
About this article
Cite this article
Hua, Y., Chen, S., Jin, Y. et al. Anatomical reconstruction of the lateral ligaments of the ankle with semitendinosus allograft. International Orthopaedics (SICOT) 36, 2027–2031 (2012). https://doi.org/10.1007/s00264-012-1577-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1577-7