Abstract
Purpose
In undetached osteochondral lesions (OCL) of the talus both revitalisation of the subchondral necrosis and cartilage preservation are essential. For these cases, we assess the results of minimally invasive retrograde core drilling and cancellous bone grafting.
Methods
Forty-one osteochondral lesions of the talus (12x grade I, 22x grade II and 7x grade III according to the Pritsch classification, defect sizes 7–14 mm) in 38 patients (mean age 33.2 years) treated by fluoroscopy-guided retrograde core drilling and autologous cancellous bone grafting were evaluated by clinical scores and MRI. The mean follow-up was 29.0 (±13) months.
Results
The AOFAS score increased significantly from 47.3 (±15.3) to 80.8 (±18.6) points. Lesions with intact cartilage (grades I and II) had a tendency to superior results than grade III lesions (83.1 ± 17.3 vs. 69.4 ± 22.2 points, p = 0.07). First-line treatments and open distal tibial growth plates led to significantly better outcomes (each p < 0.05). Age, gender, BMI, time to follow-up, defect localisation or a traumatic origin did not influence the score results. On a visual analogue scale pain intensity reduced from 7.5 (±1.5) to 3.7 (±2.6) while subjective function increased from 4.6 (±2.0) to 8.2 (±2.3) (each p < 0.001). In MRI follow-ups, five of the 41 patients showed a complete bone remodelling. In two cases demarcation was detectable.
Conclusions
The technique reported is a highly effective therapeutic option in OCL of the talus with intact cartilage grades I and II. However, second-line treatments and grade III lesions with cracked cartilage surface can not be generally recommended for this procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Revitalising the subchondral bone is the therapeutic rationale in osteochondral lesions (OCL) of the talus. This can be achieved by anterograde drilling, microfracturing, cancellous bone grafting or osteochondral plugs depending on the local cartilage condition. In principal, these techniques are restricted to unstable lesions and cracked cartilage surfaces [1–5].
In contrast, retrograde drilling penetrates the necrotic sclerotic zone for bone marrow stimulation without damaging the cartilage surface. It can be combined with retrograde autologous cancellous bone-grafting. The operative principles are based on a technique described by Wagner [6] for osteochondritis dissecans in the knee and were adopted to the talus by Conti [7]. Our study reports on the outcome of minimally invasive retrograde core drilling and autologous cancellous bone grafting guided by fluoroscopy and arthroscopy in talar OCL.
Material and methods
The osteochondral talus lesion was diagnosed preoperatively by radiographs and MRI. Inclusion criteria were symptomatic undisplaced osteochondral lesions (OCL) or osteochondritis dissecans (OD) of the talus grade I to III according to the radiological classification of Berndt and Harty [8]. The minimal defect diameter demanded for inclusion was seven millimetres as measured by MRI. At index arthroscopy, the lesions were staged according to the classification of Pritsch [9] such that intact overlying cartilage was grade I, soft overlying cartilage was grade II and frayed overlying cartilage was grade III. In this study, small cracks or chondral fissures (grade III) were treated if at least three quarters of the circumference of the cartilage was intact and the defect appeared stable on hook tip probing. Exclusion criteria were: lesions other than grade III, unstable lesions on intraoperative hook tip probing, ligamentous instability at clinical examination and a history of ankle fracture. The clinical outcome was assessed by the American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot Scale [10]. The patient's self assessment was recorded on a visual analogue scale (VAS, 0–10 cm max) for pain and function. Additionally, MRI with coronal and sagittal planes (T1- and T2-spin-echo sequences, 1.5 T, Magnetom Symphony, Siemens, Germany) were used at follow-up.
Statistical analysis
Statistics of descriptive data were calculated by standard formulas (arithmetic mean, standard deviation, range, frequency). All continuous variables are presented in terms of mean ± standard deviation of the mean. Comparison between paired data and independent groups was performed by using the Student's t test or rank-sum test for not normally distributed values. Factor analysis of patient's age, BMI and time to follow-up was calculated using the Pearson product–moment correlation coefficient (r). A p-value less than 0.05 was regarded as statistically significant. Statistical analysis was performed using the SigmaStat (Systat Software, San Jose, CA, USA) software package.
Study population
Between 2004 and 2009 a total of 48 consecutive focal grade I–III osteochondral lesions of the talus were treated by fluoroscopy-guided retrograde core drilling and autologous cancellous bone grafting. All lesions were considered chronic with persistent symptoms for over six months and after failed conservative treatment. The population of our study consisted of 16 female and 22 male patients with a total of 41 talar lesions including three male bilateral lesions. The mean measured defect-size was nine mm with a range from seven to 14 mm. All procedures were performed with a matching drill core diameter from seven to nine mm.
The average age was 33.2 years (11–56 years). The mean BMI was 24.8 (±3.6) kg/m². In 27/41 (66 %) cases a trauma history (sprain, compression) was reported. Most defects were located at the medial talus (36/41) and predominantly found at the apical rim (29/41). There were four lateral and one central localisations. Thirty-four of 41 cases were primary interventions, 4/41 had undergone previous drilling or microfracturing and 3/41 cases had undergone shaving prior to the retrograde drilling at the talar lesion. In nine cases the growth plate of the distal tibial epiphysis was detectable. None of these patients had a grade III lesion. While in the first-line group only 5/34 (15 %) lesions showed partially cracked cartilage (grade III), there were 2/7 (29 %) similar observations in the second-line treatment group. Generally, no patient was free of pain, while four patients suffered from pain at rest.
The follow-up was 12–54 months with a mean of 29 (±13) months. Intraoperative grading of the lesions revealed 12/41 as grade I, 22/41 as grade II and 7/41 as grade III. Arthroscopic concurrent therapy consisted of partial synovectomy in 28/41 (68 %) cases and removal of minor anterior tibial spurs in 4/41 (9 %) cases.
Operative technique
Primarily, all patients underwent index ankle arthroscopy in a supine straight leg position without joint distractor. Anteromedial and anterolateral standard portals and a femoral tourniquet (350 mm Hg) were used. The talus lesion was exposed by plantar flexion and staged according to the Pritsch classification [9]. Under fluoroscopic control a 2.0-mm pilot Kirschner wire was positioned transtalar from the opposite talar neck into the subchondral sclerotic zone (Fig. 1). No drill guide was used. Correct aiming was verified in AP and lateral plain view radiographs. The sclerotic zone was gently penetrated by the loss of resistance technique by core drilling and a cancellous bone cylinder was harvested (Fig. 2). The specimen was used to confirm the pathology and the location of the drilling by detecting the sclerotic zone at the top of the drilling cylinder. The correct penetration of the sclerotic zone was checked by insertion of a sharp spoon under fluoroscopy. If necessary, the drilling was gently repeated. The drilling diameter ranged from seven to nine mm. For larger defects, an additional transtalar debridement was added using a sharp spoon (Fig. 3). After dissection of the sclerotic area at the top, the core drill was reloaded with the viable autologous cancellous bone cylinder. After insertion into the drilling canal, the bone cylinder was plugged underneath the chondral roof through the drill-hole in a press-fit manner (Fig. 4) by mild tapping and simultaneous removal of the core drill. No additional bone harvesting, e.g. from the iliac crest, was performed. At the end of the surgery, the lesion site was arthroscopically re-evaluated for possible iatrogenic damage. Postoperative rehabilitation consisted of six weeks of partial weight-bearing. Full range of motion was allowed immediately. No cast or ankle bracing was provided. Impact sports activities were restricted for six months.
Results
The overall AOFAS score increased from 47.3 (±15.3) points at baseline to 80.8 (±18.6) points at follow-up. The mean overall improvement was 33.5 (±18.4) points. This was mainly caused by pain reduction. Major preoperative symptom was moderate daily (16/41) or severe almost always present pain (25/41). Postoperatively, 26/41 patients reported no or mild occasional pain, 11/41 moderate daily pain and 4/41 severe, almost always present pain. The results of the AOFAS score and its subscales are shown in Table 1.
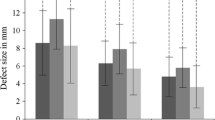
Patients were divided into subgroups by arthroscopic grade and demographic data (Fig. 5, Table 2). Within each subgroup the AOFAS score improvement was significant (p < 0.01). All follow-ups were comparable (p > 0.05, data not shown). In grade I and II lesions better results were obtained compared to grade III lesions. There was a statistically significant difference between grade I and grade III lesions at follow-up (p < 0.01, t-test). With the numbers available no statistical difference associated with a partially cracked cartilage surface (grade I + II vs. grade III) was found (p = 0.076, t-test). Patients with or without a substantial ankle trauma history did show a nearly identical improvement of 33.9 (±17.5) vs. 31.9 (±20.5) points and almost identical score results (p = 0.886, t-test). However, first-line treatments developed markedly better with 36.0 (±17.9) points versus 21.2 (±17.9) points in second-line treatments with significance at most recent AOFAS score (p = 0.009, rank-sum test). Open distal tibial growth plates also led to significantly better results in the AOFAS score at follow-up (p = 0.041, rank-sum test). No significant differences were detected for age, gender, BMI, and localisation (medial/lateral), and time to follow-up did not influence the score results (data not shown). The mean pain intensity presented on a VAS (0–10 max) decreased from 7.5 (±1.5) to 3.7 (±2.6). The subjective functional status estimated on the VAS (0–10 max) revealed a remarkable increase from 4.6 (±2.3) to 8.2 (±2.0). Both differences were statistically significant (each p < 0.001, t-test). Thirty-five of 41 (85 %) patients were satisfied with their result. Five patients complained of ankle swelling for up to 12 weeks postoperatively. Two cases of minor hypesthesia of the forefoot were reported. One delayed superficial wound healing was documented. No ankle joint infection or deep vein thrombosis was seen. No further operative interventions were recorded.
American Orthopaedic Foot and Ankle Society (AOFAS) score results by arthroscopic stage according to Pritsch [9] (*p < 0.05)
In MRI follow up two patients showed progression into detachment associated with AOFAS scores of 71/76 points. A revision has so far been declined by these two patients. All other patients did show an intact cartilage surface with aspects of complete subchondral bone remodelling in five patients. No impaction of the OCL zone occurred. No stress fracture or necrosis of the talus occurred. No joint space narrowing was seen.
Discussion
Comparing outcome in the treatment of OCL of the talus is limited by lack of homogeneity of the population, defect sizes and different operative techniques. Neither common therapeutic concepts nor randomised clinical trials can be found [1, 11]. Small, low-grade, acute and stable lesions in younger patients are reported to have a moderate success rate of 25–50 % with conservative treatment [12–14]. For any other condition, operative revision should be provided. In most studies, the diameter of the lesion did not exceed 15 mm and some studies only reported about rather small defect diameters of less than seven mm [1, 2].
Preserving an intact cartilage layer is the therapeutic paradigm in stable lesions and therefore retrograde drilling techniques should be recommended in these cases. Kono et al. [15] reported superior results of retrograde drilling versus transmalleolar drilling in a series of 30 patients with undetached lesions. These lesions can be addressed accurately by the use of fluoroscopy or computer-assisted navigation. Navigation could provide a more accurate aiming, however requires more complex and cost-intensive hardware support [16, 17].
Studies of retrograde drilling and bone grafting in OCL in the talus are rare. Lee and Mercurio reported on complete healing in a single case of a talus OD after six months in a preliminary report [18]. Additionally, Taranow et al. [19] stated an improvement of the AOFAS score from a mean of 53.9 to 82.6 points in a rather non homogenous population. Takao et al. [20] compared anterior arthroscopic drilling and retrograde cancellous bone plug transplantation in large subchondral defects (10–17 mm) in the ankle. At second-look arthroscopy after one year, the lesion had disappeared in 74 % with cancellous bone plugging and in only 7 % with drilling. Additionally, there were higher AOFAS scores in the bone plugging group at two years (95.8 vs. 88.2 points, p < 0.0001). They recommended retrograde bone plugging in OCL with large subchondral lesions.
In our study the mean age of the patients was slightly higher than in literature findings. A history of a substantial trauma was less frequent in comparison though [1]. Best AOFAS score results were predominantly seen in grade I with 88.7 (±13.4) and in grade II with 80.1 (±18.7) points, whereas grade III lesions only reached 69.2 (±22.2) points. The poorer results in grade III lesions seem to indicate that even partial cracks of the cartilage surface lead to inferior clinical results. Moreover, twice as many grade III lesions were found in second-line treatment (2/7) than in first-line treatment (5/34), possibly hinting at higher risks of failure for secondary interventions with this procedure. Extended techniques such as arthroscopic or open debridement with drilling and/or anterior cancellous bone grafting, osteochondral cylinder transfer or autologous chondrocytes implantation can be alternative treatments here. The limited value of MRI after talus drilling has been reported in literature [2, 21, 22]. In our study, clear interpretation of the repair process in MRI follow-up was typically handicapped by persistent metal drilling artefacts. For this reason, the clinical course seems to provide more relevant information for outcome evaluation. Outcome dependency on growth plate status and grade of the lesion as found in the literature is also reflected in our study [14, 23].
In comparison to single or multiple Kirschner wire drilling, matching the drill diameter to the lesion results in a markedly expanded subchondral necrosectomy. Adding a subchondral cancellous bone grafting without penetrating the cartilage surface promotes the bony revitalising processes. The defect sizes from seven to 14-mm diameter treated in our study represent typical mid-size talus lesions. In consequence, a minimal defect size correlated to the smallest drill diameter (here seven mm) is obligatory for this technique. Smaller defects should be addressed by retrograde Kirschner wire drilling instead.
With various treatment options available for OCL in the talus an accurate estimation of the condition of lesion is essential for an appropriate treatment. For this purpose, different imaging modalities such as conventional radiographs and MRI have to be taken into account. Nevertheless, our results imply that dynamic evaluation and arthroscopic tip probing provides additional important information for the choice of therapy. With intact cartilage surfaces our technique has proven effective in mid-size OCL of the talus after failed conservative therapy. The main advantages are its minimally invasive technique without need for malleolar ostetomy, additional bone grafting, aiming devices or navigation. However, disrupted surface integrity resulted in poorer outcomes indicating insufficient healing potential of cancellous bone grafting and subchondral revitalisation in these cases. This may be due to persistent cartilage detachment from the subchondral bone resulting in abnormal micromotion and shear forces under load and subchondral invasion of synovial fluid. In consequence, we recommend this technique for stable OCL lesions with intact cartilage surface after failed conservative treatment. In any other case, alternatives such as arthroscopic or open debridement with drilling and/or anterior cancellous bone grafting, osteochondral cylinder transfer or autologous chondrocytes implantation should be preferred. In the complex field of therapeutic strategies in talus OCL, further comparative long-term studies are needed for comprehensive treatment algorithms.
Conclusion
Our results indicate that fluoroscopy-guided retrograde core drilling and autologous cancellous bone grafting is an efficient option for stable mid-size OCL of the talus with intact cartilage surface after failed conservative treatment. Subchondral necrosectomy and bone grafting provide extended revitalisation for OCL healing. Open distal tibial growth plates and first-line treatments showed significantly better outcomes. Performed as a cartilage preserving minimally invasive technique, no additional bone harvesting or aiming devices are necessary. With inferior AOFAS score results this technique cannot be recommended for lesions with disrupted surface integrity.
References
Zengerink M, Szerb I, Hangody L, Dopirak RM, Ferkel RD, van Dijk CN (2006) Current concepts: treatment of osteochondral ankle defects. Foot Ankle Clin 11:331–359
Takao M, Ochi M, Naito K, Uchio Y, Kono T, Oae K (2003) Arthroscopic drilling for chondral, subchondral, and combined chondral-subchondral lesions of the talar dome. Arthroscopy 19:524–530
Draper SD, Fallat LM (2000) Autogenous bone grafting for the treatment of talar dome lesions. J Foot Ankle Surg 39:15–23
Hangody L, Kish G, Modis L, Szerb I, Gaspar L, Dioszegi Z, Kendik Z (2001) Mosaicplasty for the treatment of osteochondritis dissecans of the talus: two to seven year results in 36 patients. Foot Ankle Int 22:552–558
Becher C, Thermann H (2005) Results of microfracture in the treatment of articular cartilage defects of the talus. Foot Ankle Int 26:583–589
Wagner H (1964) Surgical treatment of osteochondritis dissecans, a cause of arthritis deformans of the knee. Rev Chir Orthop Reparatrice Appar Mot 50:335–352
Conti SF, Taranow WS (1996) Transtalar retrograde drilling of medial osteochondral lesions of the talar dome. Operat Tech Orthop 6:226–230
Berndt AL, Harty M (1959) Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am 41-A:988–1020
Pritsch M, Horoshovski H, Farine I (1986) Arthroscopic treatment of osteochondral lesions of the talus. J Bone Joint Surg Am 68:862–865
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15:349–353
Hunt SA, Sherman O (2003) Arthroscopic treatment of osteochondral lesions of the talus with correlation of outcome scoring systems. Arthroscopy 19:360–367
Canale ST, Belding RH (1980) Osteochondral lesions of the talus. J Bone Joint Surg Am 62:97–102
Letts M, Davidson D, Ahmer A (2003) Osteochondritis dissecans of the talus in children. J Pediatr Orthop 23:617–625
Bruns J, Rosenbach B (1992) Osteochondrosis dissecans of the talus. Comparison of results of surgical treatment in adolescents and adults. Arch Orthop Trauma Surg 112:23–27
Kono M, Takao M, Naito K, Uchio Y, Ochi M (2006) Retrograde drilling for osteochondral lesions of the talar dome. Am J Sports Med 34:1450–1456
Kendoff D, Geerling J, Mahlke L, Citak M, Kfuri M Jr, Hufner T, Krettek C (2003) Navigated Iso-C(3D)-based drilling of a osteochondral lesion of the talus. Unfallchirurg 106:963–967
Rosenberger RE, Fink C, Bale RJ, El Attal R, Muhlbacher R, Hoser C (2006) Computer-assisted minimally invasive treatment of osteochondrosis dissecans of the talus. Oper Orthop Traumatol 18:300–316
Lee CK, Mercurio C (1981) Operative treatment of osteochondritis dissecans in situ by retrograde drilling and cancellous bone graft: a preliminary report. Clin Orthop Relat Res 158:129–136
Taranow WS, Bisignani GA, Towers JD, Conti SF (1999) Retrograde drilling of osteochondral lesions of the medial talar dome. Foot Ankle Int 20:474–480
Takao M, Innami K, Komatsu F, Matsushita T (2010) Retrograde cancellous bone plug transplantation for the treatment of advanced osteochondral lesions with large subchondral lesions of the ankle. Am J Sports Med 38:1653–1660
Ettl V, Kenn W, Radke S, Kirschner S, Goerttler-Krauspe I, Vispo-Seara JL (2001) The role of MRI in therapy and follow-up after surgical treatment of osteochondrosis dissecans of the talus. Z Orthop Ihre Grenzgeb 139:157–162
Radke S, Vispo-Seara J, Walther M, Kenn W, Kirschner S, Ettl V, Eulert J (2004) Osteochondral lesions of the talus—indications for MRI with a contrast agent. Z Orthop Ihre Grenzgeb 142:618–624
Kumai T, Takakura Y, Higashiyama I, Tamai S (1999) Arthroscopic drilling for the treatment of osteochondral lesions of the talus. J Bone Joint Surg Am 81:1229–1235
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anders, S., Lechler, P., Rackl, W. et al. Fluoroscopy-guided retrograde core drilling and cancellous bone grafting in osteochondral defects of the talus. International Orthopaedics (SICOT) 36, 1635–1640 (2012). https://doi.org/10.1007/s00264-012-1530-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1530-9