Abstract
Purpose
Venous thromboembolism (VTE) is a common complication of orthopaedic surgery in the industrialised world; though there may be variability between population groups. This study aims to define the incidence and risk factors for symptomatic VTE following primary elective total hip and knee arthoplasty surgery in a single centre in Eastern Europe.
Methods
This prospective study included 499 adult patients undergoing total hip and knee arthroplasty for symptomatic osteoarthritis over a two-year period at the Clinic of Orthopaedic Surgery and Traumatology, Belgrade.
Results
The overall rate of confirmed symptomatic VTE during hospitalisation was 2.6%. According to the univariate logistic regression, an age greater than 75 years (OR = 3.08; 95%CI = 1.01–9.65), a family history of VTE (OR = 6.61; 95% CI = 1.33–32.90), varicose veins (OR = 3.13; 95% CI = 1.03–9.48), and ischemic heart disease (OR = 4.93; 95% CI = 1.61–15.09) were significant risk factors for in-hospital VTE. A family history of VTE and ischemic heart disease were independent risk factors according to multivariate regression analysis. Preoperative initiation of pharmacological thromboprophylaxis (p = 0.03) and a longer duration of thromboprophylaxis (p = 0.001) were protective for postoperative DVT. Though thromboprophylaxis was safe, with very few patients suffering major haemorrhage or heparin-induced thrombocytopenia, there was a general reluctance by our local surgeons to use prolonged thromboprophylaxis.
Conclusion
VTE is common following hip and knee arthroplasty surgery. Orthopaedic patients with a family history of VTE, heart failure and coronary heart disease are at a considerable risk of thromboembolic complications in the postoperative period. There may be a role for preoperative thromboprophylaxis in addition to prolonged postoperative treatment.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Venous thromboembolism (VTE) is an important cause of mortality and morbidity. The incidence of VTE in the general population is about one to five per 1000, but in the surgical population it is more than 50% in the absence of thromboprophylaxis. Despite improved medical management, the high incidence of thromboembolic complications has remained fairly static over the last 30 years [1, 2].
VTE, including both deep-vein thrombosis (DVT) and/or pulmonary thromboembolism (PE), is one of the most serious complications of major orthopaedic surgery. It is estimated that operations of hip and knee arthroplasty are in the highest risk categories for venous thromboembolic complications. About 40–60% of patients undergoing major orthopaedic surgery of the hip and knee develop DVT and 4–10% of patients without prophylaxis develop PE [3–5]. Most cases of symptomatic VTE present following discharge from hospital and often result in hospital readmissions [5], although VTE can often be asymptomatic and the first signs of a PE can be sudden death. With this in mind many surgeons now administer prolonged thromboprophylaxis, and there have been significant advances in the use of regional anaesthetic techniques and oral pharmacological anticoagulants [6–10].
VTE incidence and risk factors have already been identified in the industrialised world, though there may be variability between different population groups [11]. This study aims to assess the incidence and risk factors for symptomatic VTE following primary elective total hip and knee arthoplasty surgery in a single centre in Eastern Europe.
Patients and methods
This prospective study was carried out at the Clinic of Orthopaedic Surgery and Traumatology, Clinical Centre of Serbia, Belgrade, between January 2008 and January 2010. This teaching hospital has a catchment population of approximately 1.5 million people. All adult patients undergoing hip and knee replacement surgery for symptomatic osteoarthritis were included. Hip fracture, polytrauma and revision arthroplasty patients were excluded from the study. DVT was confirmed by ultrasonography and PE by pulmonary scintigraphy. Clinically significant bleeding was defined as fatal bleeding, bleeding leading to re-operation or bleeding leading to blood transfusion. Routine screening for postoperative VTE was not performed.
The following data were collected on standardised pre-coded forms: patients’ demographic characteristics, comorbidities, thromboembolic risk factors, thromboprophylaxis regimes, surgical data (type of prosthesis, physical status defined as a score by the American Society of Anesthesiologists—ASA), anaesthesia techniques and postoperative complications.
Study outcomes
The primary outcome was the incidence of a confirmed symptomatic VTE event defined as DVT, fatal or non-fatal PE, or both, during hospitalisation. Other study outcomes were overall mortality, the incidence of any clinically significant bleeding event or other complications, and the identification of predictors for symptomatic VTE in this patient population.
Statistical analysis
Continuous variables (age, length of stay, etc.) were summarised in terms of mean values with standard deviation and range as measures of variability. Categorical values were presented as absolute frequencies and percentages. Continuous and categorical variables were compared using Student’s t-test and the chi-square test to assess the relation between potential risk factors and the outcome of interest. Univariate analysis and multivariate analysis were carried out. Variables associated with categorical outcome (development of VTE) in the univariate analysis were introduced into stepwise forward multivariate logistic regression analysis, with an entry probability of 0.5 and a probability of removal of 0.1. Data were processed and analysed by SPSS version 10.
Formal approval of this study was granted by the Institutional Ethics Committee.
Results
Patients
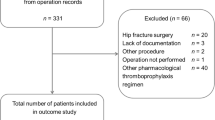
During the study period, 499 patients underwent elective total hip and knee arthoplasty surgery. Descriptive characteristics of surgical patients and thromboembolic risk factors are summarised in Table 1. The mean age of the population was 66.2 ± 9.5 years (range 30–90 years), with 61.1% greater than 65 years of age. Knee surgery patients were significantly older than hip surgery patients (p = 0.002). There were more women (68.1 %) than men in both groups, but the differences were not statistically significant (p > 0.05). The most frequent risk factor for VTE was varicose veins occurring in 139 (27.9%) patients, while 3% of affected patients had a family history of VTE and post-thrombotic syndrome. Other thromboembolic risk factors such as active cancer, thrombocytosis, acute infection and chronic obstructive pulmonary disease were seen only in low numbers of affected patients. Diabetes mellitus, heart failure, ischemic heart disease and dehydration were found in 11–24% of patients. There were no significant differences in any of these variables between patients undergoing hip and knee arthoplasty. None of the patients had active chemotherapy, myeloproliferative disorders, thrombophilia, polycythemia rubra verae or nephrotic syndrome. Moderate and severe renal impairment (creatinine clearance 30–50 ml/min, or <30 ml/min) were found in 35 (7.0%) patients.
Surgery characteristics
A total of 392 patients (78.6%) underwent total hip replacement surgery. Approximately 40% of patients had a poor physical status, defined as an ASA score of three or greater (Table 2). Surgery was performed under regional anaesthesia in 162 (32.5%) patients, and more frequently in knee surgery patients (p < 0.001). Surgical time was less than two hours in 80.6% of patients. However, the mean surgical time in knee patients was 140.1 ± 30.2 minutes, significantly longer than hip patients (105.3 ± 22.1 min) (t-test = −13.25, df = 497, p < 0.001). Patients were discharged after a mean of 26.5 ± 16.4 days and knee patients were hospitalised for longer (t-test = −2.21, df = 497, p < 0.05). A large proportion of patients (21.2% hip patients and 29.9% knee patients) were in hospital for more than 30 days.
Thromboprophylaxis and treatments
In almost all patients the thromboprophylaxis used was low-molecular-weight heparin (LMWH) (98.8% cases) (Table 2). The mean duration of thromboprophylaxis was 18.5 ± 9.1 days, with 124 (23.4%) patients receiving treatment for more than 21 days. Graduated compression stockings were only worn by eight (1.6%) patients, due to resource constraints. There was no difference between knee and hip patients for the above data. A total of 105 (21.0%) patients were taking aspirin pre-surgery (predominantly for ischaemic heart disease); these patients were recommenced on aspirin following hospital discharge and received LMWH during their hospital stays. Antithrombotic agents were started 12 hours preoperatively in 132 (26.5%) patients (LMWH in 129 patients and unfractionated heparin in three patients) and more frequently in knee surgery patients (p <0.05).
Thromboembolic events and complications
The overall rate of confirmed symptomatic VTE during hospitalisation was 2.6%. The median onset of a VTE event was three days post surgery. Below-knee DVTs were twice as common as above-knee DVTs. The rates of symptomatic deep vein thrombosis and pulmonary embolism were 1.3% and 1.5% in hip replacement patients and 0.9% and 1.9% in knee replacement patients, respectively, with no significant differences between the groups (p >0.05) (Table 3).
Two knee replacement patients (0.4%) were readmitted during their first follow-up year, one for a joint infection and the second for another surgical reason.
Six of 499 (1.5%) arthroplasties died while in hospital; these were all hip replacement patients. Two died from congestive heart failure, one from acute renal failure, one from a cerebral haemorrhage, and one from a small bowel obstruction. One patient died on the first postoperative day from an acute pulmonary embolism (confirmed on post-mortem examination).
Risk factors for symptomatic venous thromboembolism
Several risk factors associated with symptomatic venous thromboembolism in the univariate logistic regression analysis are shown in Table 4. An age greater than 75 years, a family history of VTE, varicose veins, and ischemic heart disease were significant (p < 0.05) risk factors for symptomatic venous thromboembolism during patient hospitalisation (Table 4). Preoperative initiation of pharmacological thromboprophylaxis (odds ratio 0.29; 95% CI 0.09–0.89; p = 0.03) and a longer duration of thromboprophylaxis (odds ratio 0.84; 95% CI 0.75–0.93; p = 0.001) protected patients from DVT after surgery.
According to multivariate regression analysis, a family history of VTE (odds ratio 7.63; 95% CI 1.43–40.56; p = 0.02), and ischemic heart disease (odds ratio 5.24; 95% CI 1.67–16.38; p = 0.004) were independent risk factors for a VTE event following hip and knee arthroplasty, while a duration of thromboprophylaxis greater than 19 days (odds ratio 0.81; 95% CI 0.72–0.91; p = 0.01) was a protective factor.
Oestrogen-containing oral contraception and hormone-replacement therapy (HRT), both considered potential VTE risk factors, were not analysed, as these treatments are not widely used in our country and this data was not recorded.
Discussion
VTE has been traditionally regarded as a disease of the developed world and despite thromboprophylaxis the rates of VTE in hip and knee arthroplasty patients both inpatient and post-discharge remains between 1% and 3% [12–17]; and very high levels of VTE have been seen in Asian patients not receiving preventive therapy [18, 19]. This study is one of very few longitudinal studies of in-hospital VTE following hip and knee arthroplasty in a developing country, and we found VTE incidence rates of 2.6%.
Although not statistically significant, VTE incidence rates tended to be greater following knee arthroplasty surgery (2.8% versus 2.6% following hip arthroplasty surgery), as seen in other countries [12, 20], possibly relating to the use of a thigh tourniquet and the associated venous stasis, more extensive soft-tissue damage, the release of prothrombotic tissue factors and longer surgical times [21].
In our study, the most commonly used thromboprophylactic agents were LMWHs (in 98.8% cases), as in most other countries, except than the United States where vitamin K antagonists are most frequently used [22]. Other thromboprophylactic agents (unfractionated heparin and vitamin K antagonist) were used considerably less frequently in our study.
Our mean duration for thromboprophylaxis was 18.5 ± 9.1 days, with some patients (23%) receiving thromboprophylactics for more than 21 days; we found longer-duration thromboprophylaxis, greater than 19 days, to be a protective factor for VTE in both univariate and multivariate analyses. We also found that preoperative thromboprophylaxis was a significant factor protecting against thromboembolic complications (p < 0.05), with possible implications that all patients should also receive preoperative VTE prophylaxis.
Despite the American College of Chest Physicians (ACCP) [3] recommendations for the prolonged use of thromboprophylactics, longer courses of treatment are still not routine practice in many hospitals in Serbia, or indeed in many other countries [20, 21]. The explanations for this lie with an inadequate organisation of our primary healthcare services (for home visits and the administration of thromboprophylaxis for our discharged patients), the high cost of many of the thromboprophylactic agents, the fears of perioperative haemorrhage and heparin-induced thrombocytopenia (HIT), and a possible lack of sufficient awareness of our surgeons about the significantly high risks of thromboembolic complications (PE and DVT) in the post-hospitalisation period. Nevertheless, the mean duration of thromboprophylaxis observed in our patient cohort as well as in the recent FOTO Study (36.1 ± 9.8 days) and RIETE Registry (17 ± 9.6 days) indicate an increasing trend for prolonged thromboprophylaxis [17, 23].
Risks of haemorrhage and HIT have been claimed as reasons for not using thromboprophylaxis routinely [3]. The safety of thromboprophylaxis is reflected by the low levels of haemorrhage (1.5%) seen in our patients, where there was one fatal haemorrhage, and no patients required re-intervention. A similar frequency of haemorrhage was seen in other series [7, 24]. Two of our patients suffered HIT; however this did not cause any major long-term problem.
Univariate analysis indicated that an age greater than 75 years was a risk factor for VTE (p = 0.05), as previously reported [7, 24, 25]. Multivariate analysis revealed that a family history of VTE and coronary artery disease were independent factors for VTE. Our study supports the findings of Spyropoulus et al. [21], who demonstrated that a pre-index VTE diagnosis, involving a VTE history, was the strongest independent predictor of a postoperative thromboembolic event. Others have identified comorbid conditions as independent risk factors for VTE [20, 24]. Considering the burden of these diseases within the older population, it is not surprising that among all comorbidities, cardiovascular diseases present the most significant risk for VTE. However, in contrast to our results, some investigators have reported that coronary artery disease is a poor predictor of VTE, or can even diminish the risk of VTE [9, 11], possibly due to general better health in the populations of these countries or stricter criteria for monitoring and treatment of cardiovascular diseases, including earlier aggregation therapy.
The limitations of our study are the relatively small number of patients with follow-up only during the hospitalisation period. VTE risks are known to persist beyond 11 days in elective hip replacement surgery, and fatal pulmonary embolism can still occur up to 49 days postoperatively [25]. Most of our patients went to rehabilitation centres, whereby the time to discharge was often dependent on the capacity of the facility; hence our postoperative hospital stay is longer than many Western countries. However, as our patients were generally in hospital for much longer periods, and receiving VTE prophylaxis, we consider that the number of post-discharge VTEs might not be great. This is supported by the fact that there were only two readmissions of our operated patients, and none for VTE.
Conclusion
Based on our findings, VTE is common following hip and knee arthroplasty surgery. Patients with a family history of VTE, heart failure and coronary heart disease are at a considerable risk of thromboembolic complications in the postoperative period. VTE thromboprophylaxis is safe and significant clinical bleeding and heparin-induced thrombocytopenia were rare. There may be a role for preoperative thromboprophylaxis in addition to prolonged postoperative treatment.
References
Heit JA (2008) The epidemiology of venous thromboembolism in the community. Arterioscler Thromb Vasc Biol 28:370–372
Fisher WD (2011) Impact of venous thromboembolism on clinical management and therapy after hip and knee arthroplasty. Can J Surg 54:344–351
Geerts WH, Bergquist D, Pineo G, Heit JA, Samama CM, Lassen MR et al (2008) Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 133(6 Suppl):381S–453S
Deitelzweig SB, McKean SC, Amin AN, Brotman DJ, Jaffer AK, Spyropoulos AC (2008) Prevention of venous thromboembolism in the orthopedic surgery patient. Cleve Clin J Med 75(3):S27–S36
Eriksson IB, Kakkar KA, Turpie GA, Gent M, Bandel TJ, Homering M et al (2009) Oral rivaroxaban for the prevention of symptomatic venous thromboembolism after elective hip and knee replacement. J Bone Joint Surg 91-B:636–644
Barrellier MT, Lebel B, Parienti JJ, Mismetti P, Dutheil JJ, Vielpeau C et al (2010) Short versus extended thromboprophylaxis after total knee arthroplasty: a randomized comparison. Thromb Res 6:e298–e304
Sugano N, Miki H, Nakamura N, Aihara M, Yamamoto K, Ohzono K (2009) Clinical efficacy of mechanical thromboprophylaxis without anticoagulant drugs for elective hip surgery in an Asian population. J Arthroplasty 24:1254–1257
Eikelboom JW, Quinlan DJ, Douketis JD (2001) Extended-duration prophylaxis against venous thromboembolism after total hip or knee replacement: a meta-analysis of the randomized trials. Lancet 358:9–15
Memtsoudis GS, Besculides CM, Gaber L, Liu S, Gonzales Della Valle A (2009) Risk factors for pulmonary embolism after hip and knee arthroplasty: a population-based study. Int Orthop (SICOT) 33:1739–1745
O’Donnell M, Linkins L-A, Kearon C, Julian J, Hirsh J (2003) Reduction of out-of-hospital symptomatic venous thromboembolism by extended thromboprophylaxis with low-molecular-weight heparin following elective hip arthroplasty. A systematic review. Arch Intern Med 163:1362–1366
Warvick D, Friedman RJ, Agnelli G, Gil-Garay E, Johnson K, FitzGerald G et al (2007) Insufficient duration of venous thromboembolism prophylaxis after total hip or knee replacment when compared with the time course of thromboembolic events. J Bone Joint Surg Br 89-B:799–807
Samama CM, Vray M, Barre J, Fiessinger JN, Rosencher N, Lecompte T et al (2002) Extended venous thromboemblism prophylaxis after total hip replacement: a comparison of low- molecular-weight heparin with oral anticoagulant. Arch Intern Med 162:2191–2196
Mauermann WJ, Shilling AM, Zuo Z (2006) A comparison of neuroaxial block versus general anesthesia for elective total hip replacement: a meta analysis. Anesth Analg 103:1018–1025
Macfarlane AJR, Prasad GA, Chan VWS, Brull R (2009) Does regional anaesthesia improve outcome after total hip arthroplasty? A systematic review. Br J Anaesth 103:335–345
Kakkar AK, Brenner B, Dahl OE, Eriksson BI, Mouret P, Muntz J et al (2008) Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: a doubleblind, randomised controlled trial. Lancet 372:29–37
Fuji T, Fujita S, Takahiro Ochi T (2008) Fondaparinux prevents venous thromboembolism after joint replacement surgery in Japanese patients. Int Orthop 32:443–451
Samama CM, Ravaud P, Parent F, Barre J, Mertl P, Mismetti P (2007) Epidemiology of venous thromboembolism after lower limb arthroplasty: the FOTO study. J Thromb Haemost 5:2360–2367
Anderson FA Jr, Hirsh J, White K, Fitzgerald RH Jr, Hip and Knee Registry Investigators (2003) Temporal trends in prevention of venous thromboembolism following primary total hip or knee arthroplasty 1996-2001: findings from the Hip and Knee Registry. Chest 124(6 Suppl):349–356
Sen RK, Kumar A, Tripathy SK, Aggarwal S, Khandelwal N, Manoharan SR (2011) Risk of postoperative venous thromboembolism in Indian patients sustaining pelvi-acetabular injury. Int Orthop 35:1057–1063
Friedman RJ, Gallus AS, Cushner FD, FitzGerald G, Anderson FA Jr; Global Orthopaedic Registry Investigators (2008) Physician compliance with guidelines for deep-vein thrombosis prevention in total hip and knee arthroplasty. Curr Med Res Opin 24:87–97
Spyropoulos AC, Hussein M, Lin J, Battleman D (2009) Rates of symptomatic venous thromboembolism in US surgical patients: a retrospective administrative database study. J Thromb Thrombolysis 28:458–464
Mantilla CB, Horlocker TT, Schroeder DR, Berry DJ, Brown DL (2003) Risk factors for clinically relevant pulmonary embolism and deep venous thrombosis in patients undergoing primary hip or knee arthroplasty. Anesthesiology 99:552–560
Arcelus JI, Monreal M, Caprini JA, Guisado G, Jose Soto M, Nunez MJ et al (2008) Clinical presentation and time-course of postoperative venous thromboembolism: Results from the RIETE Registry. Thromb Haemost 99:46–551
White RH, Henderson MC (2002) Risk factors for venous thromboembolism after total hip or knee replacement surgery. Curr Opin Pulm Med 8:365–371
Eikelboom JW, Quinlan DJ, Douketis JD (2001) Extended-duration prophylaxis against venous thromboembolism after total hip or knee replacement: a meta-analysis of the randomized trials. Lancet 358:91–95
Acknowledgements
This work was supported by the Ministry of Science and Technological Development of Serbia, contract No. 175046, 2011–2014.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Markovic-Denic, L., Zivkovic, K., Lesic, A. et al. Risk factors and distribution of symptomatic venous thromboembolism in total hip and knee replacements: prospective study. International Orthopaedics (SICOT) 36, 1299–1305 (2012). https://doi.org/10.1007/s00264-011-1466-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-011-1466-5