Abstract
Purpose
We evaluated the usefulness of percutaneous reduction and leverage fixation using K-wires in children with radial neck fractures.
Materials and methods
Between 2006 and 2008, we evaluated 13 paediatric patients with radial neck fractures who had been observed for at least two years and underwent percutaneous reduction and leverage fixation using K-wires. We measured radial angulation and radial translation using preoperative, postoperative and final follow-up radiographs, and we clinically investigated range of motion and carrying angle according to Steele’s grading system.
Results
Excellent clinical results were achieved in 11 (84.6%) patients, good results in one (7.6%) and fair results in one (7.6%). There were no poor results. The patient in whom fair results were achieved also had an olecranon fracture, which was treated conservatively. Complications such as nonunion, infection, iatrogenic nerve injury and periarticular ossification were minimal. Radioulnar synostosis was absent between the radial neck fracture and the greenstick fracture of the olecranon. Growth arrest in the proximal radial epiphysis was also absent.
Conclusion
Percutaneous reduction and leverage fixation using K-wires in children with radial neck fractures is a recommended surgical treatment that can achieve recovery of normal radial angulation and elbow motion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radial neck fractures account for 5–10% of all paediatric fractures; they do not occur readily because the radial head and neck are protected by the surrounding soft tissue. The main mechanism of this injury is a fall onto an outstretched arm. In the extended elbow, the capitulum of the humerus applies a strong force to the proximal radius; in a fall, this force may result in a fracture that includes dislocation of the radial head. Appropriate treatment for radial neck fractures in children is controversial, but almost all fractures with slight radial neck angulation are managed conservatively, and severely angulated fractures (>60°) require closed reduction, open reduction or open reduction and internal fixation [1–5]. Open reduction can be used for anatomical fracture fixation but may compromise the vulnerable blood supply to the radial head. Other risks of this treatment include early physeal closure, abnormal radial head enlargement and periarticular ossification.
Although the Metaizeau method introduced in 1980 has achieved excellent results, it continues to be associated with problems, such as the risk of proximal physis injury, the difficulty of maintaining reduction and superficial radial nerve injury at the pin insertion site [1, 4, 6–10]. Since the introduction of the technique by Feray [11] in 1969, percutaneous reduction and leverage fixation techniques for radial head and neck fractures in children have been further developed by Angelov [12] and Pesudo et al. [13], but they are not used universally. We devised a modified percutaneous reduction and temporary leverage fixation method and report excellent results after a follow-up of least two years.
Materials and methods
Between 2006 and 2008, we evaluated 13 paediatric patients with radial neck fractures who had been observed for at least two years and underwent percutaneous reduction and leverage fixation using K-wires. All cases with >45° angulation that were seen within 12 hours of fracture were assessed. Cases with associated fractures in the elbow region that required invasive operation were excluded. Average patient age was 10.4 (range six to 13) years. Eight patients were boys and five were girls; the average follow-up period was 3.5 (range 2.4–4.4) years. The main mechanism of injury was a fall onto an extended arm. Nine patients sustained no additional injury, two presented with olecranon fractures and two presented with ulnar shaft fractures. All procedures were performed by a single surgeon (HDS). The injured elbow was screened using a high-resolution image intensifier with magnification facilities and a thermographic printer. Under general anaesthesia, radiographs were taken of the extended elbow in the anteroposterior (AP) plane through the range of forearm rotation. The position of maximum fracture angulation was then evaluated. The degree of angulation was defined as the angle of intersection of a line drawn perpendicular to the epiphyseal plate, with another line drawn along the midline of the radial diaphysis [14]. Due to the effect of rotation, this angle could rarely be measured on original radiographs. The degree of radial translation (displacement) was measured on the same images by dividing the width of the uncovered radial metaphysis by the total width of the metaphysis, then expressing the value as a percentage. Fractures were classified into the following grades in accordance with the method of Judet et al. [15], as modified by Metaizeau et al. [9, 10]: grade 1, nondisplacement with horizontal shift; grade 2, angle <30°; grade 3, angle of 30–60°; grade 4, angle >60° (4a: 60–80°, 4b: >80°). Four cases were classified as grade 3 (mean angle, 54°; range, 48–58°) and nine as grade 4a (mean angle, 71.1°; range, 64–78°). The growth plates of all patients were open. All operations were performed within 12 hours of injury. Percutaneous leverage fixation was possible in 12 cases; in one grade 4 (78° angulation) case, stabilisation was provided by leverage fixation using a K-wire and minimal arthrotomy. In this case, soft-tissue interposition hindered reduction during the operation, and despite all efforts, alignment with manual closed reduction was not achieved.
Surgical technique
A 1.4- or 1.6-mm K-wire was used depending on patient age. The K-wire was inserted percutaneously from proximal to distal at the radial neck fracture site, the outside part of the K-wire was pulled distally through the skin and the inner side of the K-wire was then inserted around the fracture site. In this procedure, care must be taken to avoid penetration of the K-wire into the fracture site. As in the Kapandji [16] technique for treating fractures of the distal radius, the inserted K-wire was used as a lever, the radial neck fracture was reduced and reduction was confirmed with an image intensifier. After reduction, the K-wire was advanced toward the ulnar side in the same distal direction of initial insertion to prevent complications due to skin buckling resulting from differences in the initial and final K-wire trajectories (Fig. 1). In two cases, an intra-articular arthrogram was performed to confirm the type of fracture. A long-arm splint was applied, with the forearm in a neutral position after the portion K-wire remaining outside the skin was cut. The splint was applied for four to six weeks, and the K-wire was then removed before the arm was exercised. The surgeon did not directly manipulate the fracture segment for reduction or use an additional K-wire for percutaneous temporary manipulation.
Surgical technique developed by the authors. a Under general anaesthesia, we evaluated the maximal angulation and translation of the radial neck before K-wire leverage fixation. The surgeon did not directly manipulate the fracture segment for reduction or use an additional K-wire for percutaneous temporary manipulation. b The K-wire tip was positioned carefully to touch the site of the fractured radial neck. c Using the inserted K-wire as a lever, the radial neck fracture was reduced, and reduction was confirmed with an image intensifier. Care was taken to prevent penetration of the fracture site. d After reduction, the K-wire was advanced towards the ulnar side in the distal direction of initial insertion
Postoperative evaluation
Patients were reviewed at one and three months and then at six month intervals. Angulation and translation were measured postoperatively and at the final follow-up evaluation using the same methods employed preoperatively. The degree of deficits in the maximum ranges of elbow flexion and extension and forearm pronation and supination were assessed at the final follow-up examination. The degree of increased carrying angle was also evaluated at the final follow-up examination by comparison with the contralateral limb. Deformity of the radial head was assessed by comparing the diameter of the head to that of the distal humeral condyle in an AP radiograph at the final follow-up examination [5]. A ratio of less than two was regarded as overgrowth of the radial head (Fig. 2). Clinical results were scored using the grading system of Steele et al. [17] (Table 1).
Results
As measured radiographically, the average angulation of the radial head was 65.8° preoperatively, 4.69° postoperatively and 7.1° at the final follow-up examination. The deficits in the range of flexion, extension, pronation and supination were 0–10°, 0–5°, 0–15°, and 0–10°, respectively. The carrying angle of the elbow was symmetrical in 77% (10/13 cases) of patients (Fig. 3). At the final follow-up examination, the carrying angle had increased in two patients compared to the contralateral limb. Carrying angle could not be evaluated in one patient due to a deficit of extension. Deformity of the radial head was observed in one case, but the radiological deformity did not correlate with clinical results.
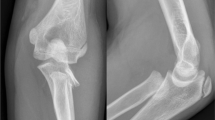
a, b A 6-year-old boy with a fracture characterised by 70° angulation and 80% displacement. c, d After K-wire fixation using a modified Kapandji [9] technique. e Radiographs showing 6° angulation after 38 months. Range of movement was not limited, and clinical results were excellent
According to the grading system of Steele et al. [17], excellent results were achieved by the time of final follow-up evaluation in 11 cases, good results in one and fair results in one. The case in which fair results were achieved was accompanied by an olecranon fracture that was treated conservatively. This patient had no complaint of functional, cosmetic or social impairment at the final follow-up examination (Table 2). Complications such as nonunion, infection, iatrogenic nerve injury and periarticular ossification were minimal. Radioulnar synostosis was absent between the radial neck fracture and the greenstick fracture of the olecranon. Growth arrest in the proximal radial epiphysis was also absent.
Discussion
Generally, radial neck fractures in children are treated with a posterior splint or long-arm cast with the elbow in a flexed position when the angulation is <30° at the time of injury or after manual reduction [5, 6, 18]. However, the appropriate treatment for radial neck fractures in children with angulations >30° is debated; the prognosis is related not only to radial neck angulation but also to patient age and the intensity of trauma [19]. Bernstein et al. [19] recommended conservative treatment of fractures with 60° radial head angulation in six-year-old patients and operative treatment in cases of radial head angulation >30° in 12-year-old patients. Steele et al. [17] developed the following classification using angulation and translation: grade I, 0–30° angulation, <10% translation; grade II, 31–60° angulation, 11–50% translation; grade III, 61–90° angulation, 51–90% translation; grade IV, >90° angulation, >90% translation. They reported satisfactory results with the use of pain control and application of a simple splint for seven to ten days in grade I cases, manual reduction or percutaneous leverage fixation in grade II and III cases and open reduction and internal fixation in grade IV cases. Using a similar method, Steinberg et al. [20] reported that angulation and translation of the radial head are helpful measures in treatment planning for radial head fractures in children.
Operative treatments of radial neck fractures in children may be closed (noninvasive) or open (invasive); the definitive indication for noninvasive treatment is controversial. Although in the past, open reduction was commonly used, its use is now restricted to comminuted fractures and cases of closed reduction failure. Open reduction is associated with extremely serious risks, such as early physeal closure, abnormal radial head enlargement and periarticular ossification. Because blood flow to the radial head can be damaged during trauma, further damage and avascular necrosis during open reduction are highly likely [10, 19–21]. This method may also result in unsatisfactory reduction or a compromised prognosis due to the surgeon’s technique.
In our study, only one grade 4a case exhibited alignment incompatible with a percutaneous reduction and leverage fixation using a K-wire. In this case, open reduction was performed with minimal arthrotomy; during this procedure, soft-tissue interposition that hindered reduction was detected. Stabilisation was achieved with a K-wire after the reduction, and no periarticular ossification developed.
Noninvasive operative treatments using percutaneous reduction techniques have been reported widely and may be divided into three categories. The first method is reduction by the direct application of pressure to the proximal fragment using a Steinmann pin or a periosteal elevator after percutaneous or mini open reduction. This method must be performed carefully due to the high risk of injury to the deep branch of the radial nerve. After reduction, the arm is fixed in a flexed (90°) position for three to six weeks. The second method is similar to the first, but a thinner K-wire is used to penetrate the fracture line, and the operator then elevates and reduces the radial head, removes the K-wire and applies a long-arm splint [17]. The third method, designed by Metaizeau [8–10, 22], involves the insertion of a specially designed long wire into the marrow cavity of the radius and then towards the radial head for reduction. The elbow is then immobilised for two to three weeks, and the wire is removed after eight weeks. This method must also be performed carefully to avoid injury to the sensory branch of the radial nerve and the physis.
The technique used in our study was similar to the second method described above. However, in our method, the radial head was elevated directly using a K-wire, as in the Kapandji [16] technique for distal radius fractures, while avoiding penetration of the fracture line by the K-wire to prevent epiphyseal injury. Our initial fixation of the K-wire and insertion of the pin from proximal to distal prevented the K-wire from buckling the skin and causing potential complications. In techniques that penetrate the fracture line, cubitus valgus or nonunion frequently develops due to epiphyseal injury. In our study, cubitus valgus or nonunion occurred less frequently than expected because our technique did not result in direct injury to the epiphyseal plate. However, the indication for such treatment of radial neck fractures is limited in cases of excessive radial neck angulation, severe translation and/or comminution of the radial head or neck. All cases in our study were reducible comminuted fractures of grade 3 or higher [9, 10, 15] radial neck angulation, which we treated using a noninvasive operative technique.
We would like to call particular attention to further damage to physis blood flow, which is already damaged slightly by the original trauma, as a result of forceful traction or manipulation. In our study, initial manual manipulation was extremely limited, and the surgeon never used an additional percutaneous K-wire for temporary reduction of the proximal fracture segment. The surgeon used only one K-wire and was careful not to penetrate the fracture line.
Conclusion
In children with severely displaced radial neck fractures requiring operative treatment, the percutaneous K-wire fixation and leverage technique described here is recommended for satisfactory restoration of radial neck alignment and range of motion and the minimisation of complications such as nonunion, infection, iatrogenic nerve injury, periarticular ossification and growth arrest in the proximal radial epiphysis.
References
Eberl R, Singer G, Fruhmann J, Saxena A, Hoellwarth ME (2010) Intramedullary nailing for the treatment of dislocated pediatric radial neck fractures. Eur J Pediatr Surg 20(4):250–252. doi:10.1055/s-0030-1249104
Kaufman B, Rinott MG, Tanzman M (1989) Closed reduction of fractures of the proximal radius in children. J Bone Joint Surg 71B:66–67
Tollet P, Toussaint D, Djemal C, Louvard A, Bremen J (1997) Surgical treatment of fractures of the radius neck in children using the Metaizeau technique. Acta Orthop Belg 63:245–249
Ugutmen E, Ozkan K, Ozkan FU, Eceviz E, Altintas F, Unay K (2010) Reduction and fixation of radius neck fractures in children with intramedullary pin. J Pediatr Orthop B 19(4):289–293. doi:10.1097/BPB.0b013e32833918a0
Vocke AK, Von Laer L (1998) Displaced fractures of the radial neck in children: long-term results and prognosis of conservative treatment. J Pediatr Orthop B 7(3):217–222
Green NE (1994) Fractures and dislocations about the elbow. In: Green NE, Swiontkowski MF (eds) Skeletal trauma in children. WB Saunders, Philadelphia, pp 213–256
Klitscher D, Richter S, Bodenschatz K, Hückstädt T, Weltzien A, Müller LP et al (2009) Evaluation of severely displaced radial neck fractures in children treated with elastic stable intramedullary nailing. J Pediatr Orthop 29:698–703. doi:10.1097/BPO.0b013e3181b76895
Metaizeau JP (2005) Reduction and osteosynthesis of radial neck fractures in children by centromedullary pinning. Injury 36(Suppl 1):A75–A77. doi:10.1016/j.injury.2004.12.016
Metaizeau JP, Lascombes P, Lemelle JL, Finlayson D, Prevot J (1993) Reduction and fixation of displaced radial neck fractures by closed intramedullary pinning. J Pediatr Orthop 13:355–360
Metaizeau JP, Prevot J, Schmitt M (1980) Reduction and fixation of fractures of the neck of the radius by centro-medullary pinning. Original technique. Rev Chir Orthop 66:47–49
Feray C (1969) Original method of bloodless reduction of severe fractures of the head of the radius in children. Presse Med 77(56):2155–2156
Angelov A (1981) A new method for treatment of the dislocated radial neck fractures in children. In: Chapchal G (ed) 9th international symposium on topical problems in orthopaedics surgery, Lausanne. Georg Thieme Verlag, Stuttgart, Germany, pp 192–194
Pesudo JV, Aracil J, Barcelo M (1982) Leverage method in displaced fractures of the radial neck in children. Clin Orthop 169:215–218
O’Brien PI, Menelaus MB (1965) Injuries involving the radial epiphysis. Clin Orthop 41:51–58
Judet J, Judet R, Lefranc J (1962) Fracture of the radial head in the child. Ann Chir 16:1377–1385
Kapandji A (1987) Intra-focal pinning of fractures of the distal end of the radius 10 years later. Ann Chir Main 6:57–63
Steele JA, Graham HK (1992) Angulated radial neck fractures in children. A prospective study of percutaneous reduction. J Bone Joint Surg 74B:760–764
Jones ERL, Esah M (1971) Displaced fractures of the neck of the radius in children. J Bone Joint Surg 53B:429–439
Bernstein SM, McKeever P, Bernstein L (1993) Percutaneous reduction of displaced radial neck fractures in children. J Pediatr Orthop 13:85–88
Steinberg EL, Golomb D, Salama R, Weintroub S (1988) Radial head and neck fractures in children. J Pediatr Orthop 8:35–40
Schmittenbecher PP, Haevernick B, Herold A, Knorr P, Schmid E (2005) Treatment decision, method of osteosynthesis and outcome in radial neck fractures in children. A multicentric study. J Pediatr Orthop 25:45–50
González-Herranz P, Alvarez-Romera A, Burgos J, Rapariz JM, Hevia E (1997) Displaced radial neck fractures in children treated by closed intramedullary pinning (Metaizeau technique). J Pediatr Orthop 17(3):325–331
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cha, S.M., Shin, H.D., Kim, K.C. et al. Percutaneous reduction and leverage fixation using K-wires in paediatric angulated radial neck fractures. International Orthopaedics (SICOT) 36, 803–809 (2012). https://doi.org/10.1007/s00264-011-1387-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-011-1387-3