Abstract
Purpose
The purpose of this prospective non-randomised study was to compare the efficacy of two opposed methods, operative and conservative. Our hypothesis was that if the method was selected correctly, on an individual basis, the results should be approximately equal.
Methods
The study included 37 adolescents aged between 12 and 16 years, with a mean follow up of 6.1 years. The presence of a significant loose body, confirmed by precise imaging, was the key for selecting operative or arthroscopic treatment. In both groups of patients, we evaluated functional knee scores and the incidence of residual patellofemoral disorders.
Results
We confirmed our hypothesis using the t-test to compare functional results and a test for comparison of proportions for incidence of residual disorders. There was no statistically significant difference (p=0.091) between operatively and conservatively treated groups with regard to functional results. The same statistical outcome emerged when comparing incidences of re-dislocation (p=0.854), or other major patellar instabilities (p=0.856), between the groups.
Conclusions
The results obtained should not promote a non-operative method on the basis of lower risk, but do support an individual approach based on precise diagnosis and defined criteria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute patellar dislocation accounts for 2–3% of acute knee injuries, with the highest incidence being in adolescence [1, 2]. Apart from the traumatic component, the presence of predisposing morphological and functional patellofemoral disorders [3, 4] is of equal importance. The two aetiological conditions are represented in various, but complementary, relations: dominant predisposing factors need less trauma for dislocation, and vice versa. The nonoperative approach was widely accepted and commonly applied in acute patellar dislocation treatment until the end of the twentieth century. However, a high incidence of residual patellar instability, anterior knee pain, and redislocation of up to 44% in the representative studies [5–7], combined with advances in and a proper understanding of functional anatomy and biomechanics of the medial patellar stabilisers [8, 9], led to expansion of primary surgical treatment for acute patellar dislocation [10]. Surgery is mainly based on immediate medial repair and proximal realignment procedures. Various surgical modalities have been reported, beginning with open [11, 12], through minimally invasive and arthroscopically assisted [13, 14], to fully arthroscopic [15–17] procedures. Traumatic patellar dislocation causes a high incidence of injuries to the medial patellofemoral ligament (MPFL) [18], the structure recognised as the most important soft tissue, passive restraint to lateral patellar dislocation, especially in the first 30° of knee flexion [19]. Therefore, primary surgery to the medial parapatellar aspect is focused on reconstructing the MPFL and surrounding soft tissues. On the other hand, the tendency towards immediate lateral retinacular release (LRR) [20] in the aforementioned studies is controversial: from “never” [21], through “in selected cases” [10, 11, 22], to “always” [12–14].
Obligatory surgical treatment of acute patellar dislocation was questioned in a retrospective analysis by Buchner et al. [23], as well as in prospective randomised studies on samples of various sizes and structures by Nikku et al. and Palmu et al. [20, 24].
The aim of our prospective, nonrandomised study was to compare the results of operative and nonoperative methods in the primary treatment of acute patellar dislocation in adolescents. As the method of treatment was adjusted for each individual, with the primary goal of achieving the best possible results with respect to residual disorders and function of the patellofemoral joint, our hypothesis was that if the method was selected correctly, there should only be minor differences in results of the two methods. Results are presented as functional knee scores at the end of initial treatment and the incidence of residual patellofemoral disorders to the end of adolescence. Clinical findings and precise imaging methods were the basis for establishing diagnosis and choosing the appropriate method of treatment.
Materials and methods
This prospective study involved 37 patients with unilateral dislocation, 28 girls and nine boys, treated between 1995 and 2004. Follow-up ranged from five to eight years (mean 6.1), being the time to complete the adolescent period. Mean age at the beginning was 13.8 (12–16) years. We used the following inclusive selection criteria:
-
1.
Presence of locked acute dislocation or history of reduced dislocation within a week of the injury.
-
2.
Typical clinical findings: haemarthrosis, medial parapatellar structures and femoral epicondyle painful on palpation, apprehension sign (except in locked dislocation).
-
3.
Positive magnetic resonance imaging (MRI) findings: effusion, medial retinacular injury, osteochondral lesion, loose body (eventually).
-
4.
Adolescent age at the time of injury.
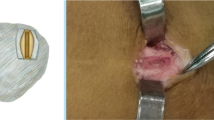
Patients with a history of previous patellofemoral disorder, serious injury, and/or surgery on the affected knee or ipsilateral leg were excluded. Initial treatment was either conservative or surgical. The criterion for surgical treatment was significant intra-articular loose body (≥8 mm diameter) diagnosed by standard X-ray and MRI (Fig. 1). Nonoperative treatment (mean three weeks) included closed reduction of dislocated patella, immobilisation, local cold packs during first 24 hours following injury, and, eventually, aspiration of effusion. As the pain subsided, isometric quadriceps exercises were initiated.
Immediate surgical treatment of acute patellar dislocation was performed within ten days of the injury. All patients underwent arthroscopic surgery, which, as a standard procedure, included effusion elimination, haemostasis, and loose-body removal if there was no possibility of refixation. Further arthroscopic surgical procedures were selected and correlated individually to meet the requirements of each patient in accordance with the extent of damage to medial structures (defined by MRI and arthroscopic findings), mediolateral patellar mobility, patellofemoral alignment, and other relevant factors that affect patellar stability. In 12 of 14 operated knees (86%), we performed medial retinacular and capsular repair using a modified Yamamoto technique [13]. Immediate lateral retinacular release [20] was performed if arthroscopic evaluation of dynamic patellofemoral alignment showed lateral patellar tilt. Nine patients (64%) underwent arthroscopic LRR by means of an electroresector. In two cases, the procedure was sufficient, without medial repair. We used the Cincinnati Knee Rating System [25] for functional assessment. The System is based on estimation of six abilities that are important for participation in sports but is also applicable for everyday highly demanding activities of the adolescent population. Maximal score in this system is 420, and the result was considered successful for the score >80%. Functional assessment took place after the initial treatment and consecutive rehabilitation, usually eight to ten months after injury. Further follow up, performed annually, included history of patellofemoral disorders, including redislocations and physical and X-ray examination. After completing the initial treatment, during follow-up, patients who sustained patellar redislocation or had significant, unrelenting patellar instability, underwent obligatory surgery: distal realignment was performed in all such cases, and proximal realignment was repeated in three.
Student’s t test was used to compare functional results of operatively treated patients with the results of patients in the nonoperative group, and to compare successfully and unsuccessfully treated subgroups. Correlative comparison of the incidence of redislocation and residual patellar instability between operated and nonoperated patients was evaluated using the chi-square test for comparison.
Results
Of 37 patients who sustained acute patellar dislocation, 23 were initially treated nonoperatively and 14 surgically. Results of functional assessment are presented in Table 1. Based on the results of the Cincinnati Knee Rating System, we successfully treated 29 patients (78.38%), 20 of them nonoperatively and nine operatively.
Comparison of the results of all nonoperatively treated patients (group A) to the results of all operatively treated patients (group B) showed there was no statistically significant difference (t = 1.73708; df = 35; p = 0.091167). Mutual comparison of the results of successfully treated patients (subgroups A1 and B1), showed there was no statistically significant difference between subgroups (A1:B1 t = 0.0268; df = 17; p = 0.9788). During the follow-up, mild symptoms of patellofemoral malalignment were reported by four patients: three complained of occasional anterior knee pain (one had pain combined with patellar subluxation), and the fourth had several episodes of painless patellar subluxation. The patient with combined symptoms was initially treated operatively and the other three nonoperatively. The test for comparison of proportions showed that there was no statistically significant difference between operatively and conservatively treated patients with respect to mild patellofemoral symptoms (Table 2). None of those four patients required delayed surgical treatment.
T test showed there was no statistically significant difference between nonoperated and operated patients with poor functional results (subgroups A2 and B2, respectively): t = 0.4726; df = 6; p = 0.6531. Eight patients had poor functional results, and they all underwent delayed surgical treatment. Three of them had patella redislocation between one and three years after the initial treatment. One patient was initially treated nonoperatively (7.14%) and the other two were operated upon (8.69%). There was no statistically significant difference between nonoperated and operated patients in the incidence of redislocation (Table 2). The remaining five patients with poor functional results underwent delayed surgery because they developed significant patellar instability with no signs of improvement. Initially, two of them were treated surgically, and three were treated nonoperatively. The incidence of major patellar instability showed no statistically significant difference between primary surgical treatment and nonoperated patients (Table 2). In eight patients who underwent additional surgery, four (20.18%) were initially treated nonoperatively and the other four (22.97%) operatively after the acute patellar dislocation. Finally, after the initial treatment of acute patellar dislocation in 37 adolescents, twelve of them (32.43%) developed a kind of patellofemoral disorder.
Discussion
Immediate diagnostic arthroscopy and surgery for osteochondral injury as a method of choice in the initial acute patellar dislocation treatment is not questioned in the majority of comparative studies. However, various authors regard the procedure differently. Buchner et al. [23], in their retrospective study, separate patients who underwent diagnostic arthroscopy and refixation of the osteochondral fragment into a special group from conservatively and surgically treated patients. Sillanpaa et al. [14] add those patients to a group of nonoperatively treated patients, whereas the authors of randomised studies, Nikku et al. [24], Palmu et al. [22], and Christiansen et al. [21], regard the procedure as diagnostic and therapeutic, which is mandatory prior to final selection of operative or nonoperative treatment. In our study, diagnostic arthroscopy with simultaneous management of the essential osteochondral fragment was regarded as an operative treatment that could accompany repair of medial parapatellar structures and/or lateral retinacular release, if necessary.
Review of the aforementioned comparative studies showed equal results when comparing of redislocation incidence and functional results between surgically and nonsurgically treated patients. However, significant difference between studies occurred in total number of patellar dislocations, whereas results of functional scores were similar, ranking >80% of maximum. Christiansen et al. reported 16.7% and 20% patellar redislocation after operative and nonoperative treatment, respectively. The average age of patients in their study (20 years) was older than adolescent, and surgical treatment was postponed some 50 days after injury. Sillanpaa et al. studied the population of the same average age but predominately men (military recruits) and reported a higher percentage of redislocation (19% and 23%, respectively). Nikku et al. reported 31% and 39% of redislocation over seven years of follow-up in a group of the same average age but with >60% of patients <16 years. Palmu et al., after 14 years of follow-up, reported a redislocation rate as high as 67% and 71%, respectively, in an adolescent population (average 13 years), with >52% within the first two years. It is interesting that such a high percentage of redislocation occurred with a high incidence of very good and excellent functional and subjective results. In our study, the rate of reported redislocation in operatively and nonoperatively treated patients was 7.1% and 8.7%, respectively. That rate was based on patient interpretation and impression reported during the follow-up period. However, we considered as more relevant the rate of all patients who had to be operated upon after the initial treatment, whether due to reported redislocation or major functional disorder of the patellofemoral joint. There were five of the latter in our study: three who underwent initial conservative treatment and two who were initially operated upon (Table 2). Therefore, we added the number of patients who underwent postponed surgery due to serious patellar instability and poor functional tests to those who reported redislocation during follow-up. Consequently, the percentage of serious recurrent patellofemoral disorders that needed postponed surgery rose to 20.18% in the group of primarily conservatively treated patients and to 22.97% in patients who initially underwent surgery. Nevertheless, requirements for postponed surgical treatment in this number of patients should be regarded as a phase in a step by step treatment of complicated cases rather than unsuccessful initial treatment.
This study showed equal results for the nonoperative and operative treatment of acute patellar dislocation in adolescents with respect to functional scores and incidence of serious patellofemoral disorders that required delayed and complex surgical treatment. Such results may implicate the nonoperative approach as a method of choice when treating primary acute patellar dislocation, as it is less invasive than surgical treatment and as equally efficient. However, such direct treatment comparison is inappropriate because different proportions between the most important aetiological factors, as well as individual growth rates during adolescence, did not allow balancing patients appropriately before choosing the initial treatment method. Rather, we suggest that both treatment methods, appropriately indicated and individually adjusted, showed similar results regarding functional scores and recurrent patellofemoral disorders.
Conclusion
Initial treatment of acute patellar dislocation should first effectively evaluate the direct consequences of the injury and second provide feasible immediate prevention of delayed ones, including redislocation. The method of choice should accomplish the fine balance between treatment extent and expected results. The results of our analysis, as well as those of some other nonrandomised studies, may be regarded as favouring nonoperative treatment due to equal results and lower risk in comparison with surgery. In our opinion, successful initial treatment of acute patellar dislocation in adolescents should not strictly follow any recommended, universal, pattern but try to create an individual approach based on precise diagnosis and defined criteria.
References
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, White LM (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32:1114–1121
Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelson C (2008) Characteristics of patients with primary acute lateral dislocation and their recovery within the first 6 months of injury. Am J Sports Med 28:472
Colvin AC, West RV (2008) Patellar instability. J Bone Joint Surg 90A:2751–2762
Bollier M, Fulkerson JP (2011) The Role of trochlear dysplasia in patellofemoral instability. J Am Acad Orthop Surg 19(1):8–16
Cofield RH, Bryan RS (1977) Acute dislocation of the patella: results of conservative treatment. J Trauma 17:526–531
Hawkins RJ, Bell RH, Anisette G (1986) Acute patellar dislocations. The natural history. Am J Sports Med 14(2):117–120
Maenpaa H, Lehlo MUK (1997) Patellar dislocation: the long-term results of non-operative treatment in 100 patients. Am J Sports Med 25:213–217
Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP (2003) Anatomy and biomechanics of the medial patellofemoral ligament. Knee 10(3):215–220
Feller JA, Amis AA, Andrish JT, Arendt EA, Erasmus PJ, Powers CM (2007) Surgical biomechanics of the patellofemoral joint. Arthroscopy 23(5):542–553
Arendt EA, Fithian DC, Cohen E (2002) Current concepts of lateral patella dislocation. Clin Sports Med 21(3):499–519
Vainionpaa S, Laasonen E, Silvennoinen T, Vasenius J, Rokkanen P (1990) Acute dislocation of the patella. A prospective review of operative treatment. J Bone Joint Surg 72B:366–369
Ahmad CS, Shubin Stein BE, Matuz D, Henry J (2000) Immediate surgical repair of the medial patellar stabilizers for acute patellar dislocation. Am J Sports Med 28(6):804–810
Yamamoto RK (1986) Arthroscopic repair of the medial retinaculum and capsule in acute patellar dislocations. Arthroscopy 2(2):125–131
Sillanpaa PJ, Maenpaa HM, Matilla VM, Visuri T, Pihlajamaki H (2008) Arthroscopic surgery for primary traumatic patellar dislocation: a prospective nonrandomized study comparing patients treated with and without acute arthroscopic stabilisation with a median 7 – year follow-up. Am J Sports Med 36(12):2301–2309
Ahmad CS, Lee FY (2001) An all-arthroscopic soft-tissue balancing technique for lateral patellar instability. Arthroscopy 17(5):555–557
Haspl M, Cicak N, Klobucar H, Pecina M (2002) Fully arthroscopic stabilization of the patella. Arthroscopy 18(1):E2
Mariani P.P., Liguori L., Cerullo G., Iannella G., Floris L. (2010). Arthroscopic patellar reinsertion of the MPFL in acute patellar dislocations. Knee Surg Sports Traumatol Arthrosc. Epub ahead of print
Nomura E (1999) Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop 23(5):260–263
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restriants to lateral patellar translation in human knee. Am J Sports Med 26:59–65
Clifton R, Ng CY, Nutton RW (2010) What is the role of lateral retinacular release? J Bone Joint Surg 92B:1–6
Christiansen SE, Jakobsen BW, Lund B, Lind M (2008) Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy 24(8):881–887
Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y (2008) Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg 90A(3):463–470
Buchner M, Baudendistel B, Sabo D, Schmitt H (2005) Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med 15(2):62–66
Nikku R, Nietosvaara Y, Aalto K, Kallio PE (2005) Operative treatment of primary patellar dislocation does not improve medium-term outcome: A 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop 76(5):699–704
Noyes FR, Barber SD, Mooar LA (1989) A rationale for assesing sports activity levels and limitations in knee disorders. Clin Orthop Relat Res 246:238–249
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Apostolovic, M., Vukomanovic, B., Slavkovic, N. et al. Acute patellar dislocation in adolescents: operative versus nonoperative treatment. International Orthopaedics (SICOT) 35, 1483–1487 (2011). https://doi.org/10.1007/s00264-011-1265-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-011-1265-z