Abstract
We report on a prospective series of 201 primary uncemented total hip arthroplasties with a Bicontact prosthesis at a mean follow-up of 12.9 years. The mean Harris hip score improved from 41 before surgery to 89 at final follow-up. Two femoral stems, one each for infection and fracture, and 12 cups were revised. The mean number of years to revision post-primary surgery was 8.7 years (six months to 16 years). The cumulative survival of the prosthesis was 95.42% for any cause at ten years and 93.57% at 12 years. Survivorship for aseptic loosening of the femoral stem was 100%. In our series, the Bicontact uncemented total hip arthroplasty stem without hydroxyapatite coating showed excellent survival and the cup survival was comparable to other leading series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The aim of the cementless hip components is to encourage biological fixation by allowing bone integration ensuring long survivorship of the prosthesis [1, 2]. The prosthesis allows preservation of bone metabolism and conserves bone, especially important in young patients with higher functional demands with longer life expectancy and also the young patients with rheumatoid arthritis [1, 2].
This bony integration requires the components to be highly stable and this is achieved as a function of the shape and surface geometry of the components, intimal fit and the load and stress transmission between the two [3]. The medium term results of the Bicontact total hip arthroplasty with a minimum follow-up of 6.5 years have been encouraging [4]. There are however concerns of osteolysis and loosening as a consequence of polyethylene particle wear [4–6] or early aseptic loosening due to reduced primary stability [1].
We report the long-term results of a clinical and radiological review of 177 patients (201 hips) who underwent a total hip arthroplasty using the Bicontact uncemented prosthesis.
Materials and methods
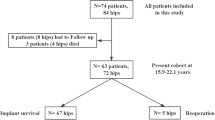
During the period between October 1991 and October 1997, 201 consecutive uncemented total hip arthroplasties using the Bicontact uncemented prosthesis (Aesculap, Tuttlingen, Germany) were performed in 177 patients; 126 of these patients were women and the procedures were carried out predominantly on the left side. Fifteen patients had bilateral arthroplasty but at different intervals. All operations were performed by one senior surgeon or a senior trainee supervised by him. The mean age at operation was 66.6 years (range 39–88 years). Of these patients, 17 were lost to follow-up (8.5%) and 62 (30.8%) patients died of unrelated causes in the follow-up period. Thus, 122 total hip arthroplasties in 98 patients were available for both clinical and radiological review beyond ten years. The mean final follow-up period was 12.9 years (range 10.1–16 years). Primary osteoarthritis was the preoperative diagnosis in 81% (n = 161), rheumatoid arthritis in 11% (n = 23) and secondary osteoarthritis (avascular necrosis, Perthes’ disease, developmental dysplasia of the hip and post-traumatic) in 8% (n = 17). The Bauer transgluteal approach was the commonest (77%) approach to the hip joint.
This uncemented femoral implant (Figs. 1 and 2) is a straight-flanged collarless stem made of titanium alloy. The proximal portion is plasma sprayed with a pore size of 50–200 μm.
The stem has an anatomical shape with a wide border medially and support flanges anteroposteriorly together with a lateral derotational wing. Fixation is restricted to the metaphyseal portion [4]. The acetabular component (Figs. 1 and 2) used was a hemispherical press-fit plasma sprayed cup; 93 cups were hydroxyapatite coated and 108 were non-hydroxyapatite porous coated. Stable fixation of the cup is achieved by press fitting as well as frictional forces. The cup has three holes available for supplementary screw fixation. The polyethylene cup was available for sizes 28 and 32 mm. The head size used was 28 mm cobalt chromium in 131 hips or alumina ceramic in 70 cases. In this series the asymmetrical liner with a 10° superolateral offset was used in all cases. The cup was positioned at 45° to the shaft with 10° anteversion.
The prosthesis was sterilised by radiation in a nitrogen atmosphere, a process that has been established in Europe since the mid-1980s.
Routine postoperative management included 24 hours of antibiotic prophylaxis (second generation cephalosporin). Anti-thromboprophylactic stockings and adjusted low dose warfarin thromboprophylaxis was used in all patients. Patients were generally mobilised within 48 hours after surgery with partial weight-bearing using crutches for the first six weeks.
Clinical evaluation
All patients had been evaluated preoperatively and postoperatively at six weeks, six months and then at few yearly intervals until their last review. In all cases clinical notes and radiographs were available for review by two independent observers by consensus of opinion. The Harris hip score functional grading system [7] was used as part of the clinical assessment using the original definitions of pain, support and limp.
Radiological evaluation
Standardised (for magnification) anteroposterior radiographs of the pelvis and proximal femurs were taken at the follow-up visits. Radiographs were analysed by two authors (GS and AP) using the Gruen zones [8] for the femoral stem and DeLee and Charnley zones [9] for the acetabular cup. Areas of periprosthetic osteolysis were noted and measured using the scales on the Patient Archive Computer System (PACS). Other variables assessed included signs of bone resorption, radiolucent lines, the position of the femoral implant (varus, valgus or central), gross evidence of distal migration, and the position of the cup and the angle of lateral opening. Heterotopic bone formation was recorded according to the Brooker classification system [10]. All radiographic assessments were evaluated by comparison with the immediate postoperative result.
Results
At an average of 12.9 years (10.1–16 years) 122 total hip replacements in 98 patients were available for review; 62 patients had died of unrelated causes at a mean of 7.4 years (range 1–13) after initial surgery, and 17 were lost to follow-up between two and 11 years (mean 5.6 years) post-surgery. The clinical notes of these patients revealed that none had been waiting for a revision surgery.
Clinical results
The Harris hip score preoperatively averaged 41 (20–80). The medium-term results published in 2002 revealed an average Harris hip score of 92 (56–96). The average score in this long-term study was 89 (54–97) (Table 1).
There were 12 acetabular revisions. Six cups were revised for aseptic loosening. In one patient there was polyethylene wear with pain necessitating revision of the polyethylene liner. Two patients sustained dislocation of liner and acetabular fracture following a fall. In one patient, both the stem and cup were revised for sepsis in a two-stage procedure to a cemented prosthesis. Recurrent dislocations requiring revision surgery occurred in two patients at six months and six years post-primary surgery. In total one femoral stem was revised for sepsis. No femoral stem was revised for aseptic loosening.
Radiological findings
A total of 116 hip radiographs were available for review beyond ten years (Fig. 2) of primary surgery. This included one patient lost to follow-up at 11 years and three patients who were dead but had X-rays beyond the ten-year period. The mean inclination of the cup was 42°. Radiolucencies (reactive lines) around the acetabulum in one or more zones were seen in 15 hips (13%). These occurred at the cup-bone interface and were less than 2 mm wide. Six hips showed lucencies in at least two of three zones and were subsequently revised. Osteolysis was observed around nine cups across all three zones (8%). There was no measurable correlation between the presence of radiolucent lines around the acetabulum and any clinical outcome measure. Radiolucent lines (reactive lines) or granulomas were seen around 13 femoral stems and these were mostly in Gruen zone 1. A total of 98 hips (88%) were implanted in a neutral position, nine hips (8%) were in a varus position and five hips (4%) were in a valgus position.
Statistical analysis
Survival analysis for the prosthesis [11] was calculated by constructing life tables (Table 2) of the data and also using the Kaplan-Meier survival curves. Using revision as an end point, Kaplan-Meier curves were plotted showing a survival of 95.4% at ten years, 93.6% at 12 years and 89.9% at 15 years (Figs. 3, 4 and 5).
Complications
There was evidence of heterotopic ossification in 22 hips. In 21 hips there was a minor perioperative fracture, usually described as ‘yawning of the anterior femoral cortex’, mainly in the initial period which was thought to represent a learning curve. There were ten documented infections including nine superficial and one deep infection necessitating revision surgery. There were seven documented cases of deep vein thrombosis and one pulmonary embolism treated with subcutaneous heparin. There was one case of sciatic nerve palsy which only resolved partially.
Discussion
This paper reports the long-term results (average 12.9 years) of 112 Bicontact uncemented primary total hip arthroplasties performed at our institution. The cumulative survivorship rate of the femoral stem remains at 100% when compared to the rate published for medium-term results (average 6.8 years) in 2002 [4]. We attributed these good results to careful surgical techniques with the primary goal to achieve press fit and maximal canal filling, as advocated by Engh and Fenwick [12]. The survivorship of the prosthesis however was 92.2% at 14 years compared to the 97.92% survivorship at medium term (five years) for revision due to any cause.
The average Harris hip score of 89 at final review compared favourably with other reported series of cementless total hip arthroplasty, including those where hydroxyapatite-coated hip implants have been used [13–15]. The AML stem [16] and Harris-Galante stem [17] showed survival of 97% at 12 years and 81% at 10.6 years, respectively.
There have been concerns with early polyethylene wear and osteolysis with the first generation ABG cups [5] and also the threaded Weill and the Mercon cups [6], but Philippot et al. [18] demonstrated good results using the dual articulation acetabular cup with 95% survival at 18 years, which is more consistent with our study with the Bicontact cup.
The survival rate for aspetic loosening reported herein is comparable to those found in the literature on the recent models of uncemented and tapered stems at similar follow-ups (Table 3). Parvizi et al. reported a 100% survival rate of a cohort of 121 Taperloc stems (Biomet, Warsaw, IN, USA) [19] at a mean of 11 years; several authors reported no cases of loosening of the CLS stem (Zimmer, Warsaw, IN, USA) at a follow-up of approximately ten years [20].
Apatite-coated implants can form a chemical fixation with strength comparable to that of cortical bone itself. The proximal geometry gives the prosthesis immediate mechanical stability within the metaphysis. The narrow stem acts as an alignment guide at implantation and does not contribute to fixation in anyway [2].
It has been reported that two thirds of the hydroxyapatite coating is resorbed within 16 weeks of implantation and replaced by bone. It seems likely that little hydroxyapatite remains after ten years [21]. Contrary to published series reporting deteriorating results of uncemented stems with time from implantation [22], the uncemented Bicontact stem maintains its 100% survivorship. Partially coated femoral implants often show increased radiolucency in Gruen zone 4 [23]. Radiographic analysis of our cohort of patients revealed radiolucency around nine femoral stems, but there was no radiographic stem loosening. In our series there were 21 minor perioperative fractures. They were all treated conservatively and united uneventfully.
Our findings and those in other series suggest these fractures around an uncemented stem are often incomplete, minimally displaced, do not compromise stability and do not detract from the clinical results [23]. A number of studies have reported the resorption of bone proximally. This is thought to result from stress shielding and is more documented with the use of porous-coated stems [21]. The effect usually manifests within the first six months after implantation. Proximal coating is thought to decrease the incidence of this resorption as is usually seen at the transition of the coated and uncoated portions of the stem [21]. This resorption was seen in 6% of our hips at long term as compared to 3% documented in the medium term. The low incidence of resorption in our series relates to the fact that the titanium stem has a Young’s modulus similar to bone aiding load transfer proximally.
There were no cases of clinical or radiographic loosening in the 112 stems at an average of 13.3 years; one must therefore assume complete proximal femoral integration in all cases. Moreover, there was no incidence of distal femoral endosteal erosion. This finding suggested that bone ingrowth or fibrous integration around the proximally, circumferentially coated femoral components can protect against distal osteolysis. This was also supported by other previous reports using the anatomical medullary locking (AML, DePuy, Warsaw, IN, USA) and the Multilock (Zimmer, Warsaw, IN, USA) stems [24]. Both prostheses had a similar design of femoral components. Radiolucent or reactive lines were seen in nine stems, but only adjacent to the non-coated distal part of the stem. These distal reactive lines are probably due to micromotion between the relatively stiff distal stem and the more elastic bone, enhanced by the strong proximal fixation.
The incidence and amount of heterotopic bone formation (22 hips) is comparable to that reported for other types of total hip replacement. Our low incidence of combined Brooker grades 3 and 4 (11%) compares favourably with some recent studies, including a multicentre study by the ABG Group [25] where hydroxyapatite-coated implants have been used.
The limitations of this study were a lack of lateral radiographic analysis and not establishing the difference between the wear rates among the metal and the ceramic heads.
Conclusion
The ten- to 15-year results of the Bicontact uncemented hip show satisfactory pain relief and good functional result with durable implant stability with excellent stem survival. There were no revisions for aseptic loosening and no radiographic stem loosening documented. The acetabulum results however showed more failures but were comparable with similar series. Results are encouraging and justify the continued use of this prosthesis.
References
Zwartele R, Peters A, Brouwers J, Olsthoorn P, Brand R, Doets C (2008) Long-term results of cementless primary total hip arthroplasty with a threaded cup and a tapered, rectangular titanium stem in rheumatoid arthritis and osteoarthritis. Int Orthop 32(5):581–587
Maheshwari AV, Ranawat AS, Ranawat CS (2008) The use of hydroxyapatite on press-fit tapered femoral stems. Orthopedics 31(9):882–884
McLaughlin JR, Lee KR (2008) Total hip arthroplasty with an uncemented tapered femoral component. J Bone Joint Surg Am 90(6):1290–1296
Badhe NP, Quinnell RC, Howard PW (2002) The uncemented Bi-Contact total hip arthroplasty. J Arthroplasty 17(7):896–901
Badhe S, Livesley P (2006) Early polyethylene wear and osteolysis with ABG acetabular cups (7- to 12-year follow-up). Int Orthop 30(1):31–34
Clarius M, Jung AW, Raiss P, Streit MR, Merle C, Aldinger PR (2009) Long-term results of the threaded Weill cup in primary total hip arthroplasty: a 15-20-year follow-up study. Int Orthop 2009 Jul 24. [Epub ahead of print]
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51(4):737–755
Gruen T, McNeice M, Amstutz H (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 141:17–27
DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 121:20–32
Brooker AF, Bowerman JW, Robinson RA, Riley LH (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55:1629–1632
Altman DG (1991) Practical statistics for medical research. Chapman and Hall, London
Engh CA Sr, Fenwick JA (2008) Extensively porous-coated stems: avoiding modularity. Orthopedics 31(9):911–912
Civinini R, D’Arienzo M, Innocenti M (2008) A ten-year follow-up of the Reflection cementless acetabular component. J Bone Joint Surg Br 90(5):570–573
Gabbar A, Rajan RA, Londhe S, Hyde ID (2008) Ten- to twelve-year follow-up of the Furlong hydroxyapatite-coated femoral stem and threaded acetabular cup in patients younger than 65 years. J Arthroplasty 23(3):413–417
Slack R, Tindall A, Shetty A, James KD, Rand C (2006) 15-year follow-up results of the hydroxyapatite ceramic-coated femoral stem. J Orthop Surg (Hong Kong) 14(2):151–154
Kim YH, Kim JS, Cho SH (1999) Primary total hip arthroplasty with the AML total hip prosthesis. Clin Orthop Relat Res 360:147–158
Cruz-Pardos H, Garcia-Cimbreto E (2001) The Harris-Galante total hip arthroplasty: a minimum 8-year follow-up study. J Arthroplasty 16(5):586–597
Philippot R, Camilleri JP, Boyer B, Adam P, Farizon F (2009) The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop 33(4):927–932
Parvizi J, Keisu KS, Hozack WJ, Sharkey PF, Rothman RH (2004) Primary total hip arthroplasty with an uncemented femoral component: a long-term study of the Taperloc stem. J Arthroplasty 19(2):151–156
Bulow JU, Scheller G, Arnold P, Synatschke M, Jani L (1996) Follow-up (6-9 years) results of the uncemented CLS Spotorno stem. Arch Orthop Trauma Surg 115(3–4):190–194
Tonino AJ, van der Wal BC, Heyligers IC, Grimm B (2009) Bone remodeling and hydroxyapatite resorption in coated primary hip prostheses. Clin Orthop Relat Res 467(2):478–484
Lettich T, Tierney MG, Parvizi J, Sharkey PF, Rothman RH (2007) Primary total hip arthroplasty with an uncemented femoral component: two- to seven-year results. J Arthroplasty 22(7 Suppl 3):43–46
Thorey F, Lerch M, Kiel H, von Lewinski G, Stukenborg-Colsman C, Windhagen H (2007) The uncemented primary Bicontact stem in revision total hip arthroplasty in young patients. Z Orthop Unfall 145(Suppl 1):S40–S43
Nercessian OA, Wu WH, Sarkissian H (2001) Clinical and radiographic results of cementless AML total hip arthroplasty in young patients. J Arthroplasty 16(3):312–316
Kim WY, Muddu BN (2006) Eleven-year results of the ABG I hip replacement. Int Orthop 30(3):182–184
Hallan G, Lie SA, Furnes O et al (2007) Medium- and long-term performance of 11,516 uncemented primary femoral stems from the Norwegian arthroplasty register. J Bone Joint Surg Br 89:1574–1580
Conflict of interest
No sponsorship was required for this research. The authors have full control of all primary data and agree to allow the journal to review their data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Swamy, G., Pace, A., Quah, C. et al. The Bicontact cementless primary total hip arthroplasty: long-term results. International Orthopaedics (SICOT) 36, 915–920 (2012). https://doi.org/10.1007/s00264-010-1123-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1123-4