Abstract
A systematic review of the literature was performed in order to evaluate the role of reduction and internal fixation in the management of Lisfranc joint fracture–dislocations. Articles were extracted from the Pubmed database and the retrieved reports were included in the study only if pre-specified eligibility criteria were fulfilled. Eleven articles were eligible for the final analysis, reporting data for the management of 257 patients. Injuries of the first three metatarsal rays were treated by closed reduction and internal fixation with screws in 16.3% of the patients, open reduction and internal fixation with screws in 66.5% and open reduction and internal fixation with Kirschner wires (K-wires) in 17.1% of the patients. The preferred method for the stabilisation of the fourth and fifth metatarsal rays was K-wires. Screw-related complications were common and were reported in 16.1% of the cases. The mean American Orthopaedic Foot and Ankle Society midfoot score was 78.1 points. Post-traumatic radiographic arthritis was reported in 49.6% of the patients, but only in 7.8% of them it was severe enough to warrant an arthrodesis. We conclude that open reduction and internal fixation of the first three metatarsal rays with screws is a reliable method for the management of Lisfranc injuries. This can be complemented by K-wires application in the fourth and fifth metatarsal rays if needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term ‘Lisfranc dislocation’ is attributed to the French Napoleonic era field surgeon, Jacques Lisfranc, who described a method of forefoot amputation through the tarsometatarsal articulation [4]. Lisfranc injuries are fracture–dislocations of the tarsometatarsal joint complex. The spectrum of injury ranges from low energy sports injuries, to high energy crush injuries [40]. The same variability accounts for the extent of injury, which may be purely ligamentous or associated with fractures of the metatarsals, cuneiforms, navicular and cuboid [40]. Our understanding and treatment modalities of these injuries has evolved during recent decades as a result of diagnostic advances (computed tomography scanning) [5, 26].
Up to 20% of Lisfranc fracture–dislocations are misdiagnosed or missed during the initial evaluation [27]. This makes early and accurate diagnosis a prerequisite for appropriate management of these injuries in order to avoid long-term sequelae and functional impairment. The general consensus is that anatomical reduction and stabilisation of the Lisfranc joint is imperative for good outcome [6, 12, 20, 25, 26]. Conservative management with closed reduction and plaster immobilisation does not appear to have a role in the contemporary treatment of Lisfranc injuries because the initial reduction is often lost when soft tissue swelling subsides [25]. There are a variety of treatments which have been advocated for these injuries. Some surgeons advocate closed fixation using percutaneous wires and/or screws, while others prefer open reduction and internal fixation (ORIF) [5, 6, 26, 40].
To our knowledge, there is a lack of consensus in the literature regarding the surgical treatment, complications, and functional outcomes of Lisfranc injuries. We performed a comprehensive review of clinical studies reporting on the management of Lisfranc fracture–dislocations with reduction and internal fixation, in order to provide “best practice” recommendations for treatment.
Material and methods
We conducted an internet-based search for English language articles in the medical literature published between January 1985 and January 2010, using the PubMed search engine, with the following key words: ‘Lisfranc joint’, ‘tarsometatarsal joint’, ‘injuries’, ‘fracture’, ‘dislocation’, ‘treatment’ and ‘outcome’ joined with Boolean operators. All potentially relevant articles were retrieved, their references were scrutinised for further missing citations and assessed for eligibility using the following predetermined selection criteria: (1) the primary treatment method for the Lisfranc injuries was reduction (open or closed) and internal fixation; (2) the cases reported were treated within the first three weeks after injury (acute phase); (3) at least ten patients were included in any study eligible for evaluation; (4) the minimum follow-up time for every patient was 12 months; (5) at least one of the outcome parameters of interest was included, namely, functional score, patient satisfaction, pain, complications and return to work; and (6) the quality of the studies was estimated using a previously reported and tested scoring system [29]. This scoring system was developed on the basis of criteria assessment as follows: Were the inclusion/exclusion criteria defined? Was the number of withdrawals or drops-out known? Was the follow-up pre-specified? Were the outcomes of interest clearly described? Did the study include characteristics, such as the type of Lisfranc injury, the surgical technique which was used, and the hardware that was used which may affect the outcome of interest? A positive answer to each of these questions scored 2 points, a positive answer without all of the required data scored 1 point and no data at all scored 0 points. A total of 5 points as a threshold was necessary for each study to be considered as fulfilling the quality criterion.
Two independent assessors reviewed the studies. Any disagreements were resolved by a consensus. Statistical analysis was performed using Microsoft Excel 2003 for Windows (Microsoft Corp, Redwood, Washington). Because relevant information was provided differently, it was not always possible to calculate each parameter with data from all eligible studies. The number of pooled studies for each parameter was recorded.
Results
The electronic search through PubMed yielded 168 citations out of which 53 potentially relevant full articles were retrieved and were subjected to further analysis. A total of 11 papers satisfied the inclusion criteria and received critical analysis [2, 11, 17, 21, 23, 30, 31, 33, 34, 38, 39]. There were seven case series retrospective studies [2, 17, 30, 31, 33, 38, 39], two comparative cohort studies [23, 34], and two prospective randomised control trials–comparative studies [11, 21]. From the latter four studies only the data from the groups of patients who were treated by internal fixation were included in the review. In nine articles [2, 11, 17, 21, 23, 30, 33, 34, 39] there was no difference in the evaluation process, and in the remaining two papers [31, 38] there was one point of difference in the quality scoring process, which was not significant.
Clinical data
The 11 papers [2, 11, 17, 21, 23, 30, 31, 33, 34, 38, 39] analysed in-depth reported 328 injuries in 325 patients (Table 1). Two hundred fifty-seven patients (79.0%) with 257 injuries (78.3%) were available for review. Their mean age was 35.1 years (range, 16–77) and the mean follow-up time was 43.9 months (range, 12–180).
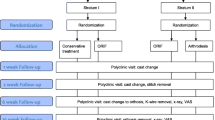
Details about the nature and type of injury were given in eight papers [11, 17, 21, 31, 33, 34, 38, 39] (Fig. 1). Pure ligamentous injuries were reported in 60 patients (42.5%) and osseoligamentous injuries in 81 patients (57.5%) [11, 17, 21, 31, 33]. Closed injuries were reported in 77 patients (87.5%), and open injuries in 11 patients (12.5%) [17, 33, 38, 39]. High energy injuries were described in 76 patients (58.0%) and low energy injuries in 55 patients (42.0%) [11, 17, 21, 33, 34, 38].
In one study [23] the categorisation of injuries was done using the Hardcastle classification [10], in two studies [31, 33] using the Myerson classification [27] and in five studies [2, 17, 30, 34, 38] using the Quénu and Küss classification [32]. In three studies [11, 21, 39] no classification of injuries was encountered.
Treatment modalities
In one study [31] closed reduction and internal fixation (CRIF) with percutaneous screws was reported in 42 patients (16.3%). In the remaining of the studies [2, 11, 17, 21, 23, 30, 33, 34, 38, 39] formal open reduction of the three medial metatarsals and cuneiforms was accomplished using one or two intermetatarsal (web space) incisions. In particular, ORIF of the three medial metatarsals and cuneiforms applying Kirschner wires (K-wires) was used in 44 patients (17.1%) [30, 34, 38] and ORIF placing screws was used in 171 patients (66.5%) [2, 11, 17, 21, 23, 33, 34, 39] (Fig. 2).
Small fragment screws (3.5- and 4.0-mm) were used in 186 patients (72.3%) [2, 11, 17, 21, 31, 33, 34], large fragment 4.5-mm screws were used in 16 patients (6.2%) [23], while in one study [39] no screw size data were described.
Transfixation of the fourth and fifth metatarsals was done only if they were unstable, using K-wires in 96 patients (37.3%) [21, 23, 30, 33, 34] and 3.5- or 4.0-mm screws in 34 patients (13.2%) [2]. In contrast, routine transfixation of the lateral column with K-wires was reported in only two studies [11, 17], presenting the outcome of 62 patients (24.1%).
Finally, primary arthrodesis was one of the treatment modalities implemented for Lisfranc injuries in three studies [11, 21, 23] (Table 2).
Postoperative protocol
Postoperative immobilisation (short leg splint or cast) was routinely used in the patients of all of the studies [2, 11, 17, 21, 23, 30, 31, 33, 34, 38, 39]. Gradual progression to full weight bearing was permitted in ten studies [2, 11, 17, 21, 23, 30, 31, 33, 34, 38] after an initial non (or touch) weight bearing mean period of 8.1 weeks (range, 6–12).
Routine hardware removal, after a prespecified period of time (8, 8, 12 and 12 weeks, respectively), was described in four studies [11, 23, 33, 34]. Routine hardware removal was also reported in two additional studies [2, 39], but only after completion of healing. In two studies [17, 21], hardware removal was suggested only if it caused problems (i.e. broken screws), while in three others [30, 31, 38] no recommendation about hardware removal was given. Regarding the type of hardware, screws were removed at eight weeks in 37 patients (14.4%) [33, 34], at 12 weeks in 30 patients (11.6%) [11, 23] and at 16 weeks in 45 patients (17.5%) [3, 39]. On the other hand, K-wires were usually removed after six to eight weeks [17, 34].
Complications
Complications were reported in eight studies [2, 11, 17, 21, 23, 30, 33, 34] describing the results of 192 patients (74.7%). Compartment syndrome was reported in five patients (2.6%) [2, 17, 34], skin problems in seven patients (3.6%) [17, 30, 34], infection in three patients (1.5%) [2, 30, 34], deep vein thrombosis in one patient (0.5%) [17], reflex sympathetic dystrophy in two patients (1.0%) [23], screw problems in 31 patients (16.1%) [2, 11, 17, 21, 33] and amputation in two patients (1.0%) [2, 33].
Functional assessment
The American Orthopaedic Foot and Ankle Society (AOFAS) midfoot score [15] was used to evaluate the functional outcome in 146 patients (56.8%) of six studies [17, 21, 31, 33, 34, 39]. The mean score was 78.1 (range, 30–100).
In two of these studies [17, 34] an additional functional score was used. In particular, Kuo et al. [17] used the long-form Musculoskeletal Function Assessment (MFA) score [22] where in 42 patients (16.3%) the mean score was 18 points (range, 0–55), and Rammelt et al. [34] used the Maryland foot score [27], reporting a mean score of 85 points (range, 70–100) in 20 patients (7.7%).
Two functional assessment scores for the evaluation of the results in 14 patients (5.4%) were also used in the study of Henning et al. [11]. The mean short-form MFA score was 17.3 (range, 1–23), and the mean Short-Form 36 (SF-36) score was 48.6 (range, 44–53.8).
The Hardcastle et al. [10] evaluation assessment was used in two studies [30, 38] (35 patients, 13.6%), depicting 27 patients (77.1%) with good results and eight patients (22.8%) with fair results.
Mulier et al. [24] used the Baltimore painful foot score [14] for the evaluation of 16 patients (6.2%) reporting a mean value of 78 (range, 60–100). A further analysis of the literature revealed that the so-called ‘Maryland foot score’ and the ‘Baltimore painful foot score’ historically use the same evaluation form. Consequently, if one combines the results of Mulier et al. [24] and Rammelt et al. [34] where they were used, there is a mean score of 81.5 points in 36 patients (14.0%).
Finally, in a study by Arntz et al. [2] of 34 patients (13.2%), the patients and their physicians rated the results as excellent or good in 28 cases (82.3%) and fair or poor in six cases (17.6%), using their own evaluation criteria.
Fifty-eight (75.3%) out of 77 patients (29.9%) in four studies [11, 21, 30, 34] were satisfied with the result. Fifty-two (86.6%) out of 60 patients (23.3%) in three studies [2, 11, 38] were expressing no or slight pain during their last follow-up. Furthermore, 63 (69.2%) out of 91 patients (35.4%) in five studies [2, 11, 21, 38, 39] reported that they returned to their previous activities and work.
Post-traumatic arthritis on radiographic examination was reported in 80 (49.6%) out of 161 patients (62.6%) in seven studies [2, 17, 21, 23, 34, 38, 39]. Post-injury arthrodesis for post-traumatic arthritis had already been performed in 15 (7.8%) out of 192 patients (74.7%) during the last follow-up in five studies [11, 17, 21, 23, 33].
Discussion
The tarsometatarsal complex consists of three functional columns [16]. The medial column is formed by the base of the first metatarsal and the medial cuneiform, the middle column is formed by the second and third metatarsals and their respective cuneiforms and the lateral column is formed by the fourth and fifth metatarsals and the cuboid. Diagnosis, management and post-injury evaluation of Lisfranc fracture–dislocations have evolved in recent years.
Historically, injuries of the tarsometatarsal complex are considered to be relatively rare, with a reported incidence of 1 per 55,000 yearly, making up for 0.2% of all fractures [1, 7]. However, these data have been disputed [42] and as they are related to older reports, whereby one could assume that the changes in civil trauma configurations, the higher index of suspicion for these injuries and the advances in imaging facilities might have altered these figures.
Up to 20% of Lisfranc fracture–dislocations are misdiagnosed or missed during the initial evaluation [27]. If overlooked or not treated correctly tarsometatarsal fracture–dislocations frequently result in painful malunion and impaired function whereas a delayed diagnosis or misdiagnosis of a major Lisfranc injury can compound associated vascular compromise. A high index of suspicion when evaluating any patient complaining of midfoot pain or any polytraumatised patient with distracting injuries must be present. Pathognomic features of Lisfranc joint disruption may be the plantar ecchymosis at the midfoot level and the pain with palpation or manipulation of the tarsometatarsal joints. In patients with subtle signs, the provocative manoeuvre of passive abduction and pronation of the forefoot while holding the hindfoot fixed with the other hand can be useful. In radiographs, look for any diastasis of the base of the first and second metatarsals and for the “fleck” sign which is present in approximately 90% of cases [27]. Further imaging should include weight-bearing views and comparison views. CT or MRI may reveal occult fractures and dislocations in case of negative plain radiographs. Missed Lisfranc fracture–dislocations can lead to persistent instability, deformity, or arthritis, and re-evaluation may be necessary if pain and swelling continue for ten days after the injury.
Injuries to the joint can be caused by direct or indirect forces. The latter are more common and include bending or twisting moments applied to the midfoot [5, 25], while the former are mostly crush injuries, which may be associated with notable soft tissue trauma. Currently, the two most common mechanisms of injury are motor vehicle accidents, which are high energy injuries, and falls from height which are mainly lower energy injuries [9, 27]. In our review there is evidence that high energy injuries are more common than low energy injuries (58.0% and 42.0%, respectively), with closed injuries to be the most encountered pattern (87.5%). This might be explained by the fact that the studies eligible for review originate mainly from the last decade, revealing the higher incidence of high energy trauma that it is currently encountered.
Quénu and Küss [32] published a classification in 1909 based on their column concept of the forefoot. They divided injuries into three categories: homolateral, isolated, and divergent. In 1982, Hardcastle et al. [10] described a classification system based on that of Quénu and Küss [32]. At the time of publication, the authors suggested that it was useful to determine treatment. Although the recommended treatment has changed for some of the injuries, this classification continues to be used today [23]. The injuries are divided into three categories: type A (complete displacement of all of the metatarsals), B (displacement of one or more of the metatarsals), and C (divergent pattern). Myerson et al. [27] (Fig. 3) modified the classification to include type A (total incongruity, medial–lateral [Fig. 4]), isolated medial or lateral incongruity patterns (types B1 and B2 [Fig. 5], respectively), and type C injuries are subdivided as to whether all four (type C2 [Fig. 6]) or fewer metatarsals (type C1) are divergently displaced. This columnar classification seems to give a more utilitarian approach to the management of incongruity and instability [31, 33]. However, the simplicity and reproducibility of the Quénu and Küss classification [32] makes it still valid, even though it is the older one [2, 17, 30, 34, 38].
The importance of anatomical reduction for improved outcome has always been recognised in the management of Lisfranc injuries [35, 40]. Initially this was accomplished with plaster application after closed reduction. Nevertheless, during the post-treatment period and as swelling was diminished, loss of reduction was noticed [27]. This method was reinforced by the application of K-wires, but still the premature removal of these resulted in subsequent diastasis or re-dislocation. Arntz et al. [2] popularised the use of screws in preference to K-wires. Our review revealed that screws were the favourite method of fixation in 213 patients (82.8%) [2, 11, 17, 21, 23, 31, 33, 34, 39], which were introduced after open reduction in 171 of them (73.7%) [2, 11, 17, 21, 23, 33, 34, 39]. Furthermore, screw fixation of the medial and middle columns provides greater biomechanical stability than pinning alone [18].
In only three studies [30, 34, 38] (44 patients, 17.1%), K-wires were used for definite fixation after open reduction. Twenty eight of these injuries were isolated (partial incongruity) injuries, according to Quénu and Küss classification [32], which might have made the choice of this method of treatment feasible. Small fragment screws (3.5- or 4.0-mm) were preferred and were used in 186 (83.7%) out of 222 patients (86.3%) in nine studies [2, 11, 17, 21, 23, 31, 33, 34, 39].
The majority of surgeons seems to prefer to stabilise the lateral column (fourth and fifth metatarsals) with K-wires, only if unstable [21, 23, 30, 33, 34], while a few prefer to do it routinely [17]. This method of stabilisation allows some motion that is normally present in the lateral column [6]. In only one study [2], were screws used for the stabilisation of the lateral column, which might reflect the enthusiasm that was apparent on the initial reports of applying rigid fixation in the treatment of all of these injuries.
Postoperatively, consensus seems to exist about the necessity of protection of the reduction and the fixation for a minimum of six weeks, but there is conflicting advice about the necessity for removal of the screws. It is clear that screw problems are among the most frequent complications reported in the our review. In 31 (16.1%) out of 192 patients (74.7%) in five studies [2, 11, 17, 21, 33], it was necessary to remove broken or problem-causing screws. Some recent case series reports [37, 41] have described the use of absorbable screws in these injuries in order to overcome these complications. However, it seems to be too early to draw any conclusions for their efficiency.
The AOFAS midfoot score [15] evaluates the mid part of the foot, taking into account parameters such as pain intensity, function limitation, the necessity for special shoes, walking performance on several ground conditions, gait abnormality and foot alignment. The score can range from 0 to 100, with 100 points reflecting an excellent outcome. It is a useful and reproducible evaluation tool and in this review it was used to describe the outcome in 146 patients (56.8%) in six studies [17, 21, 31, 33, 34, 39]. It does not differ substantially from the Baltimore painful foot score (or Maryland foot score) [27] as pain, function, foot alignment (cosmetics) and motion are also the main parameters under evaluation. However, one would be more interested if there were data concerning patients’ satisfaction from their treatment and even more if there were data reporting on their ability to return to their work or sporting and leisure activities. Nevertheless, the small number of patients that have reported these data in our review does not permit any conclusion.
On the contrary, what is clear from this review is that post-traumatic arthritic changes during follow-up radiographic evaluation remain the most common complication after Lisfranc injuries. These changes, which range from slight degenerative changes to complete loss of joint space, were presented in 80 (49.6%) out of 161 patients (62.6%) in seven studies [2, 17, 21, 23, 34, 38, 39]. Many authors have concluded that the development of degenerative changes is markedly increased if the presence or the extent of injury has initially been unrecognised, if the injury has been only partially treated, if the anatomy was not restored, or even if the injury was purely ligamentous and not osseoligamentous [1, 3, 8, 10, 19, 35]. Additionally, one should take into consideration that the initial articular cartilage damage that occurs at the time of injury cannot be estimated pre-operatively, but it is only appreciated after an adverse outcome becomes obvious. All the degenerative changes differ. As was stated by Myerson [25], “it is particularly important to recognise the lack of association between the extent of arthritis and symptoms”. Degenerative changes of the joint complex at the lateral column may not be as painful as respective changes at the medial and especially middle column, because it is known that the lateral column of the joint complex is the most mobile in both the sagittal and horizontal planes [28]. If conservative measures fail to relieve the symptoms of these changes, arthrodesis of the painful tarsometatarsal joints is the treatment of choice [13, 16, 36]. In our review, post-injury arthrodesis for post-traumatic arthritis was reported in 15 (7.8%) out of 192 patients (74.7%) during the last follow-up in five papers [11, 17, 21, 23, 33].
The rest of the reported complications could be considered minor or even expected for this type of injury. Nevertheless, one should not underestimate the possibility that some of these injuries might even result in amputation, especially in the high energy crush type injury variation [2, 33].
Conclusions
We performed a systematic review of the literature on acute Lisfranc fracture–dislocations with regard to treatment, complications, and functional assessment. There appears to be comparable incidence of purely ligamentous and osseoligamentous injuries.
Open reduction using one or two parallel incisions in the dorsum of the foot and small fragment screws application (3.5- and 4.0-mm) seems to be the preferred method of management for the injuries in the joints of the medial and middle column (first, second and third metatarsals), while K-wires can be used for the stabilisation of the lateral column (fourth and fifth metatarsals) in case of instability. Screws may create postoperative discomfort or complications but it is not clear when and if they should be removed.
A score above 75 points on the AOFAS midfoot scale [15] can be expected in appropriately treated patients, but it is not clear up to what extent it reflects their ability to return back to their previous activities. Furthermore, the prevalence of degenerative radiographic changes is considerable, even though it might not correlate with symptoms, but which and how many of these patients are going to need an arthrodesis in the future is not evident.
Further well-designed prospective, randomised controlled studies are desirable to answer certain questions about the value and effectiveness of the reduction and internal fixation of Lisfranc injuries, especially in comparison with alternative treatments such as primary or delayed arthrodesis.
References
Aitken AP, Poulson D (1963) Dislocations of the tarsometatarsal joint. J Bone Joint Surg Am 45-A:246–260
Arntz CT, Veith RG, Hansen ST Jr (1988) Fractures and fracture-dislocations of the tarsometatarsal joint. J Bone Joint Surg Am 70:173–181
Aronow MS (2006) Treatment of the missed Lisfranc injury. Foot Ankle Clin 11:127–142
Cassebaum WH (1963) Lisfranc fracture-dislocations. Clin Orthop Relat Res 30:116–129
Coetzee JC (2008) Making sense of Lisfranc injuries. Foot Ankle Clin 13:695–704
Desmond EA, Chou LB (2006) Current concepts review: Lisfranc injuries. Foot Ankle Int 27:653–660
English TA (1964) Dislocations of the metatarsal bone and adjacent toe. J Bone Joint Surg Br 46:700–704
Goossens M, De Stoop N (1983) Lisfranc's fracture-dislocations: etiology, radiology, and results of treatment. A review of 20 cases. Clin Orthop Relat Res 176:154–162
Haapamaki V, Kiuru M, Koskinen S (2004) Lisfranc fracture-dislocation in patients with multiple trauma: diagnosis with multidetector computed tomography. Foot Ankle Int 25:614–619
Hardcastle PH, Reschauer R, Kutscha-Lissberg E et al (1982) Injuries to the tarsometatarsal joint. Incidence, classification and treatment. J Bone Joint Surg Br 64:349–356
Henning JA, Jones CB, Sietsema DL et al (2009) Open reduction internal fixation versus primary arthrodesis for Lisfranc injuries: a prospective randomized study. Foot Ankle Int 30:913–922
Hunt SA, Ropiak C, Tejwani NC (2006) Lisfranc joint injuries: diagnosis and treatment. Am J Orthop 35:376–385
Johnson JE, Johnson KA (1986) Dowel arthrodesis for degenerative arthritis of the tarsometatarsal (Lisfranc) joints. Foot Ankle 6:243–253
Kenzora JE, Edwards CC, Browner BD et al (1981) Acute management of major trauma involving the foot and ankle with Hoffmann external fixation. Foot Ankle 1:348–361
Kitaoka HB, Alexander IJ, Adelaar RS et al (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15:349–353
Komenda GA, Myerson MS, Biddinger KR (1996) Results of arthrodesis of the tarsometatarsal joints after traumatic injury. J Bone Joint Surg Am 78:1665–1676
Kuo RS, Tejwani NC, Digiovanni CW et al (2000) Outcome after open reduction and internal fixation of Lisfranc joint injuries. J Bone Joint Surg Am 82-A:1609–1618
Lee CA, Birkedal JP, Dickerson EA et al (2004) Stabilization of Lisfranc joint injuries: a biomechanical study. Foot Ankle Int 25:365–370
Lenczner EM, Waddell JP, Graham JD (1974) Tarsal-metatarsal (Lisfranc) dislocation. J Trauma 14:1012–1020
Loveday D, Robinson A (2008) Lisfranc injuries. Br J Hosp Med (Lond) 69:399–402
Ly TV, Coetzee JC (2006) Treatment of primarily ligamentous Lisfranc joint injuries: primary arthrodesis compared with open reduction and internal fixation. A prospective, randomized study. J Bone Joint Surg Am 88:514–520
Martin DP, Engelberg R, Agel J et al (1996) Development of a musculoskeletal extremity health status instrument: the Musculoskeletal Function Assessment instrument. J Orthop Res 14:173–181
Mulier T, Reynders P, Dereymaeker G et al (2002) Severe Lisfrancs injuries: primary arthrodesis or ORIF? Foot Ankle Int 23:902–905
Mulier T, Reynders P, Sioen W et al (1997) The treatment of Lisfranc injuries. Acta Orthop Belg 63:82–90
Myerson MS (1999) The diagnosis and treatment of injury to the tarsometatarsal joint complex. J Bone Joint Surg Br 81:756–763
Myerson MS, Cerrato R (2009) Current management of tarsometatarsal injuries in the athlete. Instr Course Lect 58:583–594
Myerson MS, Fisher RT, Burgess AR et al (1986) Fracture dislocations of the tarsometatarsal joints: end results correlated with pathology and treatment. Foot Ankle 6:225–242
Ouzounian TJ, Shereff MJ (1989) In vitro determination of midfoot motion. Foot Ankle 10:140–146
Papadokostakis G, Papakostidis C, Dimitriou R et al (2005) The role and efficacy of retrograding nailing for the treatment of diaphyseal and distal femoral fractures: a systematic review of the literature. Injury 36:813–822
Perez Blanco R, Rodriguez Merchan C, Canosa Sevillano R et al (1988) Tarsometatarsal fractures and dislocations. J Orthop Trauma 2:188–194
Perugia D, Basile A, Battaglia A et al (2003) Fracture dislocations of Lisfranc's joint treated with closed reduction and percutaneous fixation. Int Orthop 27:30–35
Quenu E, Küss G (1909) Etude sur les luxations du metatarse (luxations metatarsotarsiennes) du diastasis entre le 1er et le 2e metatarsien. Rev Chir 39:1093–1134
Rajapakse B, Edwards A, Hong T (2006) A single surgeon's experience of treatment of Lisfranc joint injuries. Injury 37:914–921
Rammelt S, Schneiders W, Schikore H et al (2008) Primary open reduction and fixation compared with delayed corrective arthrodesis in the treatment of tarsometatarsal (Lisfranc) fracture dislocation. J Bone Joint Surg Br 90:1499–1506
Richter M, Wippermann B, Krettek C et al (2001) Fractures and fracture dislocations of the midfoot: occurrence, causes and long-term results. Foot Ankle Int 22:392–398
Sangeorzan BJ, Veith RG, Hansen ST Jr (1990) Salvage of Lisfranc's tarsometatarsal joint by arthrodesis. Foot Ankle 10:193–200
Saxena A (2005) Bioabsorbable screws for reduction of Lisfranc's diastasis in athletes. J Foot Ankle Surg 44:445–449
Tan YH, Chin TW, Mitra AK et al (1995) Tarsometatarsal (Lisfranc's) injuries—results of open reduction and internal fixation. Ann Acad Med Singapore 24:816–819
Teng AL, Pinzur MS, Lomasney L et al (2002) Functional outcome following anatomic restoration of tarsal-metatarsal fracture dislocation. Foot Ankle Int 23:922–926
Thompson MC, Mormino MA (2003) Injury to the tarsometatarsal joint complex. J Am Acad Orthop Surg 11:260–267
Thordarson DB, Hurvitz G (2002) PLA screw fixation of Lisfranc injuries. Foot Ankle Int 23:1003–1007
Vuori JP, Aro HT (1993) Lisfranc joint injuries: trauma mechanisms and associated injuries. J Trauma 35:40–45
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stavlas, P., Roberts, C.S., Xypnitos, F.N. et al. The role of reduction and internal fixation of Lisfranc fracture–dislocations: a systematic review of the literature. International Orthopaedics (SICOT) 34, 1083–1091 (2010). https://doi.org/10.1007/s00264-010-1101-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1101-x