Abstract
Fractures of the head and neck of the femur in children are very rare, occurring only after a high-velocity trauma, e.g. a fall from a height. This analysis shows the clinical course of traumatic femoral head and neck fractures in paediatric patients. Predisposing factors for poor outcome or fracture complications, such as non-union or femoral head necrosis, are described. Between 1993 and 2006, 16 paediatric patients with proximal femoral fractures were treated at the Level One Trauma Centre of the Medical University of Vienna. The minimum follow-up was two years. Inclusion criteria were age less then 16 years, intact growth plate and a proximal femoral fracture according to the classification by Delbet and Colonna. Exclusion criteria were pathological fractures or fractures of the subtrochanteric region (6/16). Ten patients met the inclusion criteria. Two patients were lost to follow-up. Therefore eight patients were included in the study. All patients except one were operated upon within 48 h after the injury (“primary”) and healed without further complications. A single case was managed by “secondary” surgical treatment, two weeks after the initial trauma resulting in femoral head necrosis that healed without any subjective complaints. This case series confirms the importance of early surgical fixation of proximal femoral fractures in paediatric patients. An operative intervention later then 48 h after the initial trauma may increase the risk of complications such as femoral head necrosis, particularly in Delbet type I fractures (traumatic slipped capital femoral epiphysis).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of the head and neck of the femur in a paediatric patient population are very rare [1–4]. They can be divided into traumatic and non-traumatic lesions. An adequate force that produces a fracture in the proximal femur of a child normally occurs only during high-velocity injury, for example a fall from a great height or motor vehicle accidents [5]. In cases of non-traumatic fractures, prior bone deformation or bone tumours of all types (benign/malignant) should be considered. The applied force that results in a fracture is often inadequate, such as simple falls or torsions of the hip region [6]. In these cases the fractures and the underlying pathology must be treated. Recurrent fractures followed by multiple procedures are reported in this subgroup [6–8].
Because of the rarity of these fractures, surgical treatment is individual and any information on the optimal surgical procedures is welcome. This analysis shows the clinical course of fractures of the head and neck of the femur in paediatric patients. Predisposing factors for poor outcome or fracture complications, such as non-union or femoral head necrosis, are described.
Patients and methods
A series of consecutive patients was analysed for this retrospective survey. Between 1993 and 2006, 16 paediatric patients with fractures of the femoral head and neck were treated at the Level One Trauma Centre of the Medical University of Vienna. The Vienna University Hospital where the Trauma Centre is located is one of the two hospitals treating children with acute trauma serving the Vienna area with 2 million inhabitants. The average number of paediatric patients (new cases) seen in the Trauma Centre is over 9,500 per annum. The minimum follow-up was two years.
Inclusion criteria were age less then 16 years, intact growth plate and a fracture of the femoral head or neck according to the classification by Delbet and Colonna [9, 10]. According to Colonna’s description of Delbet’s classification traumatic paediatric hip injuries were classified into type I: transepiphyseal separations with or without dislocation of the femoral head from the acetabulum, type II: transcervical fractures, displaced and non-displaced, type III: cervicotrochanteric fractures, displaced and non-displaced and type IV: intertrochanteric fractures. According to Rockwood et al. “in children severe violence is necessary to produce a type I injury. In adolescents, however, less trauma may be necessary because it may represent one end of the slipped capital femoral epiphysis” [11]. Exclusion criteria were pathological fractures or fractures of the subtrochanteric region (6/16). Ten patients met the inclusion criteria. Two patients were lost to follow-up. Therefore eight patients were included in the study.
At the time of the final follow-up all patients underwent clinical examination and radiographic evaluation in two planes (see Table 1). In cases of suspected femoral head necrosis or non-union consecutive magnetic resonance imaging (MRI) was performed. Signs of femoral head necrosis were classified by the score of Ratliff [3, 4]. Avascular necrosis in children according to Ratliff is classified into type I: whole head involvement, resulting in complete collapse of the femoral head, type II: partial head involvement, resulting in the minimal collapse of the femoral head and type III: an area of avascular necrosis from the fracture line to the physis. The time of bony consolidation defined by the callus on both the anteroposterior and lateral radiographs was noted as well as the time until hardware removal. Predisposing factors for possible complications, such as time interval between injury and initiation of the treatment, time interval until full weight-bearing and the influence of additional application of a cast, were analysed. The initial surgical treatment was considered as “primary” if the procedure had been performed earlier then 48 h after the injury and “secondary” after more then two days. In order to study the influence of the postoperative rehabilitation protocol, the weight-bearing periods were divided into non-weight-bearing for up to six weeks (“early rehabilitation”) and six to 12 weeks (“late rehabilitation”). The same applies to the time period for the cast application.
Results
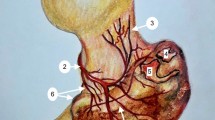
Eight patients were included in this study, six male and two female. Their median age was 11.6 (range: 3–15 years). The follow-up was at least 24 months (median: 46 months, range: 24–80 months). Five of eight were classified as Delbet type I (traumatic slipped capital femoral epiphysis), none of eight were Delbet type II, two of eight were Delbet type III and one of eight was Delbet type IV [9, 10]. A single case was managed by “secondary” surgical treatment. A ten-year-old girl fell from a horse. Initial surgical treatment was delayed and she was referred to our department only two weeks after injury. A proximal femoral fracture was diagnosed on the grounds of the adequate trauma (fall from a horse). The fracture was classified as Delbet type I (acute slipped capital femoral epiphysis) on the acute radiograph (not shown). She was treated with three K-wires. However, the K-wires showed signs of migration during the clinical course. Because of this migration, the K-wires were removed after six weeks. She did not receive additional cast treatment and was allowed full weight-bearing. Eight weeks after removal of the K-wires, i.e. 14 weeks after the initial trauma, she complained of pain typical for femoral head necrosis. MRI was performed, but this did not show any pathological signs. The patient was advised to walk without weight-bearing. Four weeks later a new MRI showed incipient femoral head necrosis classified as Ratliff II (with diffuse oedema of the bone marrow in the femoral head and neck, see Fig. 1). To prevent total necrosis of the femoral head, a valgus osteotomy of the hip was performed five months after the initial injury.
In the patients who received “primary” treatment, no case of head necrosis or non-union was observed.
A 14-year-old boy was injured by a fall during skating. The radiograph showed a Delbet type I proximal femoral fracture (acute slipped capital femoral epiphysis) of the right side. The fracture was reduced and stabilised with three K-wires. The boy was free of pain and started skating about two months after discharge from the hospital. He presented again after a fall during skating about 12 weeks after the initial injury. Although the position of the patient in the radiographs taken at the second injury was different in comparison to the postoperative radiographs, the radiograph showed a superior migration of two of the K-wires. A K-wire was protruding into the articular gap (Fig. 2f, arrow). Thus, all implants were removed. The further clinical course was uneventful. Now, the boy has given up skating and the fracture healed without further clinical abnormalities.
Of our eight patients, four had early rehabilitation (full weight-bearing after six weeks) and four had late rehabilitation (weight-bearing after 12 weeks). No difference in the outcome of these two groups could be observed. Two patients had additional cast fixation for four to six weeks, and six of eight had no additional fixation. Both cases with complications (head necrosis and K-wire perforation, respectively) did not receive cast fixation. Both cases were classified as Delbet type I fractures (traumatic slipped capital femoral epiphysis).
Discussion
Traumatic fractures of the proximal metaphyseal end of the femur in children are very rare and may be seen in a general orthopaedic practice once or twice in a decade [12, 13]. Even academic referral centres are only able to present studies reporting about ten to 40 cases, treated within seven to 25 years [14–16]. Therefore it is difficult to define what evidence-based knowledge for this entity there is. The major complications following these fractures are avascular femoral head necrosis (21–80%) [1, 2, 5, 6, 14, 16, 17], coxa vara (8–21%) [1, 2, 6] and premature physeal closure (28–30%) [1, 2, 6, 17].
The largest series over the years was presented by Canale and co-workers [1]. The authors reported about 87 cases and compared results of the late cases with those of a previously reported series [2]. The main conclusion drawn from their data is that the rate of avascular femoral head necrosis is directly related to the initial degree of dislocation. The authors recommend early and accurate reduction and fixation as a main therapeutic goal.
Other predisposing factors for these complications, such as the time interval between the injury and the start of the treatment, the choice of implant, the surgical protocol (e.g. crossing of the growth plate, evacuation of the joint) or the postoperative rehabilitation protocol, are subject of controversy. Most of the authors recommend an early reduction and treatment; Ng and Cole define an interval of 36 h as optimal for the primary procedure [18]. Closed reduction and traction in abduction is only recommended for Delbet type I fractures [17]. For operative treatment many different procedures are described, including open reduction and internal fixation using K-wires, cannulated screws or nails [5, 6, 14, 16–20]. There is no evidence that one or other implant influences the rate of postoperative complications, such as avascular femoral head necrosis or coxa vara [17, 18]. However, Canale and co-workers found evidence that the use of a smaller number of pins seems to reduce the complication rate [1]. Several authors underline the importance of not crossing the growth plate with the implant unless radiological findings show that it is almost fused [5]. On the other hand, there is experimental evidence that crossing the growth plate leads to premature closure if the pins are drilled from the epiphysis into the metaphysis. If the drilling direction is the other way around, i.e. from the metaphysis into the epiphysis, as in the proximal femur, there is no increased rate of premature physeal closure [21].
The importance of early decompression of the joint by aspiration or capsulotomy is still unclear. Ng and Cole [18] did not find any significant difference in their own study population, but in a statistical analysis including cases from various published case series they could show a tendency for a lower rate of avascular femoral head necrosis after early evacuation of the joint.
Very few studies mention the importance of the postoperative protocol. There are no data that prove the influence of early or late weight-bearing, but the use of a supplementary hip spica may improve the result. Our own patient population is too small to support this recommendation, as it does not show any significant difference in outcome related to the postoperative care protocol or the use of an additional cast.
In the long-term follow-up, the natural history after femoral neck fractures in childhood leads to a high rate of radiological deformities of the affected joint. Nevertheless these radiological changes do not seem to have a clinical significance [20].
A clear limitation of our study is the small patient cohort. But inasmuch as the majority of literature on this topic also report only limited experience of this rare condition, the results of this study at least support the common treatment strategies, in particular the call for early operative intervention. One of eight patients developed avascular femoral head necrosis after late initial presentation. Due to the rarity of proximal femoral neck fractures in paediatric patients and the small number of patients, it is not yet clear whether operative intervention later than 48 h after the initial trauma increases the risk of complications such as femoral head necrosis as described in the literature [18].
Conclusion
This study supports the importance of early surgical fixation of proximal femoral fractures in paediatric patients. An operative intervention later then 48 h after the initial trauma may increase the risk of complications such as femoral head necrosis, especially in Delbet type I fractures (acute slipped capital femoral epiphysis). The postoperative protocol, e.g. the time interval of limited weight-bearing or an additional cast fixation, does not contribute significantly to the functional or radiological outcome.
References
Canale ST (1990) Fractures of the hip in children and adolescents. Orthop Clin North Am 21:341–352
Canale ST, Bourland WL (1977) Fracture of the neck and intertrochanteric region of the femur in children. J Bone Joint Surg Am 59:431–443
Ratliff AH (1962) Fractures of the neck of the femur in children. J Bone Joint Surg Br 44-B:528–542
Ratliff AH (1974) Fractures of the neck of the femur in children. Orthop Clin North Am 5:903–924
Kujat R, Suren EG, Rogge D, Tscherne H (1984) Femoral neck fractures during the growth period. Treatment principles, results, prognosis (in German). Chirurg 55:43–48
Hahn MP, Ostermann PA, Richter D, David A (1995) Classification, therapy and complications of pediatric femoral neck fractures (in German). Zentralbl Chir 120:832–840
Davison BL, Weinstein SL (1992) Hip fractures in children: a long-term follow-up study. J Pediatr Orthop 12:355–358
von Laer L (2001) Frakturen und Dislokationen im Wachstumsalter. Thieme, Stuttgart
Delbet MP (1909) Fractures du col de fémur. Bull Mem Soc Chir 35:387–389
Colonna PC (1928) Fracture of the neck of the femur in childhood: a report of six cases. Ann Surg 88:902–907
WK RCA, Beaty JH (1996) Fractures in children. Lippincott-Raven, Philadelphia
Nolan PC, Dilworth R (1996) Irreducible femoral neck fracture in a child. Injury 27:675–676
Hughes LO, Beaty JH (1994) Fractures of the head and neck of the femur in children. J Bone Joint Surg Am 76:283–292
Kay SP, Hall JE (1971) Fracture of the femoral neck in children and its complications. Clin Orthop Relat Res 80:53–71
Nagi ON, Dhillon MS, Gill SS (1992) Fibular osteosynthesis for delayed type II and type III femoral neck fractures in children. J Orthop Trauma 6:306–313
Wiedmann H, Parsch K (1990) Femoral neck fracture in children (in German). Z Orthop Ihre Grenzgeb 128:418–421
Quinlan WR, Brady PG, Regan BF (1980) Fracture of the neck of the femur in childhood. Injury 11:242–247
Ng GP, Cole WG (1996) Effect of early hip decompression on the frequency of avascular necrosis in children with fractures of the neck of the femur. Injury 27:419–421
Rehli V, Slongo T, Gerber C (1993) Fractures near the femur head in children and adolescents (in German). Helv Chir Acta 59:547–552
Leung PC, Lam SF (1986) Long-term follow-up of children with femoral neck fractures. J Bone Joint Surg Br 68:537–540
Hajdu S (1994) Growth disturbances following artificial injury of the growth plate in rabbits. Master Thesis, Department of Trauma Surgery, Medical University of Vienna, Vienna
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hajdu, S., Oberleitner, G., Schwendenwein, E. et al. Fractures of the head and neck of the femur in children: an outcome study. International Orthopaedics (SICOT) 35, 883–888 (2011). https://doi.org/10.1007/s00264-010-1039-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1039-z