Abstract
The aim of this study was to present the clinical and functional results of revision surgery after failed hip endoprostheses using the Modular Universal Tumour And Revision System (MUTARS®). Functional results of the hip endoprostheses were recorded by applying the Harris hip score. The extent of the presurgical radiological bone defect was measured according to the classification system of the German orthopaedic association (DGOOC). Indications for revision surgery on 45 patients (21 female, 24 male) were aseptic loosening (19 patients), infection (16 patients), or periprosthetic fracture (Vancouver classification B2, B3 and C, in nine patients). Revision surgery was performed after 8.6 years on average (min. 0.6; max. 14.25 years). Large defects of the proximal femur (80% medial or lateral diaphysis; 20% meta-diaphysis according to DGOOC classification) were adequately reconstructed. The average follow-up was 38.6 months. Complications occurred in eight patients: one luxation, two aseptic loosenings, and five reinfections were diagnosed. The Harris hip score (presurgical 30; postsurgical 78) showed significant improvement after revision surgery. Regarding the extent of the patients’ bone defects, good functional results were achieved. The comparatively low number of luxations and loosenings is due to the high modularity of the prosthesis with arbitrary antetorsion in the hip joint. However, high reinfection rates in mega-implants still constitute a problem and should be the subject of further studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The increasing number of primary endoprosthetic implantations inevitably leads to an increasing number of revision operations, which mainly become necessary after infection, loosening or periprosthetic fractures. Septic and aseptic loosening, periprosthetic fractures or resorption in areas of the non weight-bearing bone (stress shielding) can cause considerable osseous defects [1, 2].
It is possible to revise smaller defects with conventional primary prosthetic designs. Larger metadiaphyseal bone defects often preclude the safe use of a primary cementless endoprosthesis [3–7].
In recent years, good clinical results have been documented for non-modular and custom prostheses. The main disadvantage of these is the lack of intraoperative possibilities for variation of the length and angle of the femoral neck and the antetorsion angle [6, 8, 9].
The aim of this study was to examine the reconstruction results obtainable using the Modular Universal Tumour and Revision System (MUTARS®; Implantcast GmbH, Buxtehude, Germany) in endoprosthetic revision surgery of the hip joint with large osseous defects.
Methods
The revision system presented in this study has been developed in co-operation with the Orthopaedic Department of the University Hospital in Muenster, Germany. The system features great modularity since each component can be combined with one another—if necessary to a total femur replacement with reconstruction of the adjacent joints. This is made possible by an adapter which connects the revision system with the modular tumour prosthesis system. The hexagonal revision stems, which are shaped with anatomical anterior curvature, are manufactured with a hydroxyiapatite coating for cement-free implantation. If a safe cement-free fixation is not possible, uncoated CoCrMo stems can be used. A variety of stems with different lengths and diameters allow for an individual application of the intramedullary fixation (see Fig. 1).
The preoperative planning of the shaft design was made with computer-assistance and with the help of digitalised radiographs with a two-level scale.
Due to the inbuilt spur gearing with steps of 5°, rotation and antetorsion can be selected even after implantation of the shaft. The shaft can be extended in 1-cm steps according to need (see Fig. 1). A variety of components are also available for metaphyseal defects. Therefore, a nearly individual “fill and fit” situation can be created. It is possible to combine the system with a MUTARS® connection tube to prevent luxation and for reattachment of soft tissue with larger defects in the area of the greater and lesser trochanter [10, 11].
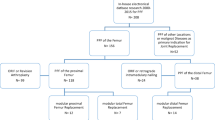
Between August 1998 and June 2003, 45 patients (24 male, 21 female) with an average age of 62.2 years (min. 31.3, max. 81) underwent hip prosthesis revision surgery. The mean follow-up was 38.5 months (min. 12.1, max. 69.9). A variety of indications precipitated the primary surgery. Revision surgery was performed after an average of 8.6 years (min. 0.6, max. 14.25) with indications being either an aseptic loosening (n = 19), a periprosthetic infection (n = 16) or a periprosthetic fracture (Vancouver classification type B2 [n = 3], B3 [n = 4], C [n = 2]). All infections were late infections after primary implantation and were treated with a two-step approach (explantation of the prosthesis, implantation of a replacement of antibiotic bone cement, thread and titanium rods comparable to the technique described by Kent et al. [12]; reimplantation after the infection has healed).
The MUTARS®-RS shaft was used in two unusual cases: One loosening of the saddle prosthesis after a pelvic tumour resection and one fibrous dysplasia with correction of an axis displacement of the proximal femur.
The standard revision system was used in 43 cases. Operative findings such as an unexpected size or site of defect led to two cases requiring additional components (MUTARS® Intramedullary Femoral Replacement prosthesis with a loosened knee prosthesis on the same side: n = 1, MUTARS® total femoral replacement with a large distal proximal femoral defect after explantation of the primary prosthesis: n = 1).
Systematic defect classification followed the recommendations of the German Orthopaedic Society (DGOOC) [1]; for periprosthetic fractures the Vancouver classification was used [13].
Clinical and functional results were recorded with pre-and postoperative examinations and documented according to the Harris hip score [14].
The postoperative healing process and the time needed to achieve full weight bearing capacity, was also documented.
Results
The patients examined mainly suffered from large bone defects. According to DGOOC-classification the following defects were recorded: 80% large medial or lateral diaphyseal defects (type 4 and 5), 20% large meta-diaphyseal defects (types 2 and 3) (see Table 1).
It was possible in every case to achieve stable reconstruction without the use of an allograft (see Fig. 2). An intraoperative change of approach because of unexpectedly bad bone quality was possible without complications in two cases (one MUTARS® Intramedullary Femoral Replacement, one total femur replacement). In both cases, a large distal defect became apparent after the removal of the primary prosthesis, requiring the use of a special prosthesis. Physiotherapy treatment was possible immediately after surgery.
Patients with a cementless fixation (n = 42), undertook progressive weight bearing starting at 10 kg for six weeks with successive increase of the load. Patients with a cemented shaft (n = 3) were mobilised with standard therapy.
In all cases, revision surgery led to a significant subjective as well as objective improvement. The Harris hip score improved from a preoperative average of 30 points (min. 8, max. 63) to a postoperative average of 78 points (min. 57, max. 95). It must be stated, though, that the validity of the preoperatively estimated scores from patients with fractures has to be judged critically.
Of all the patients, two (4%) aseptic loosenings of the shaft were recorded. This required the exchange of a shaft with a larger diameter. Five patients (11%) suffered from an infection of the shaft bearing, which required two-step revision surgery.
A luxation of the prosthesis after revision of total hip arthroplasty (RTHA) was recorded in one case (2%). Here, the primarily cemented acetabular cup was retained and a possible tendency to luxation was compensated by a correction of the antetorsion angle with the help of the revision prosthesis. Neither during the clinical nor during the radiological follow-up examinations was a malfunction of the implant found. Postoperative deep vein thrombosis was not recorded with those patients who were treated with low molecular heparin (weight-adapted, once per day s.c.).
Discussion
Reconstruction after defects resulting from failure of the prosthesis constitutes a problem for hip arthroplasty, especially in the light of the increasing number of implantations. The frequency of surgical procedures in which the prosthesis is exchanged, is still relatively low in the first five to ten years after a total arthroplasty. However, the absolute number of cases is high enough to incur considerable costs. It is all the more important to be able to use a safe and cost-efficient surgical procedure for all kinds of defects bearing in mind the patient and his psychosocial situation. The quick and safe mobilisation of the—usually older—patient should be the highest priority, especially when the patient has a high comorbidity rate.
The use of allogenic cortical or cancellous bone material in revision surgery has already been discussed [15–18].
A potential risk of infection remains with the use of an allograft augmentation in spite of radiation. Autologous implants are often not available in adequate quantity and quality. Composite constructions (such as cemented allograft prostheses) initially provide good results [19]. However, re-revision rates of up to 25% due to aseptic loosening, failure or infection of the prosthesis and dislocations are documented [9, 15–17].
If the cortical bone has been preserved or can be reconstructed with small, malleable material, the Exeter technique provides an interesting alternative in surgery. Here, a shaft is cemented into previously created cancellous allograft bedding. In up to 87%, a remodelling of the allograft with an osseointegration into the trabecular bone can be verified [20]. The clinical results reported were good, and the viability of the implant was 92% after 10.5 years. Nevertheless, the complication rate could be up to 40.7% with re-revision described in 16% and more [21].
If allogenic material is not used in revision surgery and there are large metaphyseal defects of the diaphyseal bone, a solid fixation of the implant is vital [3–8]. If possible, a cementless fixation should be striven for. Clinical results that have been recorded so far are promising for the cementless revision (revision rates of 20% cemented vs. 7% cementless) [3, 7, 22, 23].
Older patients constitute an exception because less biomechanical stress on the revision prosthesis can be expected [24]. The survival rate of cemented prostheses with a long shaft in patients with an average age of 62.3 years was rather short after initially good functional results (54% after 12 years) according to Diekerhof et al. [25]. However, recent studies have shown better results [26]. There is a significant link between the patient’s age at the time of the surgery and the long-term clinical results. The older the patient, the less the pain at the time of the follow-up. The ten-year survival rate of the whole group was 85.29% ±2.69%. In comparison with the survival rates of cemented stems found in Scandinavian hip prosthesis registries, the modular shaft examined in our study has an equally good or even better survival rate. This means that, depending on the age of the patient and quality of the bone material of the femur, the use of a cemented prosthesis is still an option.
The use of monobloc revision prostheses makes it impossible to deviate intraoperatively from the preoperative plan. Bone defects or, for example, a rotation error of the shaft implantation that are discovered during surgery cannot be corrected during that same operation. Here, the advantage of a modular system, where rotation can be adjusted accordingly and the use of another type of shaft, if needed, is possible, is clear.
In the patient group presented in this study, exercise-stable reconstruction was possible in all cases without the use of allogenic bone material (cementless n = 41, cemented n = 3, total femur replacement n = 1). The intraoperative change of the planned prosthesis because of unexpectedly bad bone quality was possible without any complications in two cases (through whole prosthesis and total femur replacement respectively).
The comparatively bad clinical functional scores of the patient group [3, 8, 17, 27] most likely result from the size of the reconstructed bone defects (80% class 4 and 5 of the DGOOC classification system). However, in all cases the preoperative functional result could be improved. The rather low revision rate considering the extent of the bone defects can be attributed to the routinely CAD-supported precise preoperative planning. Thus, the biomechanical conditions even with large defects in the region of the greater trochanter (as often seen after tumour surgery) could be restored completely [10]. These luxation rates are remarkable if compared to the rates ranging from 4% up to 30% presented in previous studies [9, 16, 28].
The cause of the relatively high infection rates (n = 5, 11%), compared to other studies and in spite of an appropriate two-step approach, probably lies in the patient cohort itself. The indication for revision was given in 16 cases after a septic loosening of the prosthesis. Reinfection could be brought under control after another two-step change of the prosthesis. A secondary hip disarticulation because of a reinfection was not necessary in our study.
The cause of aseptic loosenings of cemented as well as cementless endoprostheses remains unexplained despite numerous studies and surveys [4, 5, 17, 29]. The loosening rate in our study coincides with results found in studies of other types of megaprostheses [3–5, 8, 17, 27, 30]. However, a certain “negative-selection” in this cohort is noticeable. Furthermore, the prosthesis proved suitable in cases of periprothethic fractures. The distal interlocking with the aid of a screw provided ample rotational stability even in previously loosened primary implants or insufficient bone quality (type B2: n = 3; type B3: n = 4). However, one should refrain from interlocking “prophylactically” in order not to weaken the diapyhseal bone unnecessarily. Both loosenings observed here resulted from an insufficient diameter of the stem originally chosen. The interlocking screws that were used in one case could not cope with the forces involved. However, this study shows that with a proper pressfit a satisfactory cementless fixation of the prosthesis is possible due to the shaft design.
Conclusion
Even with extensive bone defects, the use of this modular revision system could achieve high stability and good functional results. The low loosening and luxation rates were due to the modularity of the system, enabling a “fill and fit” approach including with metaphyseal defects. Furthermore, the freely selectable antetorsion after implantation of the shaft, the consequent use of the MUTARS© connection tube with large defects in the region of the trochanter and finally, the precise preoperative planning further contribute to the good results presented in this study.
The results are promising but need to be validated by further studies with a larger patient cohort and prolonged follow-up. The high (re-)infection rates of allogenic material remain an important issue in revision surgery and should be the subject of further studies.
References
Bettin D, Katthagen BD (1997) The German Society of Orthopedics and Traumatology classification of bone defects in total hip endoprostheses revision operations. Z Orthop Ihre Grenzgeb 135:281–284
Ulrich SD, Seyler TM, Bennett D, Delanois RE, Saleh KJ, Thongtrangan I, Kuskowski M, Cheng EY, Sharkey PF, Parvizi J, Stiehl JB, Mont MA (2008) Total hip arthroplasties: what are the reasons for revision?. Int Orthop 32:597–604. doi:10.1007/s00264-007-0364-3
Wirtz DC, Heller KD, Holzwarth U, Siebert C, Pitto RP, Zeiler G, Blencke BA, Forst R (2000) A modular femoral implant for uncemented stem revision in THR. Int Orthop 24:134–138
Wirtz DC, Niethard FU (1997) Etiology, diagnosis and therapy of aseptic hip prosthesis loosening—a status assessment. Z Orthop Ihre Grenzgeb 135:270–280
Malchau H, Herberts P, Ahnfelt L (1993) Prognosis of total hip replacement in Sweden. Follow-up of 92,675 operations performed 1978–1990. Acta Orthop Scand 64:497–506
Engh CA, Glassman AH, Griffin WL, Mayer JG (1988) Results of cementless revision for failed cemented total hip arthroplasty. Clin Orthop:91–110
Hedley AK, Gruen TA, Ruoff DP (1988) Revision of failed total hip arthroplasties with uncemented porous-coated anatomic components. Clin Orthop 235:75–90
Wagner H, Wagner M (1993) Femur revision prosthesis. Z Orthop Ihre Grenzgeb 131:574–577
Gustilo RB, Pasternak HS (1988) Revision total hip arthroplasty with titanium ingrowth prosthesis and bone grafting for failed cemented femoral component loosening. Clin Orthop:111–119
Gosheger G, Hillmann A, Lindner N, Rodl R, Hoffmann C, Burger H, Winkelmann W (2001) Soft tissue reconstruction of megaprostheses using a trevira tube. Clin Orthop 235:264–271
Gosheger G, Winkelmann W (2000) Mutars—a modular tumor and revision system. Experiences at the Munster Tumor Center. Orthopade 29(Suppl 1):S54–S55
Kent M, Rachha R, Sood M (2009) A technique for the fabrication of a reinforced moulded articulating cement spacer in two-stage revision total hip arthroplasty. Int Orthop. doi:10.1007/s00264-009-0847-5
Brady OH, Garbuz DS, Masri BA, Duncan CP (1999) Classification of the hip. Orthop Clin North Am 30:215–220
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755
Chandler H, Clark J, Murphy S, McCarthy J, Penenberg B, Danylchuk K, Roehr B (1994) Reconstruction of major segmental loss of the proximal femur in revision total hip arthroplasty. Clin Orthop 298:67–74
Malkani AL, Sim FH, Chao EY (1993) Custom-made segmental femoral replacement prosthesis in revision total hip arthroplasty. Orthop Clin North Am 24:727–733
Blackley HR, Davis AM, Hutchison CR, Gross AE (2001) Proximal femoral allografts for reconstruction of bone stock in revision arthroplasty of the hip. A nine to fifteen-year follow-up. J Bone Joint Surg Am 83-A:346–354
Baba T, Shitoto K (2009) Revision of total hip arthroplasty using the Kerboull and KT plates. Int Orthop. doi:10.1007/s00264-009-0789-y
Vastel L, Lemoine CT, Kerboull M, Courpied JP (2007) Structural allograft and cemented long-stem prosthesis for complex revision hip arthroplasty: use of a trochanteric claw plate improves final hip function. Int Orthop 31:851–857. doi:10.1007/s00264-006-0275-8
Wraighte PJ, Howard PW (2008) Femoral impaction bone allografting with an Exeter cemented collarless, polished, tapered stem in revision hip replacement: a mean follow-up of 10.5 years. J Bone Joint Surg Br 90:1000–1004
Frances A, Moro E, Cebrian JL, Marco F, Garcia-Lopez A, Serfaty D, Lopez-Duran L (2007) Reconstruction of bone defects with impacted allograft in femoral stem revision surgery. Int Orthop 31:457–464. doi:10.1007/s00264-006-0211-y
Schmale GA, Lachiewicz PF, Kelley SS (2000) Early failure of revision total hip arthroplasty with cemented precoated femoral components: comparison with uncemented components at 2 to 8 years. J Arthroplasty 15:718–729
Yoo JJ, Kwon YS, Koo KH, Yoon KS, Kim YM, Kim HJ (2009) One-stage cementless revision arthroplasty for infected hip replacements. Int Orthop 33:1195–1201. doi:10.1007/s00264-008-0640-x
Ogino D, Kawaji H, Konttinen L, Lehto M, Rantanen P, Malmivaara A, Konttinen L, Salo J (2008) Total hip replacement in patients eighty years of age and older. J Bone Joint Surg Am 90:1884–1890
Diekerhof CH, Barnaart LF, Rozing PM (2000) Long-term clinical results of cemented revision of primary cemented total hip arthroplasties. Acta Orthop Belg 66:376–381
Stöckl B, Kulhanek A, Steindl V, Mayr E, Krismer M (2007) Langzeitüberleben der zementierten Langschaftprothese LINK SP II nach Revisionsoperationen. 29 Jahrestagung der Österreichischen Gesellschaft für Orthopädie und Orthopädische Chirurgie, Wien
Tanzer M, Chan S, Brooks CE, Bobyn JD (2001) Primary cementless total hip arthroplasty using a modular femoral component: a minimum 6-year follow-up. J Arthroplasty 16:64–70
Crawford SA, Siney PD, Wroblewski BM (2000) Revision of failed total hip arthroplasty with a proximal femoral modular cemented stem. J Bone Joint Surg Br 82:684–688
Kavanagh BF, Ilstrup DM, Fitzgerald RH Jr (1985) Revision total hip arthroplasty. J Bone Joint Surg Am 67:517–526
Cameron HU (2002) The long-term success of modular proximal fixation stems in revision total hip arthroplasty. J Arthroplasty 17:138–141
Author information
Authors and Affiliations
Corresponding author
Additional information
Carsten Gebert and Martin Wessling contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Gebert, C., Wessling, M., Götze, C. et al. The Modular Universal Tumour And Revision System (MUTARS®) in endoprosthetic revision surgery. International Orthopaedics (SICOT) 34, 1261–1265 (2010). https://doi.org/10.1007/s00264-010-1007-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1007-7