Abstract
The clinical and radiographic results of 174 female and 86 male Innex (Zimmer, Warsaw, Indiana) mobile bearing total knee arthroplasty systems (245 patients) were evaluated, with particular emphasis on gender-related differences at five-year follow-up. Pre-operative Knee Society (KS) function and total scores were lower in women than in men. All KS scores showed a significant improvement at follow-up, but women still obtained lower KS function scores than men. Self-reported function was significantly better for male knees. No gender differences were observed for component alignment, while the occurrence of radiolucent lines, endosteal cavitations, and wear was significantly greater in male knees. Male Innex mobile bearing knees exhibited better clinical function and satisfaction than their female peers at five-year follow-up, despite inferior radiographic findings and higher revision rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
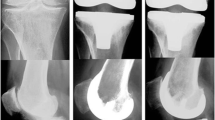
The two main Innex (Zimmer, Warsaw, Indiana) mobile bearing total knee arthroplasty (TKA) implants are the cruciate retaining, which is designed for posterior cruciate ligament retention and anterior cruciate ligament sacrifice, and the ultra congruent only rotating (posterior cruciate ligament sacrifice or retention), whose platform has a metal pin fitted into the tibial component (Fig. 1) allowing for free rotation without translation. Clinical experience demonstrates that the ultra congruent design offers similar stability to the posterior stabilised design, with the advantages of less bone removal and fewer instrumentation steps [8]. However, even though the Innex mobile bearing system is currently one of the most popular devices by European surgeons [8], limited data exists regarding knee function in male and female TKA patients who have received this implant.
The purpose of this study was to evaluate the mid-term (five years) results of 260 Innex mobile bearing prostheses implanted in our clinic (primary TKA), mainly in osteoarthritic knees. Particular attention was paid to possible gender-related differences in clinical and radiographic outcomes.
Materials and methods
In 2002, 411 Innex systems were consecutively implanted in 383 patients. During the 2002–2007 period, 23 patients (25 knees) died from causes unrelated to knee surgery, 17 patients (17 knees) moved away and were lost for follow-up but their original prosthesis was in place at five years post surgery (as verified by a telephone call), 97 knees (86 patients) had only a short-term (less than 2.5 years) follow-up but their original prosthesis was in place at five years post surgery (as verified by a telephone call), and 12 knees (2.9%) required revision surgery. The remaining 260 knees in 162 female and 83 male patients (Table 1), for which both pre-surgery and five-year follow-up results were available, were therefore considered for this study. Preoperative data were collected within six weeks prior to the TKA. The mean ± standard deviation (SD) follow-up was 5.10 ± 0.34 and 5.08 ± 0.26 years for female and male knees, respectively.
Surgical procedure
All knees received a mobile bearing prosthesis (Innex ultra congruent only rotating; Fig. 2) using the standard medial parapatellar approach. Only seven knees (2.7%) required patella replacement. Operations were performed by 12 different surgeons (62% by two head surgeons, 27% by four assistant surgeons, and 11% by six junior surgeons), with standardised Zimmer instrumentation. The procedures were performed under tourniquet control, which was released once implantation was complete. The routine pain management was via epidural catheter. In selected cases, the femoral nerve catheter or single-injection sciatic nerve block were used. The overall duration of the surgical procedure ranged between 70 and 80 minutes.
After skin incision, the correct rotation positioning of the tibial alignment was defined and the tibia segment guide was fixed proximally. The angle for the posterior slope of the tibial cut was adjusted to the physiological inclination of the tibial plateau in accordance with preoperative planning. The tibial resection was performed 10 mm below the highest point of the intact compartment unless cartilage defects dictated a different level of resection. In this case, the femur was accessed from the front with the knee flexed at 90°. The intercondylar insertion point for the femoral intercondylar drill guide was placed slightly medial of the mid-line, as indicated by preoperative frontal and sagittal X-rays of the femur (long leg X-rays). The intramedullary space was opened with an 8-mm drill, which was aligned with the anatomical axis of the femur. The size of the femoral component in both anteroposterior and mediolateral directions was then determined. The dimension in the mediolateral direction was checked with the femoral gauge. The anteroposterior resection was done by determining the femoral angle bushing according to the valgus angle. The setting for femoral rotation and ligament tension came next. The balancer was inserted into the anteroposterior cutting guide and then stretched to the smallest overall tibial height of 10 mm. The desired external rotation of the anteroposterior cutting guide (approximately 3°) was usually obtained automatically by equalising tension of the medial and lateral soft tissues by cranking up the balancer. The femoral rotation was checked via the epicondylar axis and the Whiteside line. Posterior osteophytes on the femoral condyles were removed and, when necessary, the posterior capsule was released before making the distal femoral cut. This procedure was especially important in the presence of a severe flexion contracture. The leg was then extended to assess the alignment. The alignment guide followed the mechanical axis of the limb, and was aligned with the femoral head centre. The femoral and tibial spacer plates were then put together to form the spacer gauge. After extending the knee, the level of the distal resection (extension gap) was checked with the balancer. It was verified that extension and flexion gaps were of identical height and mediolateral ligament tension was balanced. The distal femoral cut was then made. The mediolateral positioning was facilitated as the width of the chamfer guide exactly matched the width of the femoral component. Both the anteroposterior and mediolateral dimensions of the chamfer guide corresponded to the final implant size. The size of the tibial template was selected for its best coverage of the proximal tibia. The appropriate mobile bearing was attached to the tibial template, which could be fixed for best coverage without having to preset rotation. Subsequently, flexion, extension and stability of the knee joint with the trial components were checked. Finally, the same procedure as for the trial components was used for implanting the definitive prosthetic components. The femoral component was fully seated to obtain a good press fit. Femoral implants (5 sizes), tibial implants (10 sizes) and meniscal bearings (7 sizes) were chosen.
Outcomes
We used the international documentation and evaluation system [22, 27] forms [18], which allow standardised documentation of clinical and radiological information according to the American Knee Society [6, 17]. The forms collect a set of core information corresponding to the patient medical record. The independent evaluators, which included assistant and junior surgeons, were trained by one of the authors (T.G.) and used a standardised method of collecting the physical examination data according to a written protocol. The protocol ensured that all patients were positioned alike and that the same techniques were used for the examination.
Physical examination data (knee range of motion, stability, and alignment; 50 points) and self-reported pain during walking and stair climbing (50 points) were used to calculate the Knee Society (KS) knee score [17]. The KS questionnaire also included items on functional ability (walking distance, stair climbing ability, and walking aids), which allowed calculation of the KS function score (100 points). The KS scores were transformed to a 0 to 100-point scale for each domain (with 100 points being the best score): pain, knee, function, and total (i.e., mean of KS knee and function scores). At the time of follow-up, patients were also asked to self-evaluate their global function using one of these four responses: excellent, good, fair, or poor.
Radiographic evaluation was performed for each patient at follow-up visits using the methodology described by the American Knee Society [6]. Briefly, evidence of radiolucencies, endosteal cavitations, subsidence of the prosthetic component and wear were checked. The alignment of the femoral and tibial components was measured on standing anteroposterior and mediolateral radiographs and the following angles were calculated:
-
Angle α (mediolateral alignment of the femoral component) using the following categories: 83–86°, 87–89°, 91–93°, 94–96°, 97–99°, and 100–102°
-
Angle β (mediolateral alignment of the tibial component) using the following categories: <85°, 85–90°, 91–95°, and 96–100°
-
Angle γ (anteroposterior alignment of the femoral component) using the following categories: <80°, 80–85°, 86–90°, 91–95°, and >95°
-
Angle σ (anteroposterior alignment of the tibial component) using the following categories: <80°, 80–85°, 86–90°, 91–95°, and >95°
Statistical analyses
The dependent variables were KS scores (pain, knee, function, total), knee range of motion (ROM), self-reported function, and radiographic data. Non-parametric tests were used because KS scores were non-normally distributed, as verified by a Shapiro-Wilk test. Therefore, both pre-surgery and follow-up differences in KS scores and ROM between male and female knees were studied with a Mann-Whitney U test. Changes in KS scores and knee ROM between baseline and follow-up were investigated using the Wilcoxon test. In order to check for gender differences in self-reported function and radiographic data (categorical variables), independent-sample Chi square statistics were used [14], followed by z-ratio calculations to investigate the significance of the difference between two independent proportions. Significance was set at P < 0.05.
Results
Age, body mass index, and diagnoses were comparable between women and men (Table 1). Preoperative KS function and total scores were lower in female than in male knees (P < 0.05), while KS pain and knee scores, and ROM did not differ significantly between genders (Table 2). All KS scores and ROM showed an improvement at follow-up (P < 0.05) for both male and female knees (Table 2). At follow-up, only KS function score showed a significant gender-related difference, with female knees exhibiting lower scores than their male counterparts (P < 0.05). Self-reported function was, for the majority of the patients (91.2%), “good” to “excellent” (Table 2). Interestingly, the proportion of males reporting “excellent” function was greater compared to females, and vice versa for “good” function (P < 0.01).
No gender differences were observed for radiographic angles α, β, γ, and σ (component alignment) at follow-up (Table 3), although the occurrence of radiolucencies, endosteal cavitations and wear was greater in male than in female knees (P < 0.001; z-ratio). Radiolucent lines were present in four female femurs, one patella, and seven tibias (largest thickness < 2 mm). Radiolucencies were observed in six male femurs, two patellas, and 20 tibias (largest thickness >2 mm). Endosteal cavitations were observed in only one man (tibia, medial), while wear was observed in one female (<1 mm) and five male (up to >2 mm) tibial components. No knees were found to have subsidence of the prosthetic component of the tibial or the femoral components by KS criteria.
A total of six female (2.3%) and six male (4.1%) knees required surgical revision, with four total (three for early infections and one for overstuffing) and eight partial revisions (six for instability, one for arthrofibrosis and one for anterior knee pain). The three infections (one female, two males), which occurred between one and four months post-surgery, were all treated with a two-stage revision. Overstuffing was treated with a downsized TKA implant (legacy constrained condylar knee; Zimmer).
Discussion
Several interesting findings were observed in this mid-term follow-up study. Besides the satisfactory results associated with the Innex mobile bearing implant in terms of both clinical and radiographic outcomes, gender-related differences in (i) knee function, (ii) global satisfaction, (iii) radiographic findings and (iv) revision rate five years after TKA surgery require adequate discussion.
Follow-up KS scores of TKA patients with the Innex implant are similar (KS knee score) or higher (KS functional score) than those reported in previous mid-term studies [2, 5, 13, 15, 16, 24, 26], in which different implants were used (e.g. press fit condylar Sigma, Duracon, Insall-Burstein II, Optetrak, AGC, Rotaglide). In the same way, our ROM data (116.4°) are similar to those recently reported after five-year posterior cruciate retaining TKA surgery (114.9°) [24]. According to the claims of Innex manufacturers, we were satisfied with the reasonable instrument trays, which facilitated the interaction between the surgeons and the theatre nurses, as well as the standardisation of Innex surgical procedures. This resulted in good implant positioning, as witnessed by the radiographic findings, and also in high levels of patient satisfaction at five-year follow-up (see below).
Significant gender differences were observed in KS scores both pre-operatively (KS function and total) and at follow-up (KS function), with female knees displaying lower scores than their male peers. These results are in agreement with the recent findings of Ritter et al. [24], who observed greater preoperative and postoperative (six months to five years) KS function scores in TKA men than in women. They also demonstrated a greater postoperative improvement in KS function score in men, and attributed such results to the stair component of the KS function score, while in our study the postoperative improvement was not significantly affected by gender. Postoperative gender-related differences in KS function and total scores were also observed at an average follow-up of ten years [21], with female knees demonstrating poorer outcome scores, and also smaller improvements from preoperative to ten-year scores compared to male knees. Taken as a whole, these results corroborate the assumption of Lim et al. [20], who noted that patients with lower preoperative scores tend to have lower postoperative scores, and vice versa. Our KS score findings also confirm that women receive treatment later in the course of their disease because they are likely to delay surgery, are less likely to be referred, or perhaps are referred after a longer interval, to orthopaedic surgeons for consideration for arthroplasty [10].
Self-reported global function at follow-up (i.e. a sort of satisfaction score) was also influenced by gender, with a greater proportion of men reporting “excellent” function than women, and vice versa for “good” function. Robertsson et al. [25], using a simplified, subjective, patient-reported satisfaction survey with a mean six-year follow-up, reported 55% of men were very satisfied after their TKA compared with 50% of women. Although satisfaction has been found to be significantly related to pain, and only to a lower degree to physical function [1, 12, 25], in our study no gender differences were observed in KS pain score both preoperatively and postoperatively, so that function scores only appear to be linked to postoperative global satisfaction. In this study, 91% of both men and women declared good or excellent function at five-year follow-up (i.e. satisfaction), which is slightly higher than the percentage of satisfied patients reported by others (from 81 to 89%) [1, 9, 12, 25], even when the diagnoses, patients characteristics, and follow-up periods were quite heterogeneous compared to our study.
Contrary to knee function scores, the proportion of radiolucencies, endosteal cavitations and wear was significantly higher in male than in female knees, although the alignment of tibial and femoral implants was comparable between genders. Interestingly, MacDonald et al. [21] observed that men had more revisions for polyethylene wear than women (37% of male revisions, 26% of female revisions) at ten-year follow-up. As a speculation, men with TKA, who have greater expectations than their female peers [19], probably undertake higher levels of physical activity [4] and/or higher impact activities than TKA women (including non recommended activities), and this would inevitably increase the risk of wear [4] which in turn would affect the rate of TKA revision. Indelli et al. [16] observed 1-mm-thick radiolucent lines in 30% of tibial components five to nine years after TKA (Insall-Burstein II implant), and Robertsson et al. [25] observed radiolucencies in 35 of 60 knees (42%) five years after TKA (Optetrak implant), which is considerably more than in our study (approximately 15%).
We observed a higher TKA revision rate for male than for female knees, which is compatible with the findings of MacDonald et al. [21]. These authors reported significant differences in revision rate between men (10.2%) and women (8%) at an average follow-up of ten years. More importantly, the current revision rate percentages are very similar to those observed in the Australian Joint Registry [3], reporting on more than 130,000 primary TKAs with a five-year follow-up, for both men (4% vs. 4.1% in our study) and women (3.3% vs. 2.3%, respectively). In contrast, no gender-based differences in revision rates were observed in the 36,000 knees in the Swedish Arthroplasty Registry [11]. Interestingly, the rate of implant survival in TKA women has been found to be significantly greater than in men [7, 23], both at five-year (93 vs. 89%) and ten-year follow-up (83 vs. 76%). In this study, implant survival was 93.5% for male and 96.7% for female knees (95.6% overall) five years after TKA surgery.
In conclusion, our results indicate that male Innex mobile bearing knees result in better clinical function and satisfaction than their female peers at five-year follow-up, despite inferior radiographic findings and higher revision rates. We therefore suggest that the gender factor should be adequately weighed in future TKA studies.
References
Anderson JG, Wixson RL, Tsai D et al (1996) Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty 11:831–840
Asif S, Choon DSK (2005) Midterm results of cemented press fit condylar Sigma total knee arthroplasty system. J Orthop Surg 13:280–284
Australian Orthopaedic Association Joint Replacement Registry (2007) 2007 annual report. Available at: http://www.dmac.adelaide.edu.au/aoanjrr/. Accessed 8 September 2009
Bauman S, Williams D, Petruccelli D et al (2007) Physical activity after total joint replacement: a cross-sectional survey. Clin J Sports Med 17:104–108
Chana R, Shenava Y, Nicholl AP et al (2008) Five- to 8-year results of the uncemented Duracon total knee arthoplasty system. J Arthroplasty 23:677–682
Edwald FC (1989) The knee society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Greene KA (2007) Gender-specific design in total knee arthroplasty. J Arthroplasty 22:27–31
Gyssler BG (2004) Developing a mobile bearing knee prosthesis. In: Munzinger UK, Boldt J, Keblish P (eds) Primary knee arthroplasty. Springer, Berlin, pp 18–24
Hawker G, Wright J, Coyte P et al (1998) Health-related quality of life after knee replacement. J Bone Joint Surg Am 80:163–173
Hawker GA, Wright JG, Coyte PC et al (2000) Differences between men and women in the rate of use of hip and knee arthroplasty. N Engl J Med 342:1016–1022
Harrysson OLA, Robertsson O, Nayfesh JF (2004) Higher cumulative revision rate of knee arthroplasties in younger patients with osteoarthritis? Clin Orthop Relat Res 421:162–168
Heck DA, Robinson RL, Partridge CM et al (1998) Patient outcomes after knee replacement. Clin Orthop Relat Res 356:93–110
Horwitz MD, Awan S, Chatoo MB et al (2009) An 8- to 10-year review of the Rotaglide total knee replacement. Int Orthop 33:111–115
Huck SW (2004) Reading statistics and research. Pearson Education, Boston
Hudd A, Kunasingam K, Ricketts D et al (2009) A 5 to 8 year follow-up study of the Rotaglide mobile bearing total knee arthroplasty. Int Orthop 33:675–678
Indelli PF, Aglietti P, Buzzi R et al (2002) The Insall-Burstein II prosthesis. A 5- to 9-year follow-up study in osteoarthritic knees. J Arthroplasty 17:544–549
Insall JN, Dorr LD, Scott RD et al (1989) (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Institute for Evaluative Researchin Orthopaedic Surgery (IEFO) (2005) International documentation and evaluation system forms. Available at: http://www.siris-implant.ch/index.php?id=86&L=2. Accessed 8 September 2009
Karlson EW, Daltroy LH, Liang MH et al (1997) Gender differences in patient preference may underlie differential utilization of elective surgery. Am J Med 102:524–530
Lim JTK, Luscombe KL, Jones PW et al (2006) The effect of pre-operative symptom severity on functional outcome of total knee replacement-patients with the lowest pre-operative scores achieve the lowest marks. Knee 13:216–219
MacDonald SJ, Charron KD, Bourne RB et al (2008) Gender-specific total knee replacement. Prospectively collected clinical outcomes. Clin Orthop Relat Res 466:2612–2616
Paterson D (1993) International documentation and evaluation system. Clin Orthop Relat Res 290:306–307
Rand JA, Illstrup DM (1991) Survivorship analysis of total knee arthroplasty. Cumulative rates of survival of 9200 total knee arthroplasties. J Bone J Surg Am 73:397–409
Ritter MA, Wing JT, Berend ME et al (2008) The clinical effect of gender on outcome of total knee arthroplasty. J Arthroplasty 23:331–336
Robertsson O, Dunbar M, Pehrsson T et al (2000) Patient satisfaction after knee arthroplasty. A report on 27372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand 71:262–267
Robinson RP (2005) Five-year follow-up of primary Optetrak posterior stabilized total knee arthroplasties in osteoarthritis. J Arthroplasty 20:927–931
Röder C, Eggli S, EL-Kerdi A et al (2003) The international documentation and evaluation system (IDES)—10-years experience. Int Orthop 27:259–261
Acknowledgments
We are grateful to Ms. Kirsten Dobson for the English revision of this manuscript. The Schulthess Clinic received royalties from Zimmer in partial support of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Munzinger, U.K., Maffiuletti, N.A., Guggi, T. et al. Five-year results of the Innex total knee arthroplasty system. International Orthopaedics (SICOT) 34, 1159–1165 (2010). https://doi.org/10.1007/s00264-009-0887-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-009-0887-x