Abstract
The restoration of the hip centre of rotation in an anatomical position is considered to be relevant for total hip prosthesis survival. When the cup is implanted with a high centre of rotation, the lever arm of the abductor muscles is decreased, causing higher joint-reaction forces. Modular stems with varying lengths and geometries can be used to balance soft tissues, and ceramic bearing surfaces can be used to reduce the wear rate. Forty-four hip replacements performed with a high hip centre of rotation were matched with 44 performed with an anatomical centre of rotation. In all cases the preoperative diagnosis was dysplasia of the hip (DDH) and cementless modular neck prostheses with ceramic bearing surfaces were used. At nine years follow-up the mean Harris hip and WOMAC scores were not statistically different. All stems and cups were stable; the femoral offset was no different between the two groups (p = 0.4) as leg-length discrepancy (p = 0.25).
Résumé
On considère important pour la survie de la prothèse totale de la hanche que le centre de rotation soit rétabli en position anatomique. Quand le cotyle est implanté avec un centre de rotation haut, le bras de levier des muscles abducteurs se raccourcit et cause des majeures forces de réaction de l’articulation. Les tiges modulaires à longueurs et géométries variables peuvent être utilisés pour balancer les tissus mous, et les couples de frottement en céramique peuvent être utilisés pour réduire l’usure. Quarante-quatre prothèses totales de hanche réalisées avec un centre de rotation haut ont été confrontées avec 44 prothèses réalisées avec un centre de rotation anatomique. Tous les patients souffraient de dysplasie développementale de la hanche et on a utilisé une prothèse sans ciment avec un cou modulaire et avec les couples de frottement en céramique. Les résultats à 9 ans des scores Harris et WOMAC n’étaient pas statistiquement différents. Tous les cotyles et les tiges étaient stables; l’offset fémoral (p = 0,4) et la différence de longueur des membres inférieurs (p = 0,25) n’était pas différents dans les deux groupes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A high hip centre of rotation (HHCR) in total hip replacement (THR) is considered to be one of the most important factors for implant aseptic loosening because it causes inadequate soft tissue balancing and high joint reaction forces [7, 8, 13, 23]. The higher placement of the cup decreases the lever arm of the abductor muscles and increases the force of the abductor muscles needed to balance the pelvis during the gait cycle. This causes higher joint reaction force across the hip joint, with a high rate of polyethylene wear and high stresses on cup–bone interface [3, 4, 12, 14, 17, 21, 24]. Furthermore, HHCR may be responsible for a leg-length discrepancy, with limping and pain.
However, in critical cases of hip surgery such as developmental dysplasia of the hip (DDH), HHCR allows an easier surgical technique, by avoiding the use of bone grafts, cemented cups, osteotomies, or specialised implants [6].
Modular stems with varying lengths and geometries can be used to balance soft tissues and restore femoral off-set, the lever arm of abductor muscles, and leg length [18, 20]. In addition, a coupling with hard bearing surfaces (metal or ceramic) can be used to reduce the wear resulting from the high joint reaction forces. The aim of this study was to compare the four- to ten-year outcomes of a modular hip prosthesis with ceramic bearing surfaces implanted in an HHCR or in an anatomical centre of rotation (ACR).
Patients and methods
The centre of rotation (CR) was considered high when it was located at least 30 mm above the interteardrop line because of the hip load increase with a proximal displacement of the CR [3].
Between June 1995 and March 2004, 88 primary cementless prostheses were implanted in 67 patients by two senior hip surgeons. The only selection criterion was DDH as preoperative diagnosis. The first consecutive 44 prostheses (36 patients) implanted with a HHCR (group A) were compared with the first consecutive 44 prostheses (37 patients) implanted with an ACR (group B).
The average age of the patients at the time of surgery was 48.3 years in group A and 49 years in group B, with no statistically significant differences between the groups (p = 0.77). There were six male (16.7%) and 30 female (83.3%) patients in group A, and six male (16.2%) and 31 female (83.8%) patients in group B. Fifteen patients underwent bilateral operations, eight in group A (six female, two male) and seven in group B (six female, one male).
There were 22 right hips and 22 left hips in group A, and 21 right hips and 23 left hips in group B. All patients were preoperatively classified according to Crowe’s criteria [5]. There were seven type I, 16 type II, 13 type III, and eight type IV in group A, and 30 type I and 14 type II in group B (p < 0.0001) (Table 1).
All the operations were performed through a modified Watson-Jones approach with the patients in a supine position.
In all cases a cementless titanium anatomical stem with modular necks (Anca Fit, Wright Medical Technology, Arlington, Tennessee, USA), a ceramic 28 mm head with a ceramic liner (Biolox Forte, Ceramtec, Stuttgart, Germany), and a cementless titanium porus-coated cup (Anca Fit, Wright Medical Technology, Arlington, Tennessee) were used.
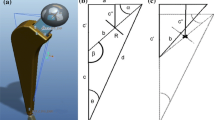
The Anca Fit stem was a titanium alloy (Ti-6A-14V) anatomical stem grit blasted and coated with 80 µm high crystalline plasma sprayed hydroxyapatite (HA) in the proximal third. In the proximal end there was a double-tapered housing for the modular necks. The modular necks were made of titanium (Ti-6A-14V) and had an oblong section and a conical design. The neck was taper-locked to the stem by an oblong conical profile taper, but the neck with the head was connected by a standard 12/14 Morse taper. Necks were available in two different lengths: short (28 mm) and long (38.5 mm). For both lengths there were six different models: straight, varus-valgus 8°, antiverted-retroverted of 8° and 15°, the combination of 6° of varus and 4.5° of retroversion for the left and the right side, and the lateralising-medialising. This wide choice of different geometries provided with the two neck lengths give a range of possible offsets of 13.5 mm (Fig. 1).
The ceramic modular heads were available in three sizes: short (−3.5 mm), medium (0 mm), and long (+3.5 mm), which, with the two necks, provided a range of possible lengthening of 17.5 mm.
The cup was a titanium alloy (Ti-6A-14V) hemispherical press fit cup, grit blasted and HA coated. Cup size varied from 46 mm to 60 mm in diameter.
All patients were reviewed clinically and radiographically at one, four, and 12 months and each year afterwards. Function was assessed by the Harris hip score (HHS) [11] and WOMAC [2]. At an average follow-up of nine years for both groups (range group A: 3.9–12.6 years; range group B: 6.8–10.6 years) a radiographic evaluation of implant stability was performed using Engh’s criteria [9]. Osteolysis was defined as a scalloped erosion exceeding 2 mm in diameter at the bone–prosthesis interface. A stem was considered to be in varus or valgus deviation if the angle was more than 5° from the neutral position. For the hemispherical press-fit cup, progressive widening of radiolucent lines more than 2 mm and migration of more than 5 mm or 5° were defined as loosening. Cup orientation (CO) was evaluated on an anteroposterior radiographic view of the hip; a cup was considered to be in a neutral position when the angle between the interteardrop line and the edge of the cup was between 40° and 50°. The differences between the two groups, in terms of femoral off-set, leg length, and abductor muscle lever arm, were also evaluated (Fig. 2).
CR center of rotation; Y CR height: the perpendicular distance from CR to the interteardrop line; X CR medialization: the perpendicular distance from CR to a line drawn perpendicularly to the interteardrop line and passing through the medial aspect of the teardrop; FO Femoral Off-set: the perpendicular distance between CR and a line drawn down the center of the femoral shaft; AM Abductor muscles lever arm: the perpendicular distance between CR and a line drawn from the anterior superior iliac spine and tangent to the great trochanter; L Leg-length: the perpendicular distance from the mid of the lesser trochanter to the interteardrop line
Statistics
Prostheses survival was calculated according to the Kaplan and Meyer method, and any reason for revision was considered as failure. The t-test for equality of means (to compare the means of variables) and the chi-square test (to assess the relationship between the cup orientation and CR and postoperative leg-length discrepancy) were used.
Results
None of the patients were lost to follow-up. There was one major complication in group A (sciatic nerve palsy) and three major complications in group B (one deep vein thrombosis, one crural nerve palsy, one haematoma), but complications were unrelated to CR (p = 0.25).
One prosthesis failure occurred in group A. The failure was due to ceramic liner fracture during childbirth five years after primary THR. The ceramic head, the liner, and the modular neck were revised. The cumulative survival at nine years was 95.7% (95% CI) for group A and 100% for group B.
Clinical results
At the latest follow-up, the mean HHS score was 74.88 in group A and 76.03 in group B with no statistically significant differences (p = 0.8). Also, the WOMAC score was not statistically different between the two groups (Table 2). No statistically significant differences were found with regards to preoperative (mean 1.85 cm in group A, 1.41 cm in group B, p = 0.06) and postoperative (p = 0.25) leg-length discrepancy (Table 3).
Radiographic results
Stem positioning was neutral in a majority of the cases (one stem >5° valgus and one stem >5° varus in group A; one >5° valgus in group B). All stems were stable without radiographic signs of distal migration.
All of the acetabular components were osteointegrated without evidence of migration or radiolucent lines. No signs of periprosthetic osteolysis were found in any prosthesis.
The inclination of the cup (CO) was independent of the centre of rotation (CR) (p = 0.05) as shown in Table 4.
There were no significant differences between the two groups with regard to CR medialisation, femoral off-set, or abductor muscles lever arm (Table 4).
Cup size distribution was not different between the two groups (Table 5). In group A, to achieve a good primary stability, two screws were used in 20 cases (45,4%), one screw in one case (2.3%), and no screws in 23 cases (52.3%). In group B, three screws were used in one case (2,3%), two screws in 12 cases (27.3%), one screw in three cases (6.8%), and no screws in 28 cases (63.6%).
The 15° antiverted-retroverted neck was predominantly used in group A, while the straight neck was used mainly in group B (Table 6).
Discussion
The aim of this study was to investigate the influence of HHCR on implant survival by using modular cementless prostheses and hard bearing surfaces in DDH patients. The hypothesis was that a modular neck stem, by restoring a correct soft-tissue balance and leg length, might avoid clinical impairment (limping) otherwise found with HHCR with standard prostheses, and that ceramic bearing surfaces, with their negligible wear [10], could have mitigated high joint reaction forces by avoiding wear and periprosthetic osteolysis.
The outcomes of 44 total hip arthroplasties (THAs) implanted in a HHCR were compared with those of 44 implanted in an ACR. No exclusion criteria were applied, no statistically significant differences in terms of sex, age, gender, and operative technique were found between the two groups. The implant model was the same in both groups.
This study came to the conclusion that, between the two groups, no statistically significant differences were found in clinical or radiographic results. The only failure reported (group A) was due to ceramic liner fracture caused by an inappropriate obstetric manoeuvre during labour, when an excessive abduction external rotation led to a hip subluxation and chipping of the ceramic liner rim. Ceramic liner fractures were usually recorded as the consequence of repeated trauma due to head subluxation and were sporadic events [22].
In our series, the liner fracture did not seem to be related to cup placement, because the only example reported was due to an inappropriate obstetric manoeuvre. Otherwise, to avoid possible ceramic fractures, a metal on metal alternative could have been recommended if a hip revision had been planned with a HHCR. Nevertheless, ceramic was preferred because of the possible complication of a metal coupling in relatively young patients [1, 16, 19] and the low incidence of ceramic fractures in our experience [22].
In patients with severe bone deficiency of the acetabular roof secondary to DDH, cup placement at the time of surgery can be troublesome. The majority of the techniques described require very good technical skills, and often a bone graft augmenting technique or expensive dedicated devices [15]. HHCR with a press-fit cementless cup is much easier, and does not require bone grafting or dedicated devices.
A similar experience has been reported for revision operations [12], but the level of activity of the population of this study is not comparable with the population of our study in which the average age at operation was less then 50 years (48.3 years in group A and 49 years in group B). The level of activity of the patient could be a critical factor for the long-term survival of the implant, because it could compound the effect of a high hip centre of rotation on joint reaction forces, increasing wear of the bearing surfaces (for polyethylene) or the risk of head or liner fracture (for alumina).
Otherwise, in contrast with the clinical results of this investigation, the majority of reports that studied the effect of a HHCR on total hip replacement showed poor clinical results [4, 14, 17, 21, 24]. In these studies a HHCR was considered to be a risk factor for aseptic loosening and prosthetic failure, but in all these clinical reports neither a hard bearing interface, nor a modular stem was used. Moreover, a cemented fixation for both components was usually applied. HHCR seemed to be predominantly critical for polyethylene cemented cups, and their survival also seemed to be affected by a cup medialisation greater than 2 mm [14]. Cup medialisation was found to be closely related to loosening, migration, and subsidence of both prosthetic components and calcar resorption.
Cup fixation technique is another important variable to influence HHCR survival as it is the effect of polyethylene wear under high reaction forces. The negative effect of high joint reaction forces on polyethylene was clinically confirmed in a study on 116 Charnley prostheses [24].
In an experimental study [8] where hip joint reaction forces were investigated it was shown that superolateral placement of the hip centre increased the joint reaction forces, while only superior placement did not alter these forces significantly. These results have been confirmed by a recent clinical study [3].
The influence of hip CR, prosthesis neck length, and neck-stem angle on hip muscles moment generating capacity were experimentally investigated by a computer model [7]. The authors suggested that, although superior relocation of the CR produced an alteration of the abductor muscles lever arm, this alteration could have been compensated for by increasing neck length and changing neck-stem angle.
Despite a lack of a control group with polyethylene liner and modular necks and the relatively short follow-up (nine years), this study seems to be the first clinical report supporting these experimental data in a series comparable with other studies reporting on this topic. Modular neck prostheses allow the restoration of femoral off-set, abductors moment arm, leg length and joint kinematics when the hip CR is relocated superiorly with respect to the ACR (Fig. 3).
Female, 34 years. Right hip DDH grade 2 (post osteotomy), left hip DDH grade 4. Using different necks a good offset was restored in both hips, leg length discrepancy was reduced from +35 mm on the left side before surgery to +12 mm after surgery. At the latest clinical evaluation the follow up was 8 years for the right side and 7 years for the left, prostheses were stable, Harris Hip Score 87
In difficult THR, when it is very demanding to place the socket within the anatomical position because of poor bone stock, it is a reasonable option to use a HHCR by reaming the bone in the higher part of the true acetabulum; thus the appropriate cup/bone contact and a good potential for bone ingrowth can be achieved. By this technique the cup is displaced just superiorly but not laterally (in our series no statistically significant differences between the groups were found concerning cup medialisation). Hip mechanics can be restored by modular necks with different lengths and geometries. Finally, to avoid the possible effect on survival of high hip joint reaction forces, a hard bearing coupling, such as ceramic, can be used.
On the other hand, the different severity of preoperative DDH between the two groups could be a possible limit of this study. This difference is due to the attempt to place the cup in the anatomical hip centre whenever possible without osteotomies or augmentation techniques. In high grades of dysplasia, an anatomical hip centre was rarely restored, resulting in 21 cases of high grade dysplasia (Crowe grade III–IV) in group A and none in group B. The difference in severity of dysplasia may affect leg length except in cases of bilateral disease, but the wide range of length options provided by modular heads and the two neck lengths (a range of possible lengthening of 17.5 mm with ceramic heads, of 24.5 mm with metallic heads) helps to solve the problem which is otherwise sensible with monoblock prostheses.
In conclusion, the results of this study are in contrast to other clinical series since porous coated cups, modular systems, and hard bearing surfaces were used. In critical cases of THA, such as high grade dysplasia, HHCR should be considered a feasible option if modular prosthesis, cementless cups, and hard bearing surfaces are used.
References
Baur W, Honle W, Willert HG et al (2005) Pathological findings in tissue surrounding revised metal/metal articulations. Orthopade 34:225–226, 228–233
Bellamy N, Buchanan WW, Goldsmith CH et al (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Bicanic G, Delimar D, Delimar M et al (2008) Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int Orthop Nov 18 [Epub ahead of print]. doi:10.1007/s00264-008-0683-z
Callaghan JJ, Salvati EA, Pellicci PM et al (1985) Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year follow-up. J Bone Joint Surg Am 67:1074–1085
Crowe JF, Mani VJ, Ranawat CS (1979) Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am 61:15–23
Dearborn JT, Harris WH (1999) High placement of an acetabular component inserted without cement in a revision total hip arthroplasty. Results after a mean of ten years. J Bone Joint Surg Am 81:469–480
Delp SL, Komattu AV, Wixson RL (1994) Superior displacement of the hip in total joint replacement: effects of prosthetic neck length, neck-stem angle, and anteversion angle on the moment-generating capacity of the muscles. J Orthop Res 12:860–870
Doehring TC, Rubash HE, Shelley FJ et al (1996) Effect of superior and superolateral relocations of the hip center on hip joint forces. An experimental and analytical analysis. J Arthroplasty 11:693–703
Engh CA, Bobyn JD, Glassman AH (1987) Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br 69:45–55
Hannouche D, Hamadouche M, Nizard R et al (2005) Ceramics in total hip replacement. Clin Orthop Relat Res 430:62–71
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755
Hendricks KJ, Harris WH (2006) High placement of noncemented acetabular components in revision total hip arthroplasty. A concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg Am 88:2231–2236
Jerosch J, Steinbeck J, Stechmann J et al (1997) Influence of a high hip center on abductor muscle function. Arch Orthop Trauma Surg 116:385–389
Karachalios T, Hartofilakidis G, Zacharakis N et al (1993) A 12- to 18-year radiographic follow-up study of Charnley low-friction arthroplasty. The role of the center of rotation. Clin Orthop Relat Res 296:140–147
Kobayashi S, Saito N, Nawata M et al (2003) Total hip arthroplasty with bulk femoral head autograft for acetabular reconstruction in developmental dysplasia of the hip. J Bone Joint Surg Am 85:615–621
Korovessis P, Petsinis G, Repanti M et al (2006) Metallosis after contemporary metal-on-metal total hip arthroplasty. Five to nine-year follow-up. J Bone Joint Surg Am 88:1183–1191
Lachiewicz PF, McCaskill B, Inglis A et al (1986) Total hip arthroplasty in juvenile rheumatoid arthritis. Two to eleven-year results. J Bone Joint Surg Am 68:502–508
Mattingly DA (2005) The S-rOM modular femoral stem in dysplasia of the hip. Orthopedics 28:s1069–s1073
Park YS, Moon YW, Lim SJ et al (2005) Early osteolysis following second-generation metal-on-metal hip replacement. J Bone Joint Surg Am 87:1515–1521
Sakai T, Sugano N, Ohzono K et al (2006) The custom femoral component is an effective option for congenital hip dysplasia. Clin Orthop Relat Res 451:146–153
Stans AA, Pagnano MW, Shaughnessy WJ et al (1998) Results of total hip arthroplasty for Crowe type III developmental hip dysplasia. Clin Orthop Relat Res 348:149–157
Toni A, Traina F, Stea S et al (2006) Early diagnosis of ceramic liner fracture. Guidelines based on a twelve-year clinical experience. J Bone Joint Surg Am 88(Suppl 4):55–63
Vasavada AN, Delp SL, Maloney WJ et al (1994) Compensating for changes in muscle length in total hip arthroplasty. Effects on the moment generating capacity of the muscles. Clin Orthop Relat Res 302:121–133
Yoder SA, Brand RA, Pedersen DR et al (1988) Total hip acetabular component position affects component loosening rates. Clin Orthop Relat Res 228:79–87
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Traina, F., De Fine, M., Biondi, F. et al. The influence of the centre of rotation on implant survival using a modular stem hip prosthesis. International Orthopaedics (SICOT) 33, 1513–1518 (2009). https://doi.org/10.1007/s00264-008-0710-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-008-0710-0