Abstract
This study entails a prospective evaluation of lumbar closing wedge osteotomy for correction of thoracolumbar kyphotic deformity in ankylosing spondylitis. Twenty patients with a median age of 52 years (range, 26–70) underwent follow-up at one year. The lumbar closing wedge osteomtomy was stabilised by metallic rods fixed by transpedicular screws. Outcome measures were quality of life (EuroQol), occiput-to-wall distance, pain, fatigue, complications, technical and radiological evaluation. The technical result was good in 16 and fair in four patients; two had neuropraxia. The deformity was reduced an average of 17° (95% confidence interval 15–25°) at one-year follow-up. Pain during activity, pain at night, and fatigue were significantly reduced. EuroQol improved from 0.42 to 0.69 (p = 0.002) and occiput-to-wall distance from 26 to 18 cm (p = 0.005). Functional outcome was improved after lumbar closing wedge osteotomy in ankylosing spondylitis.
Résumé
Evaluation prospective d’une ostéotomie lombaire à foyer fermé pour correction de cyphose lombaire chez les patients présentant une spondylarthrite ankylosante. Matériel et méthode: 20 patients dont l’âge moyen était de 52 ans (entre 26 et 70 ans) ont été suivis pendant un an et demi. Les vertèbres lombaires ont été stabilisées par deux tiges métalliques fixées par des vis transpédiculaires. Le devenir des patients a été analysé selon les critères de vie EUROQOL, selon la déformation résiduelle, les douleurs, la fatigue, les complications et la radiologie. Résultats: les résultats ont été bons chez 16 patients et passables chez 4 patients qui présentaient des troubles neurologiques résiduels (neuropraxie). A un an de recul, a déformation a été réduite en moyenne de 17°. La douleur, l’activité et la fatigue ont été significativement diminuées. L’index d’EUROQOL amélioré de 0,42 à 0,69 (p = 0,002), la flèche de cyphose mesurée en C1 de 26 à 18 cm (p = 0,005). Conclusion: dans les spondylarthrite ankylosante, l’ostéotomie lombaire à foyer fermé peut améliorer le devenir fonctionnel des patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of spondyloarthritis in the general population is estimated to be between 0.6% and 1.9% while that for ankylosing spondylitis (AS) has been estimated at 0.1–1.4% [3, 8, 17]. Pain and disability in patients with severe AS are similar to that found in age- and gender-matched patients with severe rheumatoid arthritis. Absence from work and work disability leave are increased [2, 17, 24]. Prevalent quality of life concerns are stiffness (90%), pain (83%), fatigue (62%), poor sleep (54%), concerns about appearance (50%), worry about the future (50%), and medication side effects (41%) [21]. The main targets for treatment are back pain caused by sacroiliitis, spondylitis/spondylodiscitis, enthesitis, ankylosis, joint pain, and organ involvement (uveitis, psoriasis, colitis, internal organs).
In some patients, the inflammation and joint destruction, mainly along the spine, result in a severe thoracolumbar kyphotic deformity (TLKD) of the spine. Cosmetic appearance, lack of horizontal vision, secondary neck pain, and headache are associated problems in these patients. Three surgical techniques have been employed for correction of the TLKD caused by AS: opening wedge osteotomy, polysegmental wedge osteotomy (isthmic and joint resections), and closing wedge osteotomy. According to a structured review evaluating 41 mostly retrospective studies operations on 856 patients, technical and clinical outcome data have been poorly reported [20]. Most of the studies have focussed on surgical technique. The indication for osteotomy has not been established. The average surgical correction reported in the review was 37–40° for all three techniques. About the same surgical correction for one-level osteotomy is reported in later studies [1, 5, 13]. Neuropraxia is reported in 5–10% of patients independent of surgical technique [20]. Fatalities from, for example, major pulmonary, cardiac, and intestinal complications have been reported in 4% of the operations.
Previously published studies have several methodological limitations: most of the studies are retrospective with follow-up by the spine surgeon and validated clinical measures have not been applied. The purpose of this study was to prospectively assess functional and technical outcome after closing wedge surgery in AS patients with severe TLKD.
Materials and methods
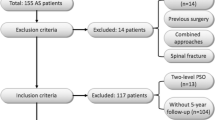
AS was diagnosed according to the 1984 New York criteria [19], and at least one rheumatologist had previously evaluated the patients. The main indication for surgery was the inability to look straight ahead and complaints about appearance, interpersonal communication, and secondary neck pain. Two female and 19 male patients were included in the study. Median age was 52 (range, 26–70) years with a median duration of disease of 30 (range, 4–45) years. Twenty patients had peripheral joint pain, nine had previous or current iridocyclitis, and six had cardiovascular disease. Ten patients had previous surgery, and four had hip prostheses. Seven patients worked full time. The regional ethics committee approved the project, and written consent was obtained from all patients.
Surgical technique
The patients were operated upon by two experienced spine surgeons (RS and RR). The patient is normally placed prone on a three-post spinal frame. The chest and pelvis were supported on firm padded blocks, leaving the abdomen hanging free. A midline skin incision was made to allow adequate levels of exposure of the laminae and transverse processes. The posterior elements of one vertebra, usually L3, including the lamina, articular processes, and pedicles in combination with a posterior wedge of the vertebral body were resected. The position of the screws was confirmed by intraoperative radiograph. The correction was achieved by passive extension of the lumbar (thoracolumbar) spine by lifting the torso. Transpedicular screws were inserted in the vertebrae three levels above and three levels below the osteotomy segment to ensure stability and consolidation. Blocks of resected spinous process were bridged posteriorly and posterolaterally for fusion. Patients stayed one to three days in the intensive care unit for close monitoring of their haemodynamic and neurological status. Patients were usually allowed out of bed and began ambulation from the first to the fourth postoperative day depending on their condition. A well-moulded thoracolumbosacral brace is worn for three to six months. When two-level osteotomy is required for severe deformity, it is usually performed in a one-staged fashion. It is designed in such a way that at least one vertebra is left intact between the two osteotomy sites. As a result, potential neurovascular injury is minimised and the bone-implant construction is more stable.
Outcome measures
All outcome measures were obtained by physicians who were not directly engaged in the operations. Using standard Cobb’s method on standing lateral radiograph of the whole spine, the lumbar lordosis was measured from the lower endplate of T12 to the upper endplate of S1. The reliability and reproducibility of this method is good [14]. Kyphosis was measured from the upper endplate of the highest visible thoracic vertebra above T5 to the upper endplate of T12 [15]. The TLKD was defined as the thoracic kyphosis minus the lumbar lordosis. In normal subjects, the physiological thoracic kyphosis and lumbar lordosis tend to negate each other, resulting in a measurement of around zero degrees. One experienced radiologist measured all radiographs.
Intraoperative, postoperative, and general complications were registered and classified according to Willems et al. [23]. Outcome was classified as good, fair, or poor according to the technical outcome grading criteria reported by van Royen and de Gast [20].
Patients filled in a questionnaire at baseline and at one-year follow-up. Pain during activity, pain at night, peripheral joint pain, and fatigue were scored by using a numerical scale ranging from 1 (no pain at all) to 9 (worst possible pain) [4]. EuroQol is a generic (nondisease specific) instrument for measurement of health status [7, 18]. The questionnaire includes five items regarding quality of daily life covering the domains of mobility, self-care, usual activities, pain and discomfort, and anxiety and depression (EQ-5D) and a visual analogue for assessment of overall current health (EQ-VAS) scored from 0 (worst imaginable) to 100 (best imaginable). Items for EQ-5D use a three point adjectival response scale. Scores are transformed using utility weights from the general population to produce a single index with scores ranging from −0.59 for the worst possible health state to +1 for the best possible health state. EuroQol is an acceptable questionnaire for measuring health-related quality of life in arthritis and correlates well with disease-specific questionnaires for AS [9]. Commonly-used disease-specific questionnaires have not been validated in patients with thoracolumbar deformity.
The questionnaire included emotional distress, medication, and work status. Emotional distress was rated using the Hopkins Symptom Check List (HSCL-25) [6]. Patients score 25 symptoms from 1 (not at all) to 4 (extremely). The use of daily pain medication was registered (drug name and dosage) for the week just prior to inclusion and at the one-year follow-up. The consumption of different classes of drugs was calculated with defined daily doses as a measurement unit. Drugs were classified according to therapeutic group, defined by the anatomical therapeutic chemical system [4, 22]. The therapeutic groups were: analgesics; anxiolytics, hypnotics and sedatives; antidepressants; anti-inflammatory agents (NSAIDs); and muscle relaxants. One defined daily dose equals 3 g paracetamol (acetaminophen) or 0.5 g naproxen.
Evaluation of work status included questions about paid work (full-time, part-time, not working) and status if not working (on sick leave, vocational or medical rehabilitation, disability leave, unemployed, other [homemaker or student]). The assessment of work status was considered standard and reliable in the target population [12].
Occiput-to-wall distance (OWD) was obtained as a reliable estimate for cervical and thoracic spine extension and was measured by the same physician before and after surgery [11].
Statistical analysis
Results are presented as means (SD), medians (range), or proportions. The normal distribution of baseline, follow-up data, and differences was checked by histograms. Differences are presented as means (95% confidence interval [CI]). Paired t tests (two-sided) were used to assess differences from baseline to one-year follow-up. Correlations (Pearson’s r) between correction of deformity and changes in occiput-to-wall distance and quality of life were calculated.
Results
The mean operation time was 285 minutes (range, 180–435 minutes). Seventeen wedge osteotomies were performed over L3 and four were performed over L2. A double wedge osteotomy was performed in five patients, T11 in three patients, and T12 in two patients. The number of mean segments fused was eight (range, 4 to 18). Average blood transfusion volume was 4,640 ml (range, 700–15,000 ml). The deformity was reduced by 20° (95% CI 15–20°) postoperatively. Twelve complications were registered in eight patients (Table 1); none were fatal or related to serious vascular injuries. Two patients had a revision operation because of implant failure. Extension of the instrumentation one level above and below was performed on one patient with implant failure. This patient eventually had solid fusion with excellent results. Deep wound infection developed in one patient, who was successfully treated within three weeks postoperatively.
Twenty patients had follow-up at one year. The last patient did not want to attend follow-up. His technical postoperative result was excellent. Over a short telephone consultation, he reported that his pain and disability was unaltered from before surgery. Technical results were graded as good in 16 (80%) and fair in four patients (Table 2). The deformity increased 3° (95% CI 1–5°) from postoperative to one-year follow-up. Significant mean improvements were observed for occiput-to wall-distance, pain during activity and at night, fatigue, and quality of life (Table 3). Emotional distress was in the normal range both before surgery and at one-year follow-up. The operation did not improve the patients’ work status. Seven patients were working full-time before surgery and six patients at one-year follow-up, while 11 had a disability pension prior to surgery and 13 at one-year follow-up. The correction of the deformity correlated poorly with improvements in quality of life (EQ-5D [r = 0.08], EQ-VAS [r = 0.21]) and occiput-to wall-distance (r = 0.31).
Discussion
The evidence for spinal surgery in AS is weak, but a recent expert committee recommended a closed wedge osteotomy [25]. Their judgement was based on clinical experience of respected authorities. We report improvement in terms of validated functional outcome in AS after closed wedge osteotomy. Consistent and significant improvements were observed for health-related quality of life and occiput-to-wall distance. The Ankylosing Spondylitis Assessment Study group (ASAS) have recommended a core set for evaluation [25]. We used five of the recommended domains (physical function, pain, spinal mobility, fatigue, and imaging). Unfortunately we did not use the Bath ankylosing spondylitis functional index (BASFI), but we included additional measures of health-related quality of life (EuroQol).
Few studies have evaluated functional outcome and quality of life after surgery for deformity of ankylosing spondylitis. Halm et al. used a retrospective questionnaire to assess outcome, and Kim et al. used a modified arthritis impact measurement scale (AIMS) at the final follow-up [10, 13]. Kim et al. did not present preoperative scores but reported that all scales of the AIMS had improved. In our study, preoperative mean values for the EQ5D-index were lower than reference values for AS and preoperative values for patients before liver transplantation [7, 9, 16]. This observation indicates that health-related quality of life was severely affected at baseline in the patients included. Results from one-year follow-up were higher than reference values for AS and values reported after liver transplantation, which suggest clinically significant improved health-related quality of life.
Spinal osteotomy surgery in AS is accompanied by relatively high numbers of complications. Both the extensive surgery and the autoimmune character of disease including direct related comorbidity, and an unfavourable biomechanical situation, contribute to the observed complication rate. The rate observed in this study is similar to that found in previous studies [5, 20, 23]. The most common complications—permanent neurological, deep wound infections, and major general—are reported at a rate of about 10% each. A recent systematic review reported that the incidence of perioperative mortality was 5.8% in opening wedge osteotomy and 1.3% in closing wedge osteotomy [20]. We observed no fatal complications.
Independent observers obtained radiological evaluation and technical grading. The mean correction of 17° at one-year follow-up of the TLKD is lower than the reduction reported in most previous studies [5, 10, 20]. Nevertheless, functional outcome was good and the overall technical results (80% success) were comparable to previous studies (78%) [20].
The weak correlations observed for improvements in deformity and quality of life agree with the previous study by Kim et al. [13] These findings together with the high surgical risk factor suggest that a control group, preferably in a randomised design, should be included in future studies.
References
Berven SH, Deviren V, Smith JA, Emami A, Hu SS, Bradford DS (2001) Management of fixed sagittal plane deformity: results of the transpedicular wedge resection osteotomy. Spine 26:2036–2043
Boonen A, de Vet H, van der Heijde D, van der Tempel H, van der Linden S (2001) Work status and its determinants among patients with ankylosing spondylitis. A systematic literature review. J Rheumatol 28:1056–1062
Braun J, Bollow M, Remlinger G, Eggens U, Rudwalteit M, Distler A et al (1998) Prevalence of spondylarthropathies in HLA-B27 positive and negative blood donors. Arthritis Rheum 41:58–67
Brox JI, Staff PH, Ljunggren AE, Staff PH (1993) Arthroscopic surgery compared with supervised exercises in patients with rotator cuff disease (stage II impingement syndrome). BMJ 307:899–903
Chang KW, Chen YY, Lin CC, Hsu HL, Pai KC (2005) Closing wedge osteotomy versus opening wedge osteotomy in ankylosing spondylitis with thoracolumbar kyphotic deformity. Spine 30:1584–1593
Derogatis LR, Lipman RS, Rickels K, Uhlenut EH, Cori L (1974) The Hopkins Symptom Checklist (HSCL): a self-report inventory. Behav Sci 19:1–15
EuroQolGroup (1990) EuroQol—a new facility for the measurement of health related quality of life. Health Policy 16:199–208
Gran JT, Husby G (1984) Ankylosing spondylitis: a comparative study of patients in an epidemiological survey, and those admitted to a department of rheumatology. J Rheumatol 11:788–793
Haywood KL, Garratt AM, Dziedzic K, Daves PT (2003) Patient centered assessment of ankylosing spondylitis-specific health related quality of life: evaluation of the patient generated index. J Rheumatol 30:764–773
Halm H, Metzstavenhagen P, Zielke K (1995) Results of surgical correction of kyphotic deformities of the spine in ankylosing spondylitis on the basis of the modified arthritis impact measurement scales. Spine 20:1612–1619
Heuft-Dorenbosch L, Vosse D, Landewe R, Spoorenberg A, Dougdos M, Mielants H (2004) Measurement of spinal mobility in ankylosing spondylitis: comparison of occiput-to-wall and tragus-to-wall distance. J Rheumatol 31:1779–1784
Holm I, Friis A, Storheim K, Brox JI (2003) Measuring self-reported functional status and pain in patients with chronic low back pain by postal questionnaires. A reliability study. Spine 28:828–833
Kim KT, Suk KS, Cho YJ, Hong GP, Park BJ (2002) Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity. Spine 27:612–618
Polly DW, Kilkelly FX, Mchale KA, Asplund LM, Mulligan M, Chang AS (1996) Measurement of lumbar lordosis: evaluation of intraobserver, interobserver, and technique variability. Spine 21:1530–1535
Rahali-Khachlouf H, Poiraudeau S, Fermanian J, Ben Saleh FZ, Dziri C, Revel M (2001) Validite et reproductibilite des mesures cliniques rachidiennes dans la spondylarthrite ankylosante. Ann Readapt Med Phys 44:205–212
Ratcliffe J, Longworth L, Young T, Bryan S, Burroughs A, Bryan S (2002) Assessing health-related quality of life pre- and post-liver transplantation: a prospective multicenter study. Liver Transpl 8:263–270
Saraux A, Guedes C, Allain J, Devauchelle V, Valls I, Lamour A et al (1999) Prevalence of rheumatoid arthritis and spondyloarthropathy in Brittany, France. J Rheumatol 26:2622–2627
Tosteson ANA (2000) Preference-based health outcome measures in low back pain. Spine 25:3161–3166
van der Linden S, Valkenburg H, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis: a proposal for modification of the New York criteria. Arthritis Rheum 27:361–368
van Royen BJ, De Gast D (1999) Lumbar osteotomy for correction of thoracolumbar kyphotic deformity in ankylosing spondylitis. A structured review of three methods of treatment. Ann Rheum Dis 58:399–406
Ward MM (1999) Health-related quality of life in ankylosing spondylitis: a survey of 175 patients. Arthritis Care Res 12:247–255
WHO (2002) ATC index with DDDs. Who Collaborating Centre for Drug Statistics Methodology, Oslo, Norway
Willems KF, Slot GH, Anderson PG, Pavlov PM, de Kleuver M (2005) Spinal osteotomy in patients with ankylosing spondylitis: complications during first postoperative year. Spine 30:101–107
Zink A, Braun J, Listing J, Wollenhaupt J (2000) Disability and handicap in rheumatoid arthritis and ankylosing spondylitis—results from the German rheumatological database. J Rheumaol 27:613–622
Zochling J, van der HD, Burgos-Vargas R, Collantes E, Davis JC, Dijkmans B et al (2006) ASAS/EULAR recommendations for the management of ankylosing spondylitis. Ann Rheum Dis 65:442–452
Acknowledgments
The authors thank the patients who participated in the study and the nurses and nurse aids at the hospital departments and outpatient clinics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brox, J.I., Helle, A., Sørensen, R. et al. Functional outcome after lumbar closing wedge osteotomy in ankylosing spondylitis. International Orthopaedics (SICOT) 33, 1049–1053 (2009). https://doi.org/10.1007/s00264-008-0590-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-008-0590-3