Abstract
We compared a minimally invasive surgical technique to the conventional (open approach) surgical technique used in fixation of hip fractures with the dynamic hip screw (DHS) device. Using a case-control design (44 cases and 44 controls), we tested the null hypothesis that there is no difference between the two techniques in the following outcome measures: duration of surgery, time to mobilisation and weight bearing postoperatively, length of hospital stay, mean difference of pre- and postoperative haemoglobin levels, position of the lag screw of the DHS device in the femoral head, and the tip–apex distance. The minimally invasive DHS technique had significantly shorter duration of surgery and length of hospital stay. There was also less blood loss in the minimally invasive DHS technique. The minimally invasive DHS technique produces better outcome measures in the operating time, length of hospital stay, and blood loss compared to the conventional approach while maintaining equal fixation stability.
Résumé
Ce travail a pour but de comparer les techniques de fixation de fractures de la hanche par voie mini-invasive ou par voie d’abord conventionnelle avec utilisation de matériel de type DHS. Nous avons pour cette étude regroupé les patients en deux groupes, 44 cas par voie mini-invasive et 44 cas contrôle. Nous avons voulu tester l’hypothèse suivante: existe-t-il une différence entre ces deux techniques, sur la durée d’intervention, de reprise de l’appui post-opératoire; de durée moyenne de séjour des pertes sanguines notamment et enfin, en ce qui concerne la position de la vis céphalique dans la tête fémorale et sa distance par rapport à l’interligne. La technique mini-invasive entraîne de façon significative un temps chirurgical diminué et une diminution de la durée moyenne de séjour. Ceci est également vrai pour les pertes sanguines. Cette technique est pour nous supérieure en ce qui concerne ces items si on la compare à l’abord de type conventionnel en sachant que les problèmes de stabilité du matériel sont identiques quelle que soit la technique utilisée.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures are a common cause of morbidity and mortality in the elderly population and are associated with considerable health expenditure in most industrialised countries [4]. The dynamic hip screw (DHS) has been the standard type of fixation for intertrochanteric fractures [3, 20]. In the attempt to find less invasive techniques to simplify surgery and minimise complications by reducing surgical time and blood loss [1], some authors used custom made implants [11] or new devices which require the purchase of additional armamentarium by the hospital [5]. We used a case-control study design to ascertain the short-term safety and effectiveness of a standardised DHS device inserted using a minimally invasive technique compared with the same implant inserted in a traditional fashion to manage AO Classification 31-A1.1 and 31-A1.2 & 31-A2.1 and 31-A2.2 fractures.
Methods
Ethics approval
All the procedures described in this article were approved by the local ethics committee. All patients gave written informed consent to take part in the study. The study recruited patients with an extracapsular hip fracture who were mentally competent and gave their informed consent to take part.
Patients
In the period September 2003 to July 2006, 44 patients underwent a minimally invasive DHS for fixation of their intertrochanteric hip fractures. All operations were performed by a single, fully trained orthopaedic surgeon with a special interest in the procedure. The patients represented the whole cohort of patients with extracapsular hip fractures operated on by that surgeon in the period of study. The department had a total of 16 fully trained orthopaedic surgeons on the on-call trauma rota with one surgeon in general charge of these patients; this surgeon operated on more than 80% of all hip fractures. Patients who received a conventional DHS were operated on by fully trained orthopaedic surgeons in the same period. The patients were not preselected for the procedure and were part of a cohort of 288 patients with extracapsular hip fractures operated on by those surgeons in the period between September 2003 and July 2006. Each patient within the ’minimally invasive DHS’ group was matched, according to their sex, age, ASA grade, date of surgery, and fracture type according to the AO classification, to a patient who has had their hip fracture fixed with a DHS placed through the conventional approach. The classification and match of the hip fracture patients was performed by two orthopaedic trainees who had not been involved in the initial management of the patients. When there was a difference in opinion between the two orthopaedic trainees an agreement was reached after consultation with a fully trained orthopaedic surgeon who had not been involved in the initial management of the patients.
We tested the null hypothesis that there is no difference between a minimally invasive DHS approach or a conventional (open procedure) DHS approach in the following outcome measures: duration of surgery, time to mobilisation and weight bearing postoperatively, length of hospital stay, mean difference of pre- and postoperative haemoglobin (Hb) levels, position of the lag screw of the DHS device in the femoral head, and the tip–apex distance.
Minimally invasive surgical technique
All patients in this study had adequate closed reduction (anatomical to 10° of valgus on antero-posterior radiograph and anatomical on lateral) prior to the start of surgery. The incision is placed under fluoroscopic guidance by identification of the site on the hip that corresponds to the position of the fractured neck of femur. The size of the incision is no longer than 5 cm. The iliotibial band and muscle are split in one incision with the scalpel blade [1]. After the insertion of a guide wire, reaming is carried out through this incision. The standard AO screw and side plates are introduced through the small incision under fluoroscopic guidance. The side plate is then placed over the guide wire as in the conventional technique and then rotated until it lies under the skin and fascia. The side plate screws are placed in the usual manner by retracting the skin and subcutaneous tissue with a right angle retractor. No drain is used, and deep layers and the skin incision closure are performed in the usual fashion. Final fluoroscopy views are taken as in any other conventional side plate fixation technique.
Conventional technique
All the operations in a given centre were performed by a single, fully trained orthopaedic surgeon with a special interest in the procedure who had been trained by the senior author (NM) before he started to use a minimally invasive approach. Each of these surgeons had performed at least 200 DHS fixations for extracapsular hip fractures. Through a skin incision 15 cm long, the fascia lata is incised longitudinally. The vastus lateralis muscle is split under direct vision [12]. A Cobb dissector is then used to gently sweep the musculature off the intermuscular septum to allow identification and electro-coagulation of the perforators from posterior to anterior. Following fixation of the fracture in the standard fashion, a drain was used according to surgeon’s preference, and the incision was closed in layers.
Outcome measures and statistical analysis
Demographic data for both case and control groups of patients were collected. Descriptive statistics for ASA grade and type of anaesthesia were determined. The Mann-Whitney test (95% CI for difference between population medians) for nonparametric outcome measure was used to compare length of time from admission to operation, duration of surgery, time to mobilisation and weight bearing postoperatively, and length of hospital stay. In both groups, bleeding was measured by the summation of the blood collected from a plastic bag taped to the surgical drapes, below the operative field, and from the weighed swabs.
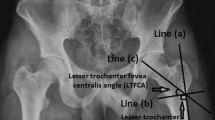
The fluoroscopic images for both groups of patients were assessed as an indicator of the quality of fracture reduction. The location of the tip of the DHS screw in the femoral head was recorded as defined previously [12]. The tip–apex distance [2] was also measured. Antero-posterior and lateral postoperative radiographs were viewed to obtain these two measurements. The mean difference of pre- and postoperative Hb levels and the tip–apex distance was compared using the independent two-tailed t test (95% confidence interval for difference between means) for parametric data.
Results
Patients
Forty-four patients constituted the minimally invasive DHS group. They were matched with 44 patients in the conventional DHS groups according to the matching criteria described above (Table 1).
Patients received routine antibiotic prophylaxis with 1.5 g of cefuroxime given intravenously on induction of anaesthesia. In patients who were at a higher risk of colonisation by methicillin-resistant staphylococcus aureus, 80 mg of gentamicin were added. Patients were given prophylactic anticoagulation with low molecular weight heparin (2500 i.u. deltaparin, Pharmacia Ltd). Where there were no contraindications, this was replaced by 150 mg Aspirin (Kent Pharmaceuticals) after 48 hours. Thromboembolic deterrent stockings were used in every patient on the opposite side of hip fracture in addition to medical prophylaxis of venous thromboembolism.
In the 24 patients in the conventional DHS group who had drains inserted after surgery, these were removed 24–48 hours after surgery. Drains were not used in the minimally invasive DHS group. All the patients in both cohorts had the same postoperative rehabilitative regime, starting mobilisation and weight bearing within 24 hours of surgery unless specified otherwise by the surgeon. The difference of the median duration of surgery and median length of hospital stay were statistically significant between the two groups of patients. These outcome measures were more favourable in the minimally invasive group than the conventional DHS group. The mean difference of preoperative and postoperative Hb levels was lower in the minimally DHS group when compared to the conventional DHS group, but this was found to be not significant statistically. The mean tip–apex distance in both groups of patients was similar. One patient in the minimally invasive DHS group and two patients in the conventional DHS group had tip–apex distances of more than 27 mm. Table 2 shows the summary of statistical data from the outcome measures outlined above and the amount of postoperative analgesia used.
The distribution of the location of the tip of the screw in the femoral head was similar in both groups (Table 3).
Complications
Five patients from the conventional DHS group required transfusion of two units of blood each due to perioperative blood loss. A transfusion threshold of 9 g/dL of haemoglobin was used as an indication for transfusion. Two patients from the minimally invasive DHS group had dehiscence of the wound site. This was managed by dressing of the wound, which healed uneventfully. In the conventional DHS group, four patients developed infection of the surgical wound which required treatment with systemic antibiotics and wound dressings.
Two patients in the minimally invasive DHS group needed replacement of the fixation device with a prosthesis due to avascular necrosis of the femoral head following screw cut-out. In the conventional DHS group, two patients developed avascular necrosis of the femoral head following screw cut-out. Prosthetic replacement was performed. In these four patients, the tip–apex distance was less than 27 mm, and the fracture type was 31-A1.2 in two patients and 31-A2.1 in two patients. In one patient in the minimally invasive DHS group, a two-hole side plate pulled out of the femoral shaft five weeks after the index operation. It was replaced with a four-hole side plate extending the original wound to a length of 6 cm, with no adverse effect.
Discussion
In this study, 94% (83/88 patients) of the fractures in both the minimally invasive and conventional DHS surgery groups healed without any complication. In this respect, both techniques of fixation of hip fractures worked well. There was no difference in the following outcome measures when the two groups of patients were compared: time from surgery to mobilisation and weight bearing postoperatively, position of the lag screw of the DHS device in the femoral head and the tip–apex distance. On the other hand, there were significant differences in the duration of surgery and length of hospital stay between the two cohorts of patients. Although the mean differences of pre- and postoperative haemoglobin levels between the two groups were not significant statistically, clinically this may have great significance, as five patients in the conventional DHS group required blood transfusion postoperatively while none of the patients in the minimally invasive DHS group required any blood transfusion. The minimally invasive DHS requires less operating time, reduces the amount of intraoperative blood loss, and allows patients to be discharged earlier. This may carry benefit to the patients, and has significant financial implications to the hospital [7, 9, 10, 14, 18, 19, 21].
The results of this study are comparable with the results of a randomised controlled trial [1] where a prospective, surgeon-randomised, blinded-outcome clinical study comparing the use of the standard DHS device in a minimally invasive and conventional surgical approach was carried out. The minimally invasive technique group of patients had significantly less blood loss and shorter operating time.
The percutaneous compression plate (PCCP) is a new implant for the minimally invasive treatment of pertrochanteric hip fractures [5]. The PCCP seems to be similar to the DHS in relation to bone and stability, but has significant advantages for blood loss, soft tissue healing, and operation time [5]. While the results were promising, the economic and logistical disadvantage caused by the need to increase hospital inventory and the learning curve involved in familiarising oneself with the new equipment offsets its perceived advantage. On the other hand, the minimally invasive DHS technique uses the existing instruments with which the operating team is familiar and confident, with no need to purchase new instruments. This and other studies [1–8] have shown that the same advantages can be gained by modifying the surgical approach while using existing fixation devices, thus requiring neither a new plating system nor training of operating theatre staff to familiarise with them.
The type of DHS device used in both the minimally invasive surgical and conventional approaches were mainly four-hole side plates, but the choice of the length of the side plate was left to the individual surgeons. Biomechanical studies demonstrated equivalent peak load to failure results when comparing the two- and four-hole DHS plates [15]. In recent studies [13, 22], stable pertrochanteric fractures (AO classification 31-A1 and 31-A2) had successful fixation with two-hole DHS. It is possible that the widespread use of four-hole side plate DHS in stable pertrochanteric fractures is merely based on tradition, and needs reconsideration in this era of evidence-based medicine. Therefore, using the two-hole DHS may be at least as safe as the four-hole DHS, as the surgical exposure required will be smaller. It may be economical financially and in the use of operating time. In osteporotic bone, though, it may be safer to use longer side plates.
Our study showed a relatively high incidence of avascular necrosis of the femoral head.
There are limitations to this study. For example, this is a case control study; therefore, several variables could not be accounted for and may produce differences in outcome. This is true, for example, for the choice of anaesthesia. In the minimally invasive DHS group, more patients received general anaesthesia. However, as spinal and epidural anaesthesia produce less blood loss than general anaesthesia [16], the differences found in this investigation are even more remarkable.
This is a short term investigation. We deliberately did not want to perform a longer term outcome study to ascertain the longer term effects of hip fracture surgery. Our resources and ethics committee did not allow us to undertake such work, but we are confident that we are unlikely to have produced adverse effects on our patients undergoing minimally invasive DHS fixation.
Recent studies using robust research methodology have ascertained the safety of limited access hip fracture surgery, and have demonstrated that it is associated with decreased bleeding and postoperative pain, reduced postoperative morbidity, and faster recovery of function [17]. Our results confirm these findings.
Conclusions
Minimally invasive surgical techniques, as a whole, reduce operative complications and postoperative morbidity [5]. Our study shows that, when compared with the conventional approach in the implantation of the DHS device, the minimally invasive surgical technique described here resulted in shorter duration of surgery and length of hospital stay, as well as less intraoperative blood loss. This is accomplished without compromising the stability of fracture fixation.
References
Alobaid A, Harvey EJ, Elder GM, Lander P, Guy P, Reindl R (2004) Minimally invasive dynamic hip screw: prospective randomized trial of two techniques of insertion of a standard dynamic fixation device. J Orthop Trauma 18:207–212
Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM (1995) The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am 77:1058–1064
Bolhofner BR, Russo PR, Carmen B (1999) Results of intertrochanteric femur fractures treated with a 135-degree sliding screw with a two-hole side plate. J Orthop Trauma 13:5–8
Boufous S, Finch CF, Lord SR (2004) Incidence of hip fracture in New South Wales: are our efforts having an effect? Med J Aust 180:623–626
Brandt SE, Lefever S, Janzing HM, Broos PL, Pilot P, Houben BJ (2002) Percutaneous compression plating (PCCP) versus the dynamic hip screw for pertrochanteric hip fractures: preliminary results. Injury 33:413–418
Clague JE, Craddock E, Andrew G, Horan MA, Pendleton N (2002) Predictors of outcome following hip fracture. Admission time predicts length of stay and in-hospital mortality. Injury 33:1–6
Craig NJ, Maffulli N (2005) Subtrochanteric fractures: current management options. Disabil Rehabil 27:1181–1190
DiPaola M, Rozbruch SR, Helfet DL (2004) Minimal incision technique using a two-hole plate for fixation of stable intertrochanteric hip fractures. Orthopedics 27:270–274
Dougall TW, Duthie R, Maffulli N, Hutchison JD (1996) Antibiotic prophylaxis: theory and reality in orthopaedics. J R Coll Surg Edinb 41:321–322
Douglas S, Bunyan A, Chiu KH, Twaddle B, Maffulli N (2000) Seasonal variation of hip fracture at three latitudes. Injury 31:11–19
Ingman AM (2000) Percutaneous intramedullary fixation of trochanteric fractures of the femur. Clinical trial of a new hip nail. Injury 31:483–487
Kyle RF, Gustilo RB, Premer RF (1979) Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg Am 61:216–221
Laohapoonrungsee A, Arpornchayanon O, Phornputkul C (2005) Two-hole side-plate DHS in the treatment of intertrochanteric fracture: results and complications. Injury 36:1355–1360
Maffulli N, Dougall TW, Brown MT, Golden MH (1999) Nutritional differences in patients with proximal femoral fractures. Age Ageing 28:458–462
McLoughlin SW, Wheeler DL, Rider J, Bolhofner B (2000) Biomechanical evaluation of the dynamic hip screw with two- and four-hole side plates. J Orthop Trauma 14:318–323
Parker MJ, Handoll HH, Griffiths R (2004) Anaesthesia for hip fracture surgery in adults. Cochrane Database of Systematic Reviews CD000521
Peyser A, Weil YA, Brocke L, Sela Y, Mosheiff R, Mattan Y, Manor O, Liebergall M (2007) A prospective, randomised study comparing the percutaneous compression plate and the compression hip screw for the treatment of intertrochanteric fractures of the hip. J Bone Joint Surg Br 89:1210–1217
Rose S, Maffulli N (1999) Hip fractures. An epidemiological review. Bull Hosp Jt Dis 58:197–201
Shabat S, Mann G, Nyska M, Maffulli N (2005) Scoring systems to evaluate elderly patients with hip fractures. Disabil Rehabil 27:1041–1044
Shah MR, Aharonoff GB, Wolinsky P, Zuckerman JD, Koval KJ (2003) Outcome after hip fracture in individuals ninety years of age and older. J Orthop Trauma:S6–11
Tarantino U, Oliva F, Impagliazzo A, Mattei A, Cannata G, Pompili GF, Maffulli N (2005) A comparative prospective study of dynamic variable angle hip screw and gamma nail in intertrochanteric hip fractures. Disabil Rehabil 27:1157–1165
Verhofstad MH, van der Werken C (2004) DHS osteosynthesis for stable pertrochanteric femur fractures with a two-hole side plate. Injury 35:999–1002
Acknowledgements
Dr Ho completed this investigation as part of his requirement of his Research Module in Trauma and Orthopaedics. Dr Garau was recipient of a Research Studentship from the Societa’ Italiana di Ortopedia e Traumatologia (SIOT).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ho, M., Garau, G., Walley, G. et al. Minimally invasive dynamic hip screw for fixation of hip fractures. International Orthopaedics (SICOT) 33, 555–560 (2009). https://doi.org/10.1007/s00264-008-0565-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-008-0565-4