Abstract
Despite recent developments in fracture treatment, cases of non-union after long bone fractures are still encountered. This work aims at evaluating the active management of delayed union after the bridge-plate fixation of multifragmentary diaphyseal fractures by a limited surgical interference. Nineteen patients were included. All had revision surgery for delayed union of multifragmentary diaphyseal fractures after bridge-plate fixation. The period between primary and revision surgery was 12–20 weeks. Increasing stability was performed by adding more screws in all cases. Interfragmentary compression was performed in 16 patients. Axial compression of the fracture was applied in two patients, while one patient had the plate exchanged for a longer one. Bone grafting was added in nine patients. Union was achieved in all patients 8–16 weeks after re-operation. This work is a message for timely surgical interference in delayed union after bridge-plate fixation by a limited surgical procedure, before complete failure of the fracture stabilisation or non-union.
Résumé
Malgré le développement des différents traitements, un certain nombre de pseudarthroses sont encore rencontré dans les fractures des os longs des membres. Le but de ce travail est d’évaluer la prise en charge de ces retards de consolidation après fixation par plaque de fractures diaphysaires multi fragmentaires. 19 patients ont été inclus pour ce travail. Ils ont bénéficié d’une reprise chirurgicale pour retard de consolidation après fixation par plaque. Le temps moyen entre l’intervention primaire et la révision a été de 12 à 20 semaines. Dans tous les cas il a été nécessaire d’augmenter la stabilité par l’addition de vis complémentaires. La compression inter fragmentaire a été réalisée chez 16 patients, une compression axiale chez 2 patients et un changement de plaque chez un patient. Une greffe a été nécessaire chez 9 patients. La consolidation a été totale chez tous les patients à 16 semaines après la réintervention. Ce travail a pour but de donner une information concernant l’algorithme chirurgical lorsqu’il existe un défaut de consolidation après ostéosynthèse par plaque.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intramedullary nailing is now the standard method of fixation for diaphyseal fractures. The plate fixation of multifragmentary fractures is, however, still a common practice in many centres due to patient considerations or the available facilities [10].
Despite recent developments in fracture treatment, cases of delayed and non-union after long bone fractures are still encountered. Prolongation of the healing time of fractures has a deleterious effect on the patient’s limb, body, socioeconomic and psychological status. Better understanding of the mechanics of fracture stabilisation and of the biological requirements of fracture healing has improved the outcome in these difficult cases [3, 4].
The aim of this work is to show the results of the active management of delayed union after the bridge-plate fixation of multifragmentary diaphyseal fractures by a limited surgical interference, before it proceeds to established non-union or complete failure of the fracture stabilisation.
Patients and methods
We followed 19 patients who had a second operation for delayed union of multifragmentary diaphyseal fractures in the authors’ institution from January 2004 to December 2006. The patient age ranged between 22 and 52 years (average 39 years); there were 15 males and four females.
Inclusion criteria
Patients were included if they experienced delayed union of multifragmentary diaphyseal fractures that were treated by the bridge-plate technique. The decision to re-operate was taken 12 to 20 weeks (average 15 weeks) after the primary surgery if there was no progress in the fracture healing. The presence of pain and local tenderness at the fracture site, with a lack of bridging callus, or the presence of a fracture gap in the anteroposterior and lateral X-ray views were considered to be clinical and radiological warning signs of delayed union. Fourteen fractures were femoral and five were tibial. According to the AO fracture classification, 14 were type B wedge fractures and five were type C complex fractures. Seven fractures were initially open. The possibility of infection was ruled out, clinically, radiologically and by laboratory studies.
Medial thigh pain, distal to the fracture site, was reported in one patient due to a malreduced medially pointing fracture fragment.
Surgery was performed through part or all of the original incision opposite the delayed union site with minimal soft tissue stripping.
Increasing the stability of the fixation was achieved by the following techniques:
-
1.
Adding more screws on one or both sides of the main fracture line in all cases.
-
2.
Interfragmentary compression was achieved by inserting lag screws, through the plate or outside it, between the main bone fragments or to fix a major wedge fragment, in 16 patients (Fig. 1). Lag screws were introduced blindly, guided by the preoperative and intraoperative X-rays. They were introduced without any soft tissue stripping, as there was no need to hold the fragments with a bone forceps or to use any Hohmann’s retractors. This depended on the fact that the fragment, by that time, is usually fairly fixed to the surroundings by good fibrous tissue.
-
3.
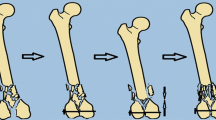
Axial compression of the fracture was carried out in two patients with a gap between the two main fracture fragments. This was applied by the removal of the screws from one side of the plate, compression of the fracture site and then reinsertion of a set of new screws (Fig. 2).
-
4.
Exchanging the plate with a longer one was performed in one patient.
a, b A multifragmentary fracture of the left femur 12 weeks after the first operation showing delayed healing. The patient also complained of discomfort on the medial side of the thigh due to medially pointing bone fragments. c, d Showing union 8 weeks after re-operation by the insertion of two lag screws through the plate to pull the wedge fragments and fix them to their bed, and the addition of iliac bone graft. The medial thigh pain disappeared
a, b Multifragmentary femoral shaft fracture that did not unite in 12 weeks. There are appreciably large posteromedial wedge fragments which are kept away from their bed by muscle pull. There is one screw at the fracture site keeping the bones apart. c, d Bony union 16 weeks after re-operation. Surgery included replacing the distal screws after the application of axial compression, changing the screw at the fracture site and the addition of two lag screws to the wedge fragments pulling them back to their bed
In nine patients, it was judged that there was a need to stimulate osteogenesis due to the presence of bone gap. Shingling, raising osteoperiosteal flaps close to the main fracture line, in addition to local bone grafting, was carried out in five patients, and iliac bone grafting was added in four patients.
Post-operative management
Hip and knee range of motion exercises and muscle strengthening were instructed for the entire extremity. Touchdown weight bearing was permitted for the first 6 weeks after surgery, and then progression to full weight bearing according to the bridging callus seen on the radiographs.
Follow-up
After hospital discharge, the patients were observed periodically every 4–6 weeks until the healing of the fracture. Fracture union was diagnosed clinically when the fracture site was painless and radiologically if solid callus formation was seen on the anteroposterior and lateral views. The follow-up period ranged from 48 to 96 weeks (average 64 weeks).
Results
All fractures united without the need for further operative procedures. The time to fracture healing ranged from 8 to 16 weeks (average 11 weeks).
Discussion
The treatment of diaphyseal fractures appears to be relatively straightforward, with a low risk of failure. However, most studies are published by specialised trauma centres that usually treat a large number of shaft fractures per year with a high institutional learning curve. So, the incidence of fixation failure and non-union published in the literature may be somewhat lower than the daily orthopaedic reality. Additionally, because of the relatively low rate of failure, a small number of surgeons have significant experience with the salvage of failed fixation [13]. Non-union is defined chronologically as a fracture that does not unite in 6 months or biologically when the healing process is lingering behind the expected rate. A delayed union was defined as the absence of radiographic progression of healing or an unstable fracture on clinical examination between 4 and 6 months after injury [11, 12].
Delayed and non-union result from devitalisation of the bone by trauma or surgery, lack of adequate stabilisation of the fracture or excessive stresses at the fracture site, e.g. early weight bearing. Excessive stresses have to be reduced to an amount that stimulates healing, without excessively straining the fracture site. Other factors resulting in non-union include fracture comminution, bone defects and local infection. These factors need to be addressed. The patients need to be evaluated for co-morbid conditions, such as diabetes, malnutrition and immunocompromised states [1].
Primary plate fixation of multifragmentary fractures
The principle of bridge plate [2, 6, 7, 14] was introduced to avoid the direct manipulation of bone fragments and stripping them of their soft tissue attachment. Minimally invasive plate osteosynthesis (MIPO), in addition, avoids disturbance of the injury zone altogether [4, 5, 8, 15]. Major bone fragments usually retain muscular attachment and, if they are not stabilised, they continue flipping by contraction of the attached muscles, interfering with the union. The bridge plate and the MIPO technique pay all of their attention to biology, however, in multifragmentary fractures with an appreciable wedge fragment, a balance between biology and mechanics should be the goal. Thus, a major bone fragment should be stabilised by one or, preferably, two lag screws, through the plate or outside it, to the main bone fragments. This should be achieved with minimal dissection or stripping, even without anatomical reduction. It may even be performed blindly through a stab wound in the overlying muscle.
Re-operation for delayed union after bridge-plate fixation
Early hardware failure within 6 months of surgery is usually due to problems in technique. Plating failures occur from an inadequate screw number, lack of compression and short or undersized plates. In salvaging early hardware failures, the key principle is to analyse the cause of failure so as not to repeat or create new problems during the revision procedure. No specific literature was found addressing the precise timing to avoid fixation failure [9].
The decision to re-operate in multifragmentary diaphyseal fractures should be taken early, probably at about 12 to 20 weeks, if it is thought that healing is not progressing at the expected rate. Further delay may lead to breakage of the plate through cyclic bending, or loosening or pulling out of the screws, which necessitate the removal of all hardware and repeating the fixation. Delay will also result in osteoporosis, especially of the distal fragment, adding greater difficulty to the problem. Timely surgical intervention may be needed to augment mechanical stability and/or stimulate osteogenesis. The fracture pattern at re-operation differs from that in the first operation. Most of the small bone fragments would have united to one of the main bone fragments, making the insertion of additional screws possible. Frequently, exuberant non-bridging callus has formed, which could be used as local bone graft.
In this study, re-operation was usually in the form of a limited surgical procedure to augment stabilisation and, sometimes, to add bone graft. Exceptionally, all hardware had to be removed and the stabilisation repeated. Interfragmentary compression could be applied by inserting lag screws, through the plate or outside it, between the main bone fragments or to fix a major wedge fragment to one or both main fragments. Lag screws were introduced without soft tissue stripping, as there was no need to hold the fragment with bone forceps or use a Hohmann’s retractor, taking advantage of the fact that the fragment is, by now, fairly fixed to its surroundings by fibrous tissue. The aim was to approximate and fix the wedge fragment to its bed, to add to the stability and share in the healing process.
The limitations of this study are the retrospective design, the lack of a control group with similar inclusion criteria to compare the outcomes and the possible selection bias, as neither precise time nor selection criteria were found in the literature to define intervention in delayed union after bridge-plate fixation.
However, these limitations do not undermine the value of the study, as it is an attempt to highlight the timing and possible methods of intervention of delayed union after the bridge-plate fixation of multifragmentary diaphyseal fractures.
Conclusion
This work is a message to actively manage delayed union after bridge-plate fixation by a limited surgical interference, saving time and increasing the chances of union and avoiding the consequences of protracted healing.
References
Babhulkar S, Pande K, Babhulkar S (2005) Nonunion of the diaphysis of long bones. Clin Orthop Relat Res 431:50–56
Baumgaertel F, Gotzen L (1994) The “biological” plate osteosynthesis in multi-fragment fractures of the para-articular femur. A prospective study. Unfallchirurg 97(2):78–84
Blatter G, Gasser B, Weber BG (1986) Die Wellenplatte. AO Bull 1:3–5
Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H (1999) Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma 13(6):401–406
Farouk O, Krettek C, Schandelmaier P, Said GZ, Tscherne H (1999) Anatomic basis of minimally invasive plate osteosynthesis in the femur. Tech Orthop 14(3):158–169
Gautier E, Ganz R (1994) The biological plate osteosynthesis. Zentralbl Chir 119(8):564–572
Müller ME, Allgöwer M, Schneider R, Willenegger H (1991) Manual of internal fixation: techniques recommended by the AO-ASIF group, 3rd edn. Springer, Berlin Heidelberg New York
Pai V, Coulter C, Pai V (2007) Minimally invasive plate fixation of the tibia. Int Orthop 31(4):491–496
Richter J, Schulze W, Muhr G (2000) Diaphyseal femur pseudarthroses—only a technical problem? Chirurg 71:1098–1106
Riemer B (2004) Plating diaphyseal fractures. Tech Orthop 18(4):360–367
Ring D, Barrick WT, Jupiter JB (1997) Recalcitrant nonunion. Clin Orthop Relat Res 340:181–189
Ring D, Kloen P, Kadzielski J, Helfet D, Jupiter JB (2004) Locking compression plates for osteoporotic nonunions of the diaphyseal humerus. Clin Orthop Relat Res 425:50–54
Smith WR, Morgan SJ (2002) Failure of internal fixation of the femoral shaft. Tech Orthop 17(4):448–457
Wenda K, Runkel M, Rudig L (1995) The “inserted” condylar plate. Unfallchirurgie 21(2):77–82
Wenda K, Runkel M, Degreif J, Rudig L (1997) Minimally invasive plate fixation in femoral shaft fractures. Injury 28(Suppl 1):A13–A19
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Said, G.Z., Farouk, O. & Said, H.G.Z. Delayed union of multifragmentary diaphyseal fractures after bridge-plate fixation. International Orthopaedics (SICOT) 33, 549–553 (2009). https://doi.org/10.1007/s00264-008-0528-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-008-0528-9