Abstract
Total hip arthroplasty (THA) still carries a higher failure rate in patients with avascular necrosis of the femoral head (AVN) than in a similar patient population with THA for other reasons. This is particularly true for the acetabular component. One of the major factors accounting for this is the compromised acetabular bone quality with structural defects subsequent to collapsing of the femoral head in high-grade AVN. In this study we implanted an acetabular reinforcement ring with hook (ARRH), which had been used successfully for other indications with acetabular bone stock deficiency, in 32 consecutive THA’s in 29 patients with AVN. Five patients died during the observation period of causes unrelated to the surgery, one patient was lost to follow-up and one patient could not be followed up due to chronic illness, leaving 25 hips (23 patients) with a minimum follow-up of ten years (mean: 11.8; range: 10–15). The mean Merle d’Aubigne score increased significantly from 7.7 preoperatively to 16.6 postoperatively (p < 0.001). One revision was performed for aseptic stem loosening. Of the unrevised hips, one acetabular component was classified as definitively loose. The cumulative 12-year survivorship for THA with ARRH in AVN was 95.2% (confidence interval: 86.1–100%) for both components, 100% for the cup and 95.2% for the stem (86.1–100%).
Résumé
Les prothèses totales de hanche posées chez les patients présentant une nécrose avasculaire de la tête fémorale présente un taux d’échec important, en particulier au niveau du composant acétabulaire. On comparera cette population à une population ayant bénéficié d’une prothèse totale de hanche pour les autres étiologies. La raison de ces échecs est la mauvaise qualité de l’os qui présente des défauts structuraux secondaires au collapsus de tête fémorale dans les nécroses de haut grade. C’est pour cette raison que nous avons implanté de façon à renforcer le côté acétabulaire des prothèses avec un implant de type Kerboul chez 29 patients ayant bénéficié de 32 prothèses totales de hanche. 5 patients sont morts durant la période de surveillance de ces prothèses, ceci sans aucune relation avec l’intervention chirurgicale, un patient a été perdu de vue, un patient n’a pu être suivi du fait de pathologies chroniques. Ont été analysé 25 hanches chez 23 patients avec un minimum de suivi de 10 ans, 11,8 ans en moyenne (de 10 à 15 ans). Le score de Merle d’Aubigné moyen s’est amélioré de 7,7 en pré-opératoire à 16,6 en post-opératoire (p < 0,001). Une révision a été réalisée (4%) pour un descellement aseptique de la pièce fémorale. Sur les prothèses non révisées, un composant acétabulaire a été considéré comme définitivement descellé (4,2%). La courbe de survie de ces patients à 12 ans est de 95,2% (intervalle de confiance 86,1% à 100%) pour les deux composants, de 100% pour la cupule et de 95,2% pour la pièce fémorale (86,1 à 100%).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Avascular necrosis of the femoral head (AVN) remains a challenging disease, as it usually leads to the destruction of the hip joint in young patients between their third and fifth decade of life. Despite attempts to preserve the hip joint in the early stages of the condition, total hip arthroplasty (THA) is indicated once the femoral head has collapsed and the hip joint has degenerated such that articulation is compromised. However, the results of THA, both with and without cement, generally have a less favourable outcome in patients with AVN than in those with the so-called idiopathic osteoarthritis despite improvements in cementing techniques and component design [18, 19]. Acetabular loosening remains one of the most frequent reasons for revision in long-term studies with or without cement in patients with AVN [2, 3, 6]. Contributing causes to the acetabular loosening are a high level of activity in younger patients and increased body weight; however, the reason for this higher failure rate are the often underestimated qualitative and quantitative acetabular deficiency subsequent to the collapsed femoral head, protected weight bearing during long periods, ongoing systemic disease and defects in mineral metabolism associated with the use of corticosteroids [22]. Consequently, long-term acetabular loosening remains a serious concern, and alternative methods for socket fixation have to be investigated [17].Reinforcement rings are frequently used in THA secondary to developmental dysplasia of the hip or in revision THA with compromised bone stock and large bone defects [8, 20, 21]. Therefore, the acetabular reinforcement ring with hook (ARRH) combined with a cemented all-polyethylene (PE) cup is performed routinely for patients with AVN at the author’s institution. The purpose of this study was to evaluate the long-term results of THA for the treatment of advanced AVN (Ficat stage 3 and 4 [5]), with special attention to the ARRH, and to compare the results with other acetabular implant failures reported in the literature.
Materials and methods
Patients
Thirty-two consecutive cases (29 patients) of THA performed for AVN between 1987 and 1993 were reviewed. Surgery was performed in ten women and 19 men, with an average age at surgery of 50.2 years (range: 31.0–78.7 years). The origin of necrosis was idiopathic in 16 hips (50%), posttraumatic in seven hips (21.9%), steroid-associated in six hips (18.8%) and alcohol-related in three hips (9.4%). Femoral head necrosis was categorised according to the classification of Ficat [5]: 17 cases were stage III (53.1%), and 15 cases were stage IV (46.9%). Thirteen patients (40.6%) had undergone previous surgery, such as fracture osteosynthesis (seven cases), intertrochanteric osteotomy (four cases) or intertrochanteric osteotomy with revascularization (two cases). A minimum follow-up of ten years was required for inclusion in the study group. Merle-d’Aubigne scores were evaluated preoperatively and at the latest follow-up [14]. By means of a questionnaire the patients were asked about their capacity to perform a variety of activities of daily living, the presence or absence of pain and their functional status. Table 1 presents an overview of all relevant data on the patients.
Surgical technique
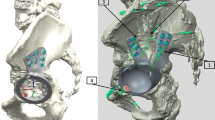
A lateral approach was adopted for surgery. Reconstruction of the acetabulum was achieved using the ARRH with a cemented PE cup in all patients. The ring consists of a titanium (Protema-Tcp) alloy with a smooth electro-polished surface without any on-growth potential (Zimmer, Warsaw, Ind., formerly Centerpulse, Winterthur, Switzerland; Fig. 1). The hook is first placed around the inferior margin of the acetabulum after the transverse acetabular ligament is exposed to prevent high or lateral placement of the ring. After careful acetabular reaming, the four 6.5-mm titanium fixation screws are positioned. The ARRH should be placed against the area of best bone stock because there is complete freedom to place the cemented PE cup in the optimal anatomical orientation during the cementing process (Fig. 1). Depending on the acetabular bone stock deficiency, structural or cancellous autograft can be placed behind the ring. Of the total ten hips with autografts in this study, cancellous bone was used in eight and structural autograft was used in two cases. In all but one hip a cemented stem (Protasul, Müller straight stem or lateralized; Zimmer) was implanted. One patient received a cementless Protasul Müller CDH femoral component (Zimmer). A 22-mm femoral metal head was used in 13 hips, a 32-mm head in ten hips and a 28-mm head for nine reconstructions. This depended on individual surgeon’s preference. In this series, the mean outer diameter of the ARRH was 52 mm (range: 50–58 mm), and the mean size of the PE inlay was 50 mm (range: 44–56 mm). In all hips, a non-cross-linked PE was used (Sulene-PE; Zimmer).
The orientation of the acetabular reinforcement ring with hook (ARRH) (Zimmer, Warsaw, Ind.) is less critical than the contact with bone because the cement-polyethylene (PE) interface allows a moderate amount of freedom to further improve the position of the cup for inclination (top) and version (bottom)
Postoperatively, all patients received prophylaxis for deep venous thrombosis with warfarin. All patients received antibiotic prophylaxis for the first 36 hours.
Radiographic evaluation
For radiographic evaluation of the loosening of the acetabular component, a special grading system was developed for the acetabular reinforcement rings and used in this series (Table 2) because standard methods are not applicable [20]. The presence and degree of acetabular migration were measured according to the system of Müller [15]. This method uses a horizontal line connecting the inferior margins of the acetabulum as a reference line for vertical migration, and a vertical line bisecting the inferior margin of the acetabulum is used as a reference for horizontal migration. Heterotopic ossification was evaluated according to the system of Brooker et al. [1]. The presence and progression of any acetabular or femoral osteolysis was also assessed according to the DeLee and Charnley zones [4] or the Gruen zones [9], respectively.
Statistical analysis
The Wilcoxon rank sum test was used to compare pre- and postoperative Merle d’Aubigné scores. Kaplan-Meier survivorship analysis was performed to determine the cumulative survival rate for the ARRH with revision of each component as the end point [11].
Results
Clinical results
Of the 32 hips operated on, 25 were available (22 patients) with a minimum follow-up of ten years (average: 11.8 years; range: 10–15 years). Five patients (five hips) died 0.4–8.2 years postoperatively of causes unrelated to the surgery. One patient could not be radiographically followed up because of chronic illness (latest follow-up: 6.1 years; Merle-d’Aubigne score: 17), and one was lost to follow-up (latest follow-up: seven years; Merle-d’Aubigne score: 18). Both of these two patients had no clinical problems at their latest follow-up.
The average Merle-d’Aubigne score of the remaining 25 hips increased from 7.7 preoperatively (range: 5–11) to 16.6 postoperatively (range: 13–18; p < 0.0001). Of these 25 hips, 23 (92%) were considered as good or excellent results, with a Merle-d’Aubigne score of 15 or more points (Fig. 2). The two cases with less than 15 points had no radiological signs of loosening, but heterotopic ossifications class II and III were present retrospectively, and one of them had a history of early dislocation.
a A 32-year-old patient (no. 4/5) with bilateral, steroid-induced avascular necrosis of the femoral head. Note the collapsed left femoral head with beginning erosion of the acetabulum. b One year after a two-staged total hip arthroplasty (THA) with cemented lateralised Müller straight stem and ARRH. c X-ray at the latest follow-up 11 years after THA. No signs of loosening can be observed. Clinically, a Merle-d’Aubigne score of 16 (left) and 17 (right) was achieved
Of the five deceased patients, at the time of their latest follow-up two showed a Merle-d’Aubigne score of 15 points after 5.9 years and 5.6 years, respectively, with no signs of implant loosening. No scores were available for the other three deceased patients.
Radiographic examination
One acetabular component with a cancellous bone graft was judged to be definitely loose with breakage of the hook, osteolysis around the screws and radiolucent lines 5.9 years postoperatively (Fig. 3). However,, at a follow-up of 13.5 years, the Merle-d’Aubigne score was 16. No revision has been required to date since the acetabular bone stock and implant have remained unchanged. None of the 24 remaining cups showed radiolucencies around the ring or screws, or migration of more than 2 mm in any direction.
This 53-year-old patient (no. 31) had an idiopathic avascular necrosis of the femoral head (AVN) on the left side. A substantial destruction of the femoral head and the acetabular side was observed preoperatively. On the right side, an uncemented Müller straight stem with a Müller reinforcement ring was performed years before due to the same disease. A cemented lateralised Müller straight stem and ARRH was implanted on the left side. Taken 13.5 years postoperatively, this X-ray shows a migration of the ARRH with breakage of the hook, which is a definite sign of loosening of the acetabular component. Since its first detection 5.9 years after operation, the radiological situation has remained unchanged, and at latest follow-up the patient had no clinical sings of loosening and had a Merle-d’Aubigne score of 16. No revision has been required to date
With respect to the 24 non-revised femoral components, two hips showed radiographic changes: in one hip stem, an initial subsidence of 5 mm was observed (uncemented stem) in the first postoperative period, but at 18 months postoperatively no more subsidence was noticed and the stem remained stable. The Merle-d’Aubigne score was 16 at the 13.5-year follow-up. In the other hip a circumscribed osteolysis (zone 7) was seen, even though the Merle-d’Aubigne score was 15 at the latest follow-up. None of the unrevised hips showed definitive radiological signs of stem loosening.
Signs of heterotopic ossification were observed in 11 cases and subsequently classified according to Brooker’s criteria. Class I was diagnosed in three hips, class II in three hips, class III in four hips and class IV in one hip. The latter had to be revised because of stem loosening (see below). Out of the ten unrevised patients, two had a fair result with a Merle-d’Aubigne score of 13 and14 points, respectively.
Revisions
The only revised hip had a previous history of osteosynthesis of an acetabular fracture with central dislocation of the femoral head. Consecutive revision was necessary for resection of heterotopic ossification (class III). One year after the accident, a THA was implanted for post–traumatic AVN. Stem loosening was apparent as early as one year postoperatively, with adjacent development of heterotopic ossification (class IV). Due to the minor symptoms, stem revision was performed only nine years after THA. The ARRH was stable during the intraoperative period and did not require exchange. No revision was necessary due to ARRH loosening in any of the 25 hips with a minimum follow-up of ten years.
With the revision of any component as the end point, the cumulative survival rate was 95.2% (confidence interval: 88.1–100%). With the revision of the ARRH as the end point, the cumulative survival rate was 100%.
Complications
There were three hips with dislocations. One early hip dislocation was observed two weeks postoperatively and treated successfully by closed reduction, even though the Merle-d’Aubigne score at the latest follow-up was only 13. In this patient, chronic pain was present with heterotopic ossification (Grade II) without any radiographical signs of acetabular or femoral component loosening. One patient sustained four dislocations four years postoperatively and one more dislocation 13 years postoperatively, all requiring closed reduction without a need for revision; at the follow-up of 14.7 years a Merle-d’Aubigne score of 16 was noted. Finally, another patient suffered from a traumatic hip dislocation five years postoperatively which also required closed reduction; the Merle-d’Aubigne score at the latest follow-up was 17. There were no deep infections.
Discussion
Early stages of AVN aim at procedures for preserving the hip joint, but end stage disabling collapse and destruction occur frequently. Despite alternative procedures THA remains the most widespread treatment for advanced AVN. Although there is ongoing improvement in cementing techniques and the design of prostheses, THA in patients with AVN still has higher failure rates than age-matched controls with other diagnoses. Both long-term and mid-term acetabular loosening are typical complications and remain a serious concern, with the supposed cause being attributed to the decreased qualitative and quantitative acetabular bone stock in AVN (Table 3). To the authors’ knowledge, this is the first report on long-term results on the use of the ARRH for this specific indication. In this series none of the 25 sockets required revision. There was only one revision necessary on the femoral side, and no further definitive radiological femoral loosening could be detected. One (4.2%) definite case of acetabular loosening was observed, without clinical symptoms, and there was no need for revision surgery. Bearing in mind the minimal follow-up of ten years (average: 11.9 years), these data on revision seem to be very low compared to other studies reported in literature (Table 3).
The authors believe that the high acetabular loosening rates in AVN may be due to poor bone stock. Acetabular subchondral sclerotic bone frequently decreases as a consequence of longstanding protected weight bearing due to pain or because of fast ongoing femoral head destruction. Further, femoral head collapse may lead to erosion and destruction of the acetabular socket [22] (Fig. 2a). Progressive associated osteoporosis or osteomalacia due to the different aetiological factors of the disease may be associated in patients with hemoglobinopathies, long-term alcohol abuse or corticosteroid medication. These factors may induce osteoporosis and potentially compromise consecutive healing of microfractures and thus facilitate subchondral fractures [10]. Kobayashi et al. recently assessed 405 primary Charnley THA patients to identify risk factors for aseptic fixation failures [12]. Preoperative diagnosis of atrophic osteoarthrosis (defined by rare osteophyte formation) was identified as a risk factor for socket loosening, and these researchers speculated that in such hips the acetabulum might not have been strong enough to prevent fatigue fracture or collapse of the cancellous bone. We believe that one of the major reasons for the reported acetabular loosening rate is the use of the ARRH providing good protection of the underlying bone stock through load distribution and minimal iatrogenic bone loss. Initial fixation is performed by multiple screws directed toward areas of the best host bone stock in the supra–acetabular region, thereby allowing a good stress distribution. Furthermore, the ARRH can be placed in a position deliberately in order to use optimal support from bone stock since the cemented PE cup still can be oriented differently with an optimal version and inclination.
This study has limitations, primarily consisting of the relatively small patient group and the lack of a control cohort. Also, in comparison to data from the literature, the average age of 50.2 years was relatively high in our patient group; although the data was consecutively collected, the young average age may favourably influence the revision and loosening rate. However, even in previous studies with a substantially older patient population, the acetabular revision rate was still significantly lower, indicating thereby the excellent outcome of this study for the ARRH.
There was a rather high rate of dislocations. In all three cases, a 22-mm head was implanted which will favour hip dislocation due to decreased head/neck diameter ratio. Since there is a relatively high degree of freedom to place the PE within the metal cage, it is conceivable that either anterior or posterior impingement can be the cause of dislocation. However, since this manoeuvre is tested intraoperatively, it is unlikely that an implant impingement represents the reason for dislocation.
Although THA in AVN remains a challenging treatment, good to excellent results can be achieved with the ARRH, as the results from this approach are comparable with cementless fixations at present. Compromised bone stock on the acetabular side probably plays an important role in cup loosening. We believe that the ARRH with cemented PE cup can potentially lead to favourable results because this approach takes the compromised acetabular bone stock situation into account. Its use is associated with a low rate of acetabular loosening for THA in AVN and represents an attractive alternative to cementless implants.
References
Brooker AF, Bowerman JW, Robinson RA, Riley LH (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg [Am] 55:1629–1632
D’Antonio JA, Capello WN, Manley MT, Feinberg J (1997) Hydroxyapatite coated implants. Total hip arthroplasty in the young patient and patients with avascular necrosis. Clin Orthop Relat Res 344:124–138
Delank KS, Drees P, Eckardt A, Heine J (2001) Results of the uncemented total hip arthroplasty in avascular necrosis of the femoral head (in German). Z Orthop Ihre Grenzgeb 139:525–530
DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 121:20–32
Ficat RP (1985) Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg [Br] 67:3–9
Fyda TM, Callaghan JJ, Olejniczak J, Johnston RC (2002) Minimum ten-year follow-up of cemented total hip replacement in patients with osteonecrosis of the femoral head. Iowa Orthop J 22:8–19
Fye MA, Huo MH, Zatorski LE, Keggi KJ (1998) Total hip arthroplasty performed without cement in patients with femoral head osteonecrosis who are less than 50 years old. J Arthroplasty 13:876–881
Gerber A, Pisan M, Zurakowski D, Isler B (2003) Ganz Reinforcement Ring for Reconstruction of Acetabular Defects in Revision Total Hip Arthroplasty. J Bone Joint Surg [Am] 85:2358–2364
Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 141:17–27
Kantor SG, Huo MH, Huk OL, Salvati EA (1996) Cemented total hip arthroplasty in patients with osteonecrosis. A 6-year minimum follow-up study of second-generation cement techniques. J Arthroplasty 11:267–271
Kaplan E, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Statist Assoc 53:457–481
Kobayashi S, Saito N, Horiuchi H, Iorio R, Takaoka K (2000) Poor bone quality or hip structure as risk factors affecting survival of total-hip arthroplasty. Lancet 355:1499–1504
Lee SB, Sugano N, Nakata K, Matsui M, Ohzono K (2004) Comparison between bipolar hemiarthroplasty and THA for osteonecrosis of the femoral head. Clin Orthop Relat Res 424:161–165
Merle d’Aubigné R, Postel M (1954) Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg [Am] 36:451–475
Müller ME (1989) Total Hip Arthroplasty. In Evarts CM (ed): Surgery of the musculoskeletal system. Churchill Livingstone, New York
Nich C, Courpied JP, Kerboull M, Postel M, Hamadouche M (2006) Charnley-Kerboull total hip arthroplasty for osteonecrosis of the femoral head a minimal 10-year follow-up study. J Arthroplasty 21:533–540
Nich C, Sariali el-H, Hannouche D, Nizard R, Witvoet J, Sedel L, Bizot P (2003) Long-term results of alumina-on-alumina hip arthroplasty for osteonecrosis. Clin Orthop Relat Res 417:102–111
Ritter MA, Meding JB (1986) A comparison of osteonecrosis and osteoarthritis patients following total hip arthroplasty. A long-term follow-up study. Clin Orthop Relat Res 206:139–146
Saito S, Saito M, Nishina T, Ohzono K, Ono K (1989) Long-term results of total hip arthroplasty for osteonecrosis of the femoral head. A comparison with osteoarthritis. Clin Orthop Relat Res 244:198–207
Siebenrock KA, Tannast M, Kim S, Morgenstern W, Ganz R (2005) Acetabular reconstruction using a roof reinforcement ring with hook for total hip arthroplasty in developmental dysplasia of the hip-osteoarthritis. Minimum 10-year follow-up results. J Arthroplasty 20:492–498
Siebenrock KA, Trochsler M, Sadri H, Ganz R (2001) Hooked roof cup in revision of difficult loose hip prosthesis cups. Results after a minimum of 10 years (in German). Orthopäde 30:273–279
Steinberg ME, Corces A, Fallon M (1999) Acetabular Involvement in Osteonecrosis of the Femoral Head. J Bone Joint Surg [Am] 81:60–65
Stulberg BN, Singer R, Goldner J, Stulberg J (1997) Uncemented total hip arthroplasty in osteonecrosis: a 2- to 10-year evaluation. Clin Orthop Relat Res 334:116–123
Taylor AH, Shannon M, Whitehouse SL, Lee MB, Learmonth ID (2001) Harris Galante cementless acetabular replacement in avascular necrosis. Journal Bone Joint Surg [Br] 83:177–182
Xenakis TA, Gelalis J, Koukoubis TA, Zaharis KC, Soucacos PN (2001) Cementless hip arthroplasty in the treatment of patients with femoral head necrosis. Clin Orthop Relat Res 386:93–99
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koch, P.P., Tannast, M., Fujita, H. et al. Minimum ten year results of total hip arthroplasty with the acetabular reinforcement ring in avascular osteonecrosis. International Orthopaedics (SICO 32, 173–179 (2008). https://doi.org/10.1007/s00264-006-0303-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-006-0303-8