Abstract
The OPG/RANK/RANKL system has been implicated in the biological cascade of events initiated by particulate wear debris and bacterial infection resulting in periprosthetic bone loss around total hip arthroplasties (THA). Individual responses to such stimuli may be dictated by genetic variation caused by single nucleotide polymorphisms (SNPs). Case control study of the osteoprotegerin and RANK genes for possible association with deep sepsis or aseptic loosening. All patients were Caucasian and had had a cemented Charnley THA and polyethylene acetabular cup. Cases consisted of 91 patients with early aseptic loosening and 71 patients with deep infection. Controls were 150 clinically and radiologically well-fixed THAs. DNA samples were genotyped using Taqman allelic discrimination. The A allele (p<0.001) and genotype A/A (p<0.001) for the OPG-163 SNP were associated with aseptic failure. Additionally, the RANK +575 (C/T SNP) T allele (p=0.004) and T/T genotype (p=0.008) frequencies were associated with aseptic failure. Comparing the septic group with the controls, the frequency of the A allele (p<0.001) and the genotype A/A (p<0.001) for the OPG-163 SNP were statistically significant. Aseptic loosening and deep infection of THA may be under the influence of susceptibility genes. SNP markers may serve as predictors of implant survival.
Résumé
Le système OPG/RANK/RANKL est impliqué dans la cascade des événements initiés par les débris d’usure et l’infection, conduisant à l’ostéolyse périprothètique de la hanche. La réponse individuelle est peut-être génétique, à cause du polymorphisme des nucléotides (SNPs). étude, avec groupe contrôle, des gènes RANK et ostéoprotégérine, et de l’association possible avec l’infection ou le descellement aseptique. Tous les patients étaient caucasiens et avaient eu une prothèse totale de hanche type Charnley avec cupule en polyéthylène. Il y avaient 91 patients avec un descellement aseptique précoce et 71 avec une infection profonde. Le groupe contrôle était constitué de 150 arthroplasties bien fixées cliniquement et radiologiquement. Les échantillons d’ADN étaient génotypés en utilisant la discrimination allèlique Taqman. L’allèle A (p<0,001) et le génotype A/A (p<0,001) pour l’OPG-163SNP était associé avec un échec aseptique. De plus, l’allèle RANK+575 (C/T SNP) T (p=0,004) et le génotype T/T étaient associés a l’échec aseptique. Entre le groupe septique et le groupe contrôle , la fréquence de l’allèle A (p<0,001) et du génotype A/A (p<0,001) pour l’OPG-163SNP était statistiquement différente. Le descellement aseptique et l’infection profonde d’une arthroplastie totale de la hanche peuvent être sous l’influence d’une susceptibilité génétique et les marqueurs spécifiques peuvent servir d’éléments prédictifs de la survie de l’implant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total joint replacement is one of the most innovative, cost-effective, and successful procedures in modern medicine. Function and mobility have been restored to millions since its advent over 30 years ago. The failure of total hip arthroplasty (THA) due either to aseptic loosening or deep bacterial infection is characterised by progressive bone loss and osteolysis [8]. The goal, in seeking a better understanding of the mechanism of osteolysis, is to reduce wear-related complications after total joint arthroplasty. This goal can be approached by efforts to reduce particle generation and to inhibit the biological response to particulate debris. Susceptibility to osteolysis is probably due to a combination of environmental and genetic factors, as progression of loosening and osteolysis varies between individuals with apparently identical total joint replacements. Environmental factors include the design of prostheses used, materials used, and surgical technique. These areas have been extensively studied and can explain the onset of osteolysis in certain situations [1].
Analysis of periprosthetic material and experimental models of debris-induced osteolysis have implicated osteoclasts as being central to the development of osteolysis [1]. The differentiation and function of osteoclasts is tightly coupled to the bone-forming cells (osteoblasts) since formation of the osteoclasts is not possible without co-culture of osteoblasts and monocytes [22]. The method of coupling has been identified as the receptor/activator of nuclear factor-κβ, its ligand, and the osteoprotegerin (RANK/RANKL/OPG) system [4]. This system plays an important role in osteolysis associated with inflammatory arthritis and tumour-mediated bone loss [12, 13]. OPG decreases the level of osteoclast formation and may cause severe osteopetrosis [21].
The RANK/RANKL/OPG system has been directly implicated in the development of osteolysis around THAs. In vitro experiments using cells retrieved from interface tissue demonstrated induction of RANK and RANKL mRNA by both wear particle and lipopolysaccharide endotoxin stimulation [9]. Activated cells in the interface membrane of failed THAs overproduce both RANKL and RANK [18]. The expression of RANK, RANKL, and OPG in the interface membrane of both aseptic and septic loosened THAs has implicated this system as being central to the mechanism of bone loss [6].
OPG and RANK have been investigated as candidate genes for the development of diseases characterised by increased osteoclast activity, such as Paget’s disease and osteoporosis [18, 23]. To investigate the association with osteolysis in aseptic and septic loosening of THAs, we chose to study three informative single nucleotide polymorphisms (SNPs) that, as demonstrated in previous studies [2, 17], may have possible effects on gene function: an A/G SNP at position −163 in the promoter (OPG-163), a T/G SNP at position −245 in the promoter (OPG-245), and a G/C SNP at position +1181 in the first exon, which causes a shift in codon 3 from lysine to asparagine (OPG +1181). Within the RANK gene comprising the promoter and 10 exons with surrounding intron sequences, a C/T SNP at position 575 (RANK +575) in exon 6 causes a shift in codon 2 from valine to alanine and as such may have a functional effect on the protein product and has also been included in our study [23]. Previous association studies have demonstrated positive findings between the presence of these SNPs and osteoporosis, and given the apparent central role of OPG/RANK in the development of periprosthetic osteolysis, we have used a case-control approach to examine the above proposed functional candidate SNPs for association with either aseptic or septic loosening of THAs.
Patients and methods
Patients
All patients were recruited from outpatient clinics between August 2002 and August 2004. Strict inclusion and exclusion criteria were set for the study groups (aseptically loosened or deeply infected THAs) and the control group (well-fixed implants) to make them directly comparable and to exclude possible biasing environmental risk factors. Only Caucasian patients of either sex with a primary diagnosis of osteoarthritis were included. All had a cemented Charnley monoblock femoral stem and either a cemented Charnley or Ogee flanged polyethylene acetabular cup. All patients with hip joint degeneration due to secondary causes and inflammatory or septic arthritis were excluded.
The aseptic study group consisted of subjects who had early loosening of prosthetic implants. Early aseptic loosening for both components was defined as that occurring within six years of implantation in line with the yearly incidence of loosening in relation to the evolution of the Charnley low-friction arthroplasty [19]. Only prostheses with no evidence of malposition and complete cement mantles were included. None had clinical, haematological, biochemical, microbiological, or operative findings suggestive of infection at the time of revision surgery. Femoral stem aseptic loosening was defined either by findings at revision surgery, the definite radiographic loosening criteria of Harris et al. [8], or progressive endosteal cavitation across zones as described by Gruen et al. [7]. Demarcation of acetabular components was recorded as per the zones described by DeLee and Charnley [5], and loosening was confirmed either at the time of revision surgery or by using the criteria of Hodgkinson et al. [10].
Well-fixed control THAs were defined as those that had remained clinically asymptomatic for over ten years and demonstrated none of the described radiographic features of aseptic loosening as described above or any “at risk” signs as described by Wroblewski et al. [19].
The septic (deep infection) group consisted of subjects who had developed proven deep bacterial infection of a THA at the time of revision surgery.
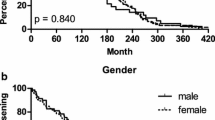
In total, 312 successive patients were recruited into the trial (150 controls, 91 aseptic cases, and 71 septic cases). The mean age of all patients was 68.6 years (70.9 in the control group, 66.2 in the aseptic group, and 68.7 in the septic group) with a range of 29–92 and SD of 7.8. In total, 163 women and 149 men were recruited. The differences in age and gender between the groups were not statistically significant.
Average length of survival for controls was 14.6 years. Average time to aseptic loosening was 5.1 years. Average time to first diagnosis of infection (either clinical or radiological) was 0.83 years. The infecting organism was a coagulase-negative staphylococcus in 69%, Staphylococcus aureus in 14%, streptococcus in 6%, E. coli in 6%, and other bacteria in 5%.
DNA extraction
Five milliliters of peripheral venous blood was collected into EDTA bottles from each subject by a standard venesection technique and was stored at -20ºC. DNA was extracted from pelleted white blood cells using phenol and ethanol. Concentrations of DNA were measured using a PicoGreen assay technique and diluted to 20 ng/μl with sterile water.
Genotyping
All SNPs were ABI typed using a TaqMan allelic discrimination assay developed for use on the 7,700 instrument (PE/Applied Biosystems, USA). For the OPG-163, OPG-245, and RANK+575 SNPs, assay-by-design Taqman assay reagent kits containing one pair of polymerase chain reaction (PCR) primers and one pair of fluorescently labeled Taqman probes were used (Applied Biosystems, CA, USA).
PCR was performed in 5-μl reaction volumes in 96 well plates and contained 10 ng genomic DNA per reaction. The standard protocol provided with the kit was followed. Thermocycler conditions were an initial 10-min denaturation at 95°C followed by 40 cycles at 95°C for 15 s and 60°C for 1 min. Available primer sequences for PCR were as follows: OPG-163—Forward GGACCACACTTTACAAGTCATCAAG/Reverse TGCTCTAGGGTTCGCTGTCT; OPG-245-Forward ACCCTAGAGCAAAGTGCCAAACT/Reverse AGGGCTATTGGTATCGGAGCTT; RANK+575-Forward AGAGTAGAACATCATGGGACAGAGA/Reverse GTGGTTTTCTAGCTGGCAGAGA.
Probe sequences for each SNP were as follows: OPG-163 (RS3102725)-VIC-CCCCATTAATTCCCT-MGBNFQ/6FAM-CCCATCAATTCCCT-MGBNFQ; OPG-245 (RS2073617)-VIC-CTTCTGGAGTAGCCTC-MGBNFQ/6FAM-CTTCTGGAGTCGCCT-MGBNFQ; RANK+575-VIC-AACTGCAAACCGCATCG-MGBNFQ/6FAM-AACTGCAAACCACATCG-MGBNFQ. For the OPG+1181 SNP (RS2073618), an assay-by-demand (Applied Biosystems reference number C_1971047_1) was used, details of which can be found at the company Web site [14]. The RS number is used as a means of integration with other National Center for Biotechnology Information (NCBI) sources for use in their publicly accessible Web-based database (http://www.ncbi.nlm.nih.gov/).
Reporter fluorescence emission was detected by an AB7700 fluorescent plate reader using Sequence Detection Software (Applied Biosystems, USA) for allele calling.
Statistical analysis
For each SNP the STATA 8.0 statistical analysis program (STATA Corporation, Texas, USA) was used to calculate the distribution of allele frequencies between subjects and controls and compared using the chi-square test. Odds ratio (OR) and 95% confidence intervals (CI) were also calculated. Based on published allele frequencies, an OR of 2, and 80% power with a 5% significance level, the numbers recruited were adequate.
Results
Genotype frequency distributions were in Hardy-Weinberg equilibrium for all four SNPs in cases and controls. Allele and genotype frequencies for controls and aseptic and septic failures are given in Table 1.
The frequency of the A allele (p=0.001, OR=3.76, 95% CI 2.31–6.11) and homozygous genotype A/A (p=0.001) for the OPG-163 SNP were highly associated with aseptic failure compared with the controls. Additionally, the RANK+575 C/T SNP T allele (p=0.004, OR=1.77, 95% CI=1.20–2.59 ) and T/T genotype (p=0.008) frequencies were associated with aseptic failure. No statistically significant relationship was found between aseptic loosening and the OPG-245 or OPG+1181 SNPs.
With regard to the septic group compared with the controls, the frequency of the A allele (p=0.001, OR=3.42, 95% CI=1.98–5.91) and homozygous genotype A/A (p=0.001) for the OPG-163 SNP were statistically significant. No statistically significant relationship was found between septic failure and the OPG-245, OPG+1181, or RANK+575 SNPs.
Discussion
Genetic and functional experiments by numerous groups indicate that the balance between RANKL-RANK signalling and the levels of biologically active OPG regulate development and activation of osteoclasts and bone metabolism [9, 12, 17]. Inhibition or increase in bone resorption via osteoclasts occurs via regulation of RANK/RANKL and OPG. Numerous cytokines have been associated with the pro-inflammatory cascade that is thought to be induced by wear particles or bacterial infection and that ultimately leads to periprosthetic bone loss [15]. The RANK/RANKL/OPG system is a potential candidate gene system because it is the final common pathway by which these cytokines mediate their effects on bone metabolism, making this system an attractive target for the prevention of pathological bone loss [20].
RANKL is expressed on the surface of osteoblasts and directly stimulates the differentiation of osteoclast progenitor cells into osteoclasts. This signalling is mediated via the binding of RANKL to RANK, which is expressed on the surface of precursors of osteoclasts and mature osteoclasts. OPG negatively regulates RANKL signalling and blocks osteoclast differentiation by acting as a soluble decoy receptor to RANKL and competes with RANK for RANKL binding [12].
Langdahl et al. [16] and Arko et al. [2] examined the promoter and the five exons with surrounding intron sequences of the OPG gene for SNPs and found 12, of which two sets of four and five were in complete linkage.
In this study we have attempted to investigate whether proposed functional polymorphisms in the OPG and RANK genes are associated with failure of THA. The OPG promoter SNPs could influence transcription and thus the level of OPG protein produced, and the RANK SNP could affect the function of the protein product. Both the OPG-163 and RANK+575 SNPs are significantly associated with aseptic failure, and the OPG-163 SNP was significantly associated with a deep infection. It would appear that there is a strong relationship between the A allele and osteolysis due to both aseptic and septic failure. It is perhaps not surprising that both types of failure have such an association given that although the initial stimuli are different, the clinical phenotype is similar in the type and extent of bone loss.
Association studies can be very useful in elucidating the relationship between complex disease phenotype and a specific genotype. However, they have a number of caveats such as small sample size, population stratification, and linkage disequilibrium. We have managed to collect a large number of study and control cases with approximately twice as many controls as study subjects in the aseptic group. Slightly fewer septic cases were recruited, which probably represents its lower prevalence.
Stringent recruitment criteria were employed in an attempt to avoid population stratification. Only patients with the same diagnosis, of the same ethnicity, and with the same implant and method of implantation were recruited. The distinction between controls and study subjects was done by using strict clinical and radiological criteria.
In this study we looked only at variation within the OPG and RANK genes. The biological effects of OPG are antagonistic to RANKL, as it acts as a decoy molecule. It is the ratio of RANKL to OPG that regulates osteoclast survival, differentiation, and activity. It will be important in the future to assess the effect of polymorphisms in the RANKL gene and compare OPG/RANKL/RANK haplotypes to gain a fuller picture of the effect of variation in the whole of this system.
The discovery of putative genetic effects on the survival of THAs represents a novel method of investigating the basic science behind prosthetic failure and a potential answer to the common scenario of such failure, which cannot be explained by mechanical, technical, or environmental factors. Any such genetic component is likely to be complex in nature and dependent upon numerous gene pathways. It is known that other systemic and local factors can modulate expression of OPG and RANKL and thus have an effect upon osteoclast activity and bone resorption. Such factors include interleukin-1, tumor necrosis factor-alpha, bone morphogenic protein-2, and prostaglandin E2 [11]. The identification of these new pathogenetic mechanisms of total hip replacement failure make new indicators of disease susceptibility and prognosis plus new drug targets direct possibilities. The possibility of attenuating the biological response to the development of aseptic loosening or deep infection around THAs remains a goal. One group has produced promising results using soluble RANK:Fc (a molecule that blocks RANK), which suggests that such a blockade may prevent or ameliorate wear debris-induced osteolysis by osteoclast depletion without inhibiting osteogenesis [3].
References
Archibeck MJ, Jacobs JJ, Roebuck KA, Glant TT (2001) The basic science of periprosthetic osteolysis. Instr Course Lect 50:185–195
Arko B, Prezelj R, Komel A, Kocijancic A, Hulder P, Marc J (2002) Sequence variations in the osteoprotegerin gene promoter in patients with postmenopausal osteoporosis. J Clin Endocrinol Metab 87(9):4080–4084
Childs LM, Paschalis EP, Xing L et al (2002) In vivo RANK signalling blockade using the receptor activator of NK-kappaB: Fc effectively prevents and ameliorates wear debris-induced osteolysis via osteoclast depletion without inhibiting osteogenesis. J Bone Miner Res 17:192–199
Clohisy D (2003) Cellular mechanisms of osteolysis. J Bone Joint Surg [A] 85(Suppl 1):4–6
DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 121:20–32
Gehrke T, Sers C, Moraweitz L et al (2003) Receptor activator of nuclear factor kappaB ligand expressed in resident and inflammatory cells in aseptic and septic prosthetic loosening. Scand J Rheumatol 32(5):287–294
Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop 141:17–27
Harris WH, McCarthy JC, O’Neill DA (1982) Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Joint Surg [A] 7:1063–1067
Haynes DR, Crotti TN, Potter AE et al (2001) The osteoclastogenic molecules RANKL and RANK are associated with periprosthetic osteolysis. J Bone Joint Surg [B] 83:902–911
Hodgkinson JP, Shelley P, Wroblewski BM (1988) The correlation between the roentographic appearance and the operative findings at the bone-cement junction of the socket in Charnley low-friction arthroplasties. Clin Orthop 228:105–109
Hofbauer LC, Kholsa S, Dunstan CR, Lacey DL, Boyle WJ, Riggs BL (2000) The roles of osteoprotegerin and osteoprotegerin ligand in the paracrine regulation of bone resorption. J Bone Miner Res 15:2–12
Holstead Jones D, Kong Y-Y, Penninger JM (2002) Role of RANKL and RANK in bone loss and arthritis. Ann Rheum Dis 61(Suppl 2):32–39
Honore P, Luger NM, Sabino MA et al (2000) OPG blocks bone cancer-induced skeletal destruction, skeletal pain and pain-related neurochemical reorganization of the spinal cord. Nat Med 6:521–528
Konttinen YT, Xu J-W, Patiala H et al (1997) Cytokines in aseptic loosening of total hip replacement. Curr Orthop 11:40–47
Langdahl BL, Carstens M, Stenkjaer L, Eriksen EF (2002) Polymorphisms in the osteoprotegerin gene are associated with osteoporotic fractures. J Bone Mineral Res 17(7):1245–1255
Mandelin J, Li T-F, Liljestrom M et al (2003) Imbalance of RANK/RANKL/OPG system in interface tissue in loosening of total hip replacement. J Bone Joint Surg [B] 85:1196–1201
Ohmori H, Makita Y, Funamizu M et al (2002) Linkage and association analyses of the osteoprotegerin gene locus with human osteoporosis. J Hum Genet 47:400–406
Pacheco V, Shelley P, Wroblewski BM (1988) Mechanical loosening of the stem in Charnley arthroplasties. J Bone Joint Surg [B] 70:596–599
Ross FP (2000) RANKing the importance of measles virus in Paget’s disease. J Clin Invest 105:555–558
Simonet WS, Lacey DL, Dunstan CR et al (1997) Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell 89:309–319
Suda T, Takahashi N, Martin TJ (1992) Modulation of osteoclast differentiation. Endocr Rev 13:66–80
Wuyts W, Van Wesenbeck L, Morales-Piga A et al (2001) Evaluation of the role of RANK and OPG genes in Paget’s disease of bone. Bone 28(1):104–107
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00264-007-0473-z
Rights and permissions
About this article
Cite this article
Malik, M.H.A., Bayat, A., Jury, F. et al. Genetic susceptibility to hip arthroplasty failure—association with the RANK/OPG pathway. International Orthopaedics (SICO 30, 177–181 (2006). https://doi.org/10.1007/s00264-006-0074-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-006-0074-2