Abstract
Between 1993 and 2002, we treated 43 patients with malignant musculoskeletal tumours of the knee region. All patients had partial resection of the femur or tibia together with endoprosthetic replacement. We were able to follow-up 23 patients with an average follow-up of 30 (12–97) months. Complications occurred in ten cases, of which one was a case of local recurrence. Most of the patients were completely satisfied with their condition, with a decreased walking distance as the only notable restriction. There was no correlation between the functional outcome and life quality assessment and the type of the implanted prosthesis, length of resected bone and type of resection. However, patients with tumours in the distal femur had significantly better functional and life quality outcome than those with a proximal tibial tumour.
Résumé
Entre 1993 et 2002 nous avons traité 43 malades avec une tumeur musculo-squelettique maligne de la région du genou. Tous les malades avaient une résection partielle du fémur ou du tibia avec remplacement prothétique. Nous avons suivi 23 malades avec un délai moyen de 30 (12–97) mois. Des complications se sont produites dans 10 cas dont une récidive locale. La plupart des malades ont été satisfaits du résultat avec un périmètre de marche diminué comme seule restriction notable. Il n’y avait aucune corrélation entre, d’une part les résultats fonctionnels et la qualité de vie et, d’autre part, le type de résection, la longueur de résection osseuse et le type de prothèse implantée. Cependant, les malades avec une tumeur du fémur distal avaient de meilleurs résultats pour la fonction et la qualité de vie que ceux atteints d’une tumeur du tibia proximal
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Longer survival of those suffering from malignant musculoskeletal tumours not only supports the decision for limb-saving surgery but also necessitates assessment of life quality and functional results. In the literature, comparison of different surgical techniques (amputation vs endoprosthesis; arthrodesis vs endoprosthesis) can be found [7, 8]. Articles discussing the results of limb-saving operations have also appeared in the last few years. Here we report the outcome of endoprosthetic reconstruction of tumours in the knee region performed at our clinic from 1993 until 2002.
Materials and methods
Between 1993 and 2002, we treated 43 patients with malignant musculoskeletal tumours of the knee region in the orthopaedic clinic of Semmelweis University using limb-saving surgery and endoprosthetic replacement. We were able to follow-up 23 patients, as 16 had succumbed to their malignant disease and four could not be traced. In 22 patients, we implanted a modular tumour endoprosthesis (16 cementless Howmedica HMRS prostheses and six cemented Protetim prostheses) while one had a rigid prosthesis and was therefore excluded from the study. Osteosarcoma, chondrosarcoma and carcinoma metastases were the most frequently found tumours.
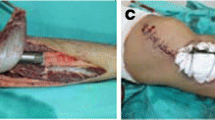
The average age at the time of surgery was 24.8 years. There were 12 female and ten male patients. Thirteen patients had a distal femoral tumour and eight had a proximal tibial tumour. All had a wide resection, 18 being intra-capsular and the remaining four extra-capsular. The length of the resected bone averaged 14.5 cm. The extensor mechanism was repaired by suturing the patellar ligament directly to the rotated muscle flap. In one case with a distal tibial tumour, the prosthesis was covered by a rotation flap from the medial head of the gastrocnemius muscle, as described by Malawer and McHale [12]. The average follow-up was 30 (12–97) months (Fig. 1).
At follow-up, we conducted a physical and radiographical examination. Tumour status, signs of local recurrence and septic or other complications were registered. The functional results were assessed by using Enneking’s criteria [4]. For the evaluation of life quality, the Oxford Knee Questionnaire was used [3]. We used five out of 12 questions and judged them to represent the entire questionnaire (Table 1).
We correlated functional results and life quality score to the type of resection (intra- or extra-capsular), length of resection, type of prosthesis, and tumour site. Statistical analysis was performed using the Mann–Whitney test.
Results
Of the 24 patients with osteosarcoma, 14 had no signs of tumour while two had metastases. Of the eight patients with chondrosarcoma, four were free of disease. All patients treated for metastatic carcinoma were dead by the time of the follow-up.
There was no significant correlation between response to the life quality questions and the type of prosthesis or length or type of resection. Of 13 patients with distal femoral tumours, 11 were able to wash and dry themselves without any trouble. Of eight patients with proximal tibial tumours, four gave a similar response. Four patients with femoral tumours and one patient with a tibial tumour were able to use public transportation and to walk down a flight of steps. A significantly better life quality score was found in patients with a distal femoral tumour compared with those with a proximal tibial tumour (Table 2).
As with the life-quality assessment, there was no correlation between functional score and type of prosthesis or type or length of resection. With regard to the entire group, seven patients could walk without limitation while eight could cope with a distance of 500–1,000 m without pain. In half the patients, the range of knee movement (ROM) exceeded 90°, and an additional third had a ROM between 60° and 90°. Sixteen patients were completely free of pain, and three complained of mild pain in the treated knee. The emotional acceptance was graded as enthusiastic in 13 patients and as good in five (Fig. 2).
The only factor having an impact on functional outcome was the site of the tumour. Of the patients treated for distal femoral tumours, seven had a pain-free walking distance of more than 1,000 m. No such individual could be found in the proximal tibial tumour group. An extension lag was seen in seven patients with distal femoral tumours and in six with proximal tibial tumours. Sixteen patients were completely free of pain irrespective of the site of the tumour; however, the emotional acceptance was 85% in the distal femoral tumour group compared with only 33% in the tibial group. Overall, functional outcome was significantly better in the distal femoral tumour group than in the tibial group (Table 3).
Reviewing our study material, it turned out that the most frequent complication was infection. Altogether, five cases (11%) of septic complications were found, one being superficial and four deep. There were two mechanical complications: a hinge, and a femoral stem fracture. Aseptic loosening of the prosthesis appeared in one patient, and in one case, a patellar tendon avulsion occurred.
Discussion
In the last decade, the therapy of malignant musculoskeletal tumours has changed. In 1985, amputation was performed in 90% of cases with musculoskeletal tumours treated at the orthopaedic clinic of Semmelweis University, leaving only 10% treated with limb-saving surgery. In recent years, this proportion has almost reversed: In 2000, limb-saving surgery became the dominating (82%) treatment, and the rate of amputation decreased. Since then, this change has further progressed, resulting in limb-saving surgery with endoprosthetic replacement in most patients.
Longer survival of patients with musculoskeletal tumours of the knee region has raised interest in comparing the outcome of the great variety of surgical methods, such as amputation, arthrodesis, allograft reconstruction, rotationplasty and tumour endoprosthetic implantation. Harris et al. [7] evaluated the results after amputation, arthrodesis and endoprosthetic replacement. They found that only patients with prosthetic reconstruction felt themselves close to the healthy population. However, considering other life quality aspects, there were no differences among the three groups. Boyle et al. [2] found no difference in the influence of the type of surgery on patients’ mental status—whether it was amputation or prosthetic reconstruction. Hillmann et al. [8] found better functional results after rotationplasty than after prosthetic implantation.
Previously, following analysis of the outcomes of different surgical procedures, the use of allografts seemed to be a good choice that provided adequate anatomical reconstruction. Further investigation, however, has shown an increased rate of post-operative infections, graft fracture, non-union, rejection or late arthritis of the knee, resulting in postoperative complications in nearly 40%. Therefore, this technique has disappeared from surgical practice [5].
When planning surgical interventions, it is necessary to take into consideration not only oncological aspects and the functional outcome, but also the needs of the patient including ethnic–cultural–religious differences. This was proven by Grimer et al. [6] in a study in which patients were given the choice between prosthetic reconstruction and rotationplasty, which gives excellent functional results. Only one chose rotationplasty while most considered it unacceptable. Similar experiences were observed by the same group with arthrodesis. Taking the risk of a more complex surgical procedure, the majority of the patients decided to have endoprosthetic replacement providing a flexible knee.
In an earlier publication, we reported our experiences with the Howmedica HMRS prosthesis [15]. In the study, we evaluated the outcome of all limb-saving procedures performed at our clinic for cases of knee-region malignant tumours, with respect to functional results and life quality. Sixteen patients succumbed to their malignant disease by the time of the follow-up, and a further four could not be traced. In view of their malignancy, it is probable that they had also died of their disease. We would like to emphasise that all five patients having surgery performed for carcinoma metastases had died by the time of the follow-up.
Evaluating life quality, we found that all patients rated the therapy excellent or good, regardless of the type of prosthesis, length or type of resection or tumour site. Surgical intervention did not limit their every-day life activities. However, trouble-free use of public transport or trouble-free walking on steps was observed three times more often in patients with a distal femoral tumour. It could be said, therefore, that the only factor having an influence on life quality was the site of the tumour. The results in cases of distal femoral tumours were significantly better than in those of proximal tibial tumours.
Regardless of the type of the implanted prosthesis, length and type of resection or tumour site, half of the patients had a ROM exceeding 90°, and a further 40% had a ROM between 60° and 90°. Two patients had smaller values (60° and 30°); both had had a septic complication. Also, apart from the factors examined by us, more than three fourths of the patients were completely free of pain. Of the factors taken into consideration, more than half of the patients in the distal femoral tumour group had a walking distance of more than 1,000 m while not a single patient in the group treated for tibial tumours could do this. The two groups also differed regarding knee-extension lag. Three quarters of the patients treated for a tibial tumour had an extension lag compared to only one third in the group with distal femoral tumours. The same proportion was observed regarding emotional acceptance: The surgical procedure was accepted completely only by one third of the patients in the tibial group against more than three fourths in the distal femoral group. So, as with life quality, we observed significantly worse functional results in the group with tibial tumours compared with the group with distal femoral tumours.
In the literature, it is widely accepted that the results in cases of proximal tibial tumours are inferior and complications more frequent than in cases of distal femoral tumours [1, 14, 17]. Poor soft tissue coverage, difficulties with anchoring the patellar tendon and possible injuries to the neurovascular system are the most likely causes for this [11]. Not only has the tumour site seemed to affect the final outcome. Studies with more patients also show that an increase in the length of resected bone or extra-capsular resections leaving a larger soft tissue defect, both influenced the outcome negatively [1, 10]. In our relatively small number of patients, the same effect could not be shown.
Factors including chemotherapy, the large soft-tissue defects and the relatively long duration of the surgical procedures, result in infections being the most frequent complications after endoprosthetic reconstruction [9]. The incidence of infections ranges between 2.9% and 13% [9, 13, 16]. The highest reported infection rate—33%—was published by Grimer et al. in cases with proximal tibial tumours [6]. This unacceptably high infection rate was caused by poor soft tissue coverage of the prosthesis in addition to the factors mentioned above. The incidence of septic complications significantly decreased, to about 12%, by using a rotation flap containing the medial head of the gastrocnemius, as described by Malawer and McHale [12]. The same procedure is used at our clinic, providing a septic complication rate of 11.6% and having 9.3% deep infections among them. Mechanical complications in the form of breakage of prosthetic components were observed in 4.6%. Aseptic loosening is reported in the literature to be rather frequent [13, 16] but was only seen in one patient in our study. However, since the average follow-up time was only 30 months, we will probably see more cases in the future. The most severe complication is thought to be local recurrence. In our study, we saw one local recurrence, for which an amputation was performed.
In our experience, prosthetic reconstruction of musculoskeletal tumours near the knee provides excellent functional results and life quality when performed in centres with adequate oncological background.
References
Anract P, Missenard G, Jeanrot C, Dubois V, Tomeno B (2001) Knee reconstruction with prosthesis and muscle flap after total arthrectomy. Clin Ortop 384:208–216
Boyle M, Tebbi CK, Mindell ER, Mettlin CJ (1982) Adolescent adjustment to amputation. Med Pediatr Oncol 10:301–312
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 88:63–69
Enneking WF (1987) Modification of the system for functional evaluation of surgical management of musculoskeletal tumors. In: Enneking WF (ed) Limb salvage in musculoskeletal oncology. Churchill Livingstone, New York, pp 626–639
Gebhardt MC, Flugstad DI, Spigfield DS, Mankin HJ (1991) The use of bone allograft for limb salvage in high grade extremity osteosarcoma. Clin Ortop 270:181–196
Grimer RJ, Carter SR, Tillman RM, Sneath RS, Walker PS et al (1999) Endoprosthetic replacement of the proximal tibia. J Bone Joint Surg Br 81:488–494
Harris IE, Leff AR, Gitelis S, Simon M (1990) Function after amputation, arthrodesis, or arthroplasty for tumors about the knee. J Bone Joint Surg Am 72:1477–1483
Hillmann A, Hoffmann C, Gosheger G, Krakau H, Winkelmann W (1999) Malignant tumor of the distal part of the femur or the proximal part of the tibia: endoprosthetic replacement or rotationplasty. J Bone Joint Surg Am 81:462–467
Holzer G, Windhager R, Kotz R (1997) One-stage revision surgery for infected megaprosthesis. J Bone Joint Surg Br 79:31–35
Horowitz SM, Lane JM, Otis JC, Healey JH (1991) Prosthetic arthroplasty of the knee after resection of a sarcoma in the proximal end of the tibia. J Bone Joint Surg Am 73:286–293
Ilyas I, Yuonge D, Pant R, Moreau P (2000) Limb salvage for proximal tibial tumours using a modular prosthesis. Int Orthop 24:208–211
Malawer MM, McHale KA (1989) Limb-sparing surgery for high-grade malignant tumors of the proximal tibia: surgical technique and a method of extensor mechanism reconstruction. Clin Ortop 239:231–248
Roberts P, Chan D, Grimer RJ, Sneath RS, Scales JT (1991) Prosthetic replacement of the distal femur for primary bone tumours. J Bone Joint Surg Br 73:762–769
Sanjay BKS, Moreau PG (1999) Limb salvage surgery in bone tumour with modular endoprosthesis. Int Orthop 23:41–46
Szendrői M, Antal I, Kiss J (2003) Howmedica tumor endoportézissel (HMRS) szerzett tapasztalatok. Magy Traumatol Ortop 2:122–129
Wirganovicz PZ, Eckhardt JE, Dorey FJ, Eilber FR, Kabo JM (1999) Etiology and results of tumor endoprosthesis revision surgery in 64 patients. Clin Ortop 358:64–74
Zwart HJJ, Taminiau AHM, Schimmel JW, Horn JR (1994) Kotz modular femur and tibia replacement: 28 tumor cases followed for 3 (1–8) years. Acta Orthop Scand 65:315–318
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skaliczki, G., Antal, I., Kiss, J. et al. Functional outcome and life quality after endoprosthetic reconstruction following malignant tumours around the knee. International Orthopaedics (SICOT) 29, 174–178 (2005). https://doi.org/10.1007/s00264-005-0655-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-005-0655-5