Abstract
Axial pain is one of the major complications after laminoplasty, and preservation of C7 spinous process during the procedure can reduce the axial pain. However, it has not been elucidated whether laminoplasty preserving the C7 spinous process can maintain neurological improvement for a long time. The purpose of our retrospective study was to investigate the long-term neurological outcome after open-door laminoplasty preserving the C7 spinous process for cervical spondylotic myelopathy (CSM). Clinical and radiological outcomes were analysed in 42 patients who underwent open-door laminoplasty preserving C7 spinous process and followed up for more than 5 years. Neurological function was evaluated by means of the Japanese Orthopaedic Association (JOA) scoring system for cervical myelopathy. Axial pain was assessed using a visual analog scale (VAS) at the last examination. Alignment and motion of the cervical spine were measured from radiographs, and magnetic resonance imaging (MRI) was used to evaluate postoperative compression at C7. The mean JOA score was 9.4 before surgery and 12.0 at the latest follow-up. The mean VAS score in 26 patients score was 9.7/100. No compression of the spinal cord was observed in any MRI at the latest follow-up. Preservation of the C7 spinous process does not influence the long-term outcome of CSM after laminoplasty. Although we did not have a comparative group, the procedure described here should be considered as the solution.
Résumé
Analyse rétrospective sur le devenir neurologique des patients traités par laminoplastie pour les myélopathies cervicales. Les douleurs rachidiennes axiales sont une des complications majeures après laminoplastie. La préservation del’épineuse de C7, durant l’intervention peut faire en sorte de diminuer ces douleurs axiales. Cependant, il n’est pas facile de savoir pourquoi la préservation de l’épineuse de C7 peut maintenir un résultat neurologique à long terme. Le propos de cette étude est d’analyser à long terme le devenir des laminoplasties préservant l’épineuse de C7 lors des CSM. Les paramètres cliniques et radiologiques ont été analysés chez 42 patients qui ont bénéficié d’une laminoplastie préservant l’épineuse de C7, ces patients ont été suivis pendant 5 ans. L’analyse neurologique a utilisé le score de l’Association Japonaise d’Orthopédie (JOA), les douleurs rachidiennes axiales ont été analysées par une échelle analogique de la douleur (VAS) lors du dernier examen. L’alignement et la mobilité de la colonne cervicale ont été mesurés sur les radiographies et l’IRM a évalué les compressions post-opératoires au niveau de C7. Le score moyen JOA était de 9,4 avant la chirurgie et de 12 au dernier suivi. Le score moyen de la douleur (VAS), sur 27 patients, a été de 9,7 sur 100. Aucune compression de le moelle n’a été observée sur l’IRM lors du dernier suivi. La préservation de l’épineuse de C7 n’entraîne donc pas d’influence sur le devenir à long terme de la CSM après laminoplastie.Cependant, nous n’avons pas de groupes comparatifs dans le cadre d’une procédure prospective pour considérer si cette solution est parfaitement satisfaisante.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laminoplastic procedures have been widely employed in the treatment of multilevel cervical spondylotic myelopathy (CSM), and the neurological recovery has been reported to be comparable with that after anterior decompression and spinal fusion [1, 2]. Axial pain, C5 palsy and limitation of the range of motion of the cervical spine are major complications after laminoplasty for cervical multisegmental compression myelopathy [3, 4].
Damage to the posterior musculature or the facet joints of the cervical spine and prolonged immobilisation are possible candidates, among others, for the cause of the axial pain; however, it has not yet been elucidated [5]. The spinous process of the C7 vertebra is the origin of the trapezius, rhomboid minor muscles and the nuchal ligament. Thus sacrificing this spinous process can cause great damage to the posterior musculature of the cervical spine. If the muscle damage is the cause of the pain, preservation of the attached muscles and ligament of the C7 spinous process in the course of the laminoplasty might lessen the axial pain.
Most of the authors who have reported the neurological outcome of cervical laminoplasty extended their procedures from C3 to C7. To our knowledge, the long-term outcome after laminoplasty from C3 to C6 has not been reported. We have not always included the C7 lamina in the laminoplasty in the case of CSM.
Therefore, the purpose of this study was to review the outcome in patients who underwent laminoplasty from C3 to C6 in the treatment of CSM to discover whether the exclusion of C7 from the operated area influences the neurological result.
Materials and methods
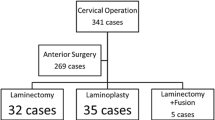
Between 1989 and 1998, 77 patients underwent laminoplasty for the treatment of CSM. Of these, 54 had laminoplasty from C3 to C6 using the same surgical procedure. In this study, we included 42 patients who were followed up for 5 years or more after surgery; the remaining 12 patients were lost to follow-up. There were 36 men and 6 women with a mean age at the time of surgery of 62.7 years (range 44–80 years), and a mean duration of follow-up of 9.6 years (range 6–15 years).
Procedure
A posterior approach was made along the nuchal ligament down to the line of the spinous process. The semispinalis cervicis muscle was not detached from the C2 spinous process. The trapezius and rhomboid minor muscles and the nuchal ligament were not detached from C7. The C3–C6 laminae were exposed to the medial aspect of the facet joints bilaterally. From C3 to C6 the spinous processes were cut at the bottom and were split in the midline using a high-speed drill. Dome-like laminotomy was carried out at the caudal portion of the C2 lamina and the cranial portion of C7. Bilateral gutters for hinges were made at the medial margin of the facet joints using a high-speed drill. Spinal canal enlargement was achieved by opening the split laminae bilaterally with a spreader and placing a spacer made of hydroxylapatite between the split spinous processes with polyethylene sutures [6].
Clinical assessment
To assess the severity of myelopathy, we used a scoring system for cervical myelopathy proposed by the Japanese Orthopaedic Association (JOA) [7]. The system consists of seven categories: motor function of fingers, shoulder and elbow, and lower extremity; sensory function of upper extremity, trunk, and lower extremity; and bladder function. The total score for a healthy individual is 17. The recovery rate described by Hirabayashi et al. was used: Recovery rate (%) = (postoperative JOA score − preoperative JOA score) / (17 − preoperative JOA score) × 100. To assess axial pain after surgery, the extent of nuchal and shoulder pain was scored using a visual analog scale (VAS) for 26 patients at the latest examination.
Radiographic assessment
Sagittal alignment of the cervical spine on lateral radiographs in neutral position was assessed as the C2–C7 angle between the tangential lines at the posterior edge of the C2 and C7 cervical vertebral bodies. Range of motion (ROM) of each segment from C2/3 to C6/7 was also measured using lateral radiographs taken in flexed and extended positions. Magnetic resonance (MR) images were also taken at the latest examination to determine whether the subarachnoid space was preserved at the caudal end of the operated area.
Results
The mean preoperative JOA score was 9.4 (range 4–14). Immediately after surgery, the mean JOA score was 12.7 (range 7–16) and the mean recovery rate was 43.4%. At the latest follow-up, the mean JOA score was 12.0 (range 6–17) and the mean recovery rate was 33.8% (Fig. 1). Among the 42 patients, 4 showed a decrease in JOA score of more than 2 points for reasons unrelated to the cervical myelopathy: these included malignant melanoma, lumbar canal stenosis, cerebral infarction and geriatric problems. None of these patients had spinal cord compression on MR images taken after the decrease in JOA score. Exclusion of these 4 patients yielded a JOA score and recovery rate at last follow-up of 12.6 and 41.7%, respectively.
Among the 26 patients who were evaluated using the visual analog scale (VAS), 16 did not complain of any pain, and another 4 had pain of less than 20/100 on the VAS. The VAS scores of the other 6 patients were 20 or more (range 20–50) at the latest follow-up.
Cervical alignment and motion
All but three patients had lordotic curvature before surgery, and their mean C2–C7 angle was 9.9° of lordosis (5° of kyphosis to 23° of lordosis). Although the mean C2–C7 angle at follow-up was 26.6° of lordosis (−6.8° of kyphosis to 26.6° of lordosis), three patients developed kyphosis (Figs. 2 and 3). The mean range of motion from C2 to C7 decreased from 37.8° (range 16–56) before surgery to 11.4° (range 3–19.5) at the latest follow-up.
A 67-year-old woman who underwent laminoplasty from C3 to C6 with dome-shaped laminotomy at C7. Her preoperative JOA score of 14 points recovered to 16 points at 15 years after surgery, and the recovery rate was calculated as 66.7%. Plain lateral radiographs before surgery (a) and 15 years after surgery (b) showed a decrease inthe C2–C7 angle from 23° to –6.8°, and a decrease in the cervical ROM from 54° to 7°. T1-weighted MR images before surgery (c) and 15 years after surgery (d) showed sufficient posterior spinal shift and no spinal cord compression at C6/7 (e)
A 49-year-old woman who underwent laminoplasty from C3 to C6 with dome-shaped laminotomy at C7. Her preoperative JOA score of 13.5 points recovered to 16 points at 15 years later after surgery. She developed kyphotic deformity after surgery; the C2–C7 angle deteriorated from 2° before surgery (a) to –13° 3 months after surgery (b) and −30° 15 years after surgery (c). The ROM of the cervical spine also decreased from 48° before surgery (d) to 10.4° at 15 years after surgery (e). MR images showed that sufficient decompression at C6/7 was maintained at the latest follow-up
The recovery rate of the JOA score, the lordosis angle and the ROM did not correlate with the VAS score at the latest follow-up (Fig. 4).
Discussion
The results of this study showed that the neurological recovery obtained after laminoplasty from C3 to C6 for the treatment of CSM seemed to be maintained for more than 5 years after operation. This was further confirmed by the MR images taken at the latest follow-up, in which no compression of the spinal cord at the caudal level of the laminoplasty was observed [7].
Most previous authors ignored the levels to be operated, or operated from C3 to C7 regardless of the level of spinal cord compression in the case of multisegmental CSM [8]. The C6/7 segment is not a common level of the spinal cord compression in CSM. Fukui and his co-workers investigated the patients who had dynamic canal stenosis showing posterior slippage, and found that only 1 of 53 patients had the slippage at C6–C7 [9]. Nevertheless, we think that it is not necessary to open the C7 lamina, since the pincer phenomenon can be managed by laminoplasty of C6 and dome-shaped laminotomy of the C7 lamina. It is important to avoid including laminae unnecessarily in the procedure, and inclusion of the C7 lamina should be exceptional in the case of CSM.
Malalignment is a possible cause for the poor neurological prognosis or the axial pain [10, 11]. These results showed that lordotic posture was maintained in most cases. In some, however, kyphosis developed after operation. Since muscles including the long rotator muscles and multifidus muscles which attach to the posterior structures were detached at the time of operation, the surgical procedure used in this study cannot prevent the kyphotic deformity in all cases.
The ROM decreased with time. This decrease seems to be caused, at least in part, by spontaneous inter-laminar fusion. The duration of postoperative immobilisation in a collar among the patients in the present series varied from 3 weeks to 3 months. On the assumption that this prolonged postoperative immobilisation causes a reduction in ROM, we decreased the period of immobilisation. In fact, many of our more recent patients have not worn a collar at all, and the reduction in ROM has become much milder. Thus, the difference between the ROM at 5 years and 10 years follow-up probably does not indicate a gradual increase in the limitation of motion, but rather reflects the reduction in immobilisation.
Although we assessed the axial pain using a VAS, we do not have any group for comparison. It was clear that the axial pain is not related to the neurological condition or the ROM.
In conclusion, preservation of the C7 spinous process in order to maintain the attachment of the back musculature does not influence the long-term neurological outcome after laminoplasty for cervical spondylotic myelopathy. The effect of the preservation on the axial pain was not ascertained; however, we should consider it as a means to overcome this problem.
References
Wada E et al (2001) Subtotal corpectomy versus laminoplasty for multilevel cervical spondylotic myelopathy: a long-term follow-up study over 10 years. Spine 26:1443–1447, discussion 1448
Wang MY, Green BA (2004) Open-door cervical expansile laminoplasty. Neurosurgery 54:119–123, discussion 123–124
Hosono N, Yonenobu K, Ono K (1996) Neck and shoulder pain after laminoplasty. A noticeable complication. Spine 21:1969–1973
Kawaguchi Y, Matsui H, Ishihara H, Gejo R, Yoshino O (1999) Axial symptoms after en bloc cervical laminoplasty. J Spinal Disord 12:392–395
Yoshida M et al (2002) Does reconstruction of posterior ligamentous complex with extensor musculature decrease axial symptoms after cervical laminoplasty? Spine 27:1414–1418
Katoh S, Ikata T, Hirai N, Okada Y, Nakauchi K (1995) Influence of minor trauma to the neck on the neurological outcome in patients with ossification of the posterior longitudinal ligament (OPLL) of the cervical spine. Paraplegia 33:330–333
Okada Y, Ikata T, Katoh S, Yamada H (1994) Morphologic analysis of the cervical spinal cord, dural tube, and spinal canal by magnetic resonance imaging in normal adults and patients with cervical spondylotic myelopathy. Spine 19:2331–2335
Wang MY, Shah S, Green BA (2004) Clinical outcomes following cervical laminoplasty for 204 patients with cervical spondylotic myelopathy. Surg Neurol 62:487–492
Fukui K, Kataoka O, Sho T, Sumi M (1990) Pathomechanism, pathogenesis, and results of treatment in cervical spondylotic myelopathy caused by dynamic canal stenosis. Spine 15:1148–1152
Suda K et al (2003) Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine 28:1258–1262
Kawakami M, Tamaki T, Ando M, Yamada H, Yoshida M (2002) Relationships between sagittal alignment of the cervical spine and morphology of the spinal cord and clinical outcomes in patients with cervical spondylotic myelopathy treated with expansive laminoplasty. J Spinal Disord Tech 15:391–397
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Higashino, K., Katoh, S., Sairyo, K. et al. Preservation of C7 spinous process does not influence the long-term outcome after laminoplasty for cervical spondylotic myelopathy. International Orthopaedics (SICOT) 30, 362–365 (2006). https://doi.org/10.1007/s00264-005-0062-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-005-0062-y