Abstract
We reviewed 38 hip replacements in 33 female patients (mean age 55.3 years) with developmental hip dysplasia. One patient had died and the remaining 32 patients (36 hips) had a mean follow-up of 12.2 years (range 8–19 years). All hips were replaced using the Müller cemented implant, and in 32 hips bulk femoral head autograft was used. In 33 hips the socket was reconstructed at the level of the true acetabulum. Complications included one intra-operative femoral fracture and two early dislocations. Correction of leg length discrepancy was possible in 30 patients. The post-operative mean modified Merle d’Aubigne and Postel scores for pain, movement and walking were 5.9, 5, and 5.3 respectively. One cup was revised due to aseptic loosening at ten years. All grafts united, but minor graft resorption was noticed in 24 hips, moderate in 2 hips and major in 1 hip.
Résumé
Nous avons examiné 38 remplacements prothétiques de la hanche chez 33 femmes (âge moyen 55,3 ans) avec une dysplasie de la hanche. Une patiente était décédée et les 32 autres (36 hanches) avaient un suivi moyen de 12,2 ans ( 8 à 19). Toutes les hanches ont eu un implant type Müller cimenté et pour 32 une autogreffe massive de tête fémorale a été utilisé. Pour 33 hanches la cavité a été reconstruite au niveau du paléo-cotyle. Les complications comprenaient une fracture fémorale opératoire et deux luxations précoces. La correction de l’inégalité de longueur des membres inférieurs était obtenue chez 30 malades. Le score postopératoire modifié de Merle d’Aubigné et Postel pour la douleur, la mobilité et la marche étaient en moyenne de 5,9, 5 et 5,3 respectivement. Une cupule a été révisée pour un descellement aseptique à 10 ans. Toutes les greffes ont consolidé, mais une résorption mineure de la greffe a été remarquée dans 24 hanches, une résorption modéré dans deux hanches et majeure dans une.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Developmental hip dysplasia (DDH) is the most common cause of secondary osteoarthritis of the hip [2]. Patients with advanced disease often present severe technical challenges regarding the prosthetic reconstruction of their hips. The acetabulum is hypoplastic and usually deficient anteriorly and superiorly, making it difficult to obtain sufficient bony coverage of the cup [5]. The femur is hypoplastic with a narrow medullary canal and increased torsion, resulting in excessive anteversion and a posterior location of the greater trochanter [25]. The distorted anatomy, especially in high dislocations, affects most of the soft tissues around the hip. With the possible exception of the abductors, the muscles around the hip joint are shortened and the capsule is thickened. The sciatic nerve is shortened and the course of the femoral nerve and the profunda femoris artery is distorted, putting them at increased risk of injury during surgery [15].
Acetabular reconstruction traditionally involves the use of a cemented cup with a structural bone graft fixed with screws or bolts at the deficient superolateral aspect of the socket. Although early results of the technique were gratifying, some authors have reported high failure rates in the long term and recommend the use of structural grafts only as a last resort [23], whilst others have maintained that structural grafts provide satisfactory long-term results [11].
In the present study we report our experience using the cemented Müller implant and structural or morselized autografts for acetabular reconstruction in a series of patients with DDH.
Patients and methods
Between 1981 and 1996 the senior author (G.P.) performed 38 consecutive total hip replacements in 33 women with end-stage arthritis secondary to DDH. The patients’ mean age at the time of surgery was 55.3 years (range 39–69 years). Twenty-eight patients were classified as Charnley category A (unilateral hip disease) and 5 as Charnley category B (bilateral hip disease, no other functional disabilities).
The severity of dysplasia was classified according to Hartofilakidis et al. [10]. Seven hips were dysplastic, 19 hips were low dislocations and 12 hips were classified as high dislocations. No patient had a normal acetabular angle. Sharp's angle [22] was between 45° and 60° and in the 12 high dislocations it was greater than 60°.
All patients received antibiotic prophylaxis and unfractionated or low-molecular-weight heparin perioperatively to prevent DVT.
In all cases the Müller cemented system was used (Protec, Winterthur, Switzerland.) This included an all-polyethylene cup with a monoblock straight stem in seven hips and a monoblock CDH Müller stem in the remaining 31 hips. All stems were made of chrome cobalt and had 22-mm heads.
In 27 hips a transtrochanteric approach and in the remaining 11 hips a direct lateral approach was used.
The true acetabulum was identified using the cortical edge of the cotyloid notch as landmarks. Reaming commenced in a postero-medial direction with the smallest available reamer and continued up to the inner table of the pelvis. Progressively larger reamers were used to enlarge the acetabulum to the limits of its anteroposterior width and a trial implant was used to determine the coverage of the cup by host bone. If more than 80% of the cup was covered by host bone, morselized graft only was packed supero-laterally. If the estimated cup coverage was between 60% and 80%, structural grafting was performed. If cup coverage was less than 60%, the so-called cotyloplasty technique was employed to reduce the area of cup supported by the structural graft [10]. The medial wall of the acetabulum was penetrated using a power reamer, reamings were impacted to reinforce the floor of the acetabulum, and structural supero-lateral grafting was performed .
Structural bone grafting
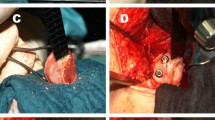
All soft tissues were removed from the deficient area of the acetabulum. Multiple 2-mm holes were drilled to obtain a bleeding bone bed. The patient's femoral head was shaped to conform to the contour of the prepared area and to provide complete cover of the acetabular cup. The graft was positioned carefully so that the primary compressive group of its trabeculae would be aligned with those of the ilium and it was fixed in the prepared acetabular area with two compression screws. The acetabulum and graft were reamed to a spherical shape, and reamings were used to fill any remaining gaps. Anchoring holes were then made in the host acetabulum. High-viscosity Palacos cement was pressurized and cup insertion followed (Fig. 1).
Preparation of the femur included widening of the canal with hand reamers. Initially, finger packing of high-viscosity Palacos cement and hand pressurization without a distal cement plug was used. In the last 23 hips of the study, treated after 1986, retrograde filling of the femoral canal with a cement gun and distal occlusion of the medullary canal was employed.
In cases where more than 4 cm leg lengthening was planned the femur was shortened in the metaphyseal region. This resulted in a neck cut at or slightly distal to the lesser trochanter. Reattachment of the greater trochanter followed with the leg in abduction using a three-wire technique.
Patients were mobilised three weeks after surgery and were advised to use two crutches for a total of 12 weeks. They were evaluated clinically and radiographically at three, six, and 12 months postoperatively and then every two to three years, unless otherwise indicated. The modified Merle d' Aubigne and Postel scale [18] was used for clinical evaluation.
Postoperative anteroposterior radiographs were assessed for cup coverage by graft. This was expressed as the ratio of the projection of the cup that was covered by graft to the projection of the distance between the most medial point and the lateral edge of the cup on the inter-teardrop line. The criterion for graft union was the disappearance of the graft–ilium interface or the appearance of bridging trabeculae across this interface. Graft resorption was graded as minor, moderate, or major according to Gerber and Harris [6]. Evaluation of fixation of the components was performed based on the criteria set by Harris et al. [9] for femoral stem loosening and Russotti et al. [21] for acetabular cup loosening. Ectopic bone formation was evaluated according to the criteria of Brooker et al. [3]. Annual linear wear of the polyethylene was measured according to the method described by Livermore et al. [16] Fig. 2.
Results
Clinical
The average preoperative leg length discrepancy was 5 cm (1–7 cm). Correction within 5 mm was possible in 30 patients. There was one intra-operative femoral fracture, which was treated successfully by cerclage wiring. There were no nerve palsies, vascular complications, or infections. Sixteen patients suffered a post-operative DVT. There were two dislocations 3 and 12 months after surgery. Both were successfully managed with closed reduction.
No patients were lost to follow-up. One patient whose bilateral hip were functioning replacements died ten years after the first arthroplasty and nine years after the second. The remaining 32 patients (36 hips) had a mean follow-up of 12.2 years (range 8–19 years). The pre-operative Merle d' Aubigne and Postel modified scores for pain, movement, and walking were 2.1 (range 1–3), 2.6 (range 1–4) and 2.7 (range 2–4) respectively. Post-operatively the scores increased to 5.9 (range 5–6), 5 (range 4–6) and 5 (range 5–6). One cup was revised for aseptic loosening 10 years postoperatively. No stem revision was required.
Radiographic
The mean abduction angle of the socket was 43° (range 35°–50°). The mean height of the hip center was 23 mm (range 10–40 mm), measured vertically from the inter-teardrop line. The mean cup coverage by the structural graft was 30% (range 20–40%). All structural grafts united. Minor graft resorption was seen in 26 hips, moderate resorption in five hips and marked resorption in 1 hip. These changes involved the lateral part of the graft, which was not supporting the cup. In six hips where morselized graft only was used there was rapid incorporation at 3–6 months postoperatively. In all cases where a cotyloplasty was performed, reconstitution and thickening of the medial acetabular wall was observed. All trochanteric osteotomies united, but wire breakage was observed in five hips. Brooker I–II ectopic bone formation was noticed in six hips. At the latest follow-up three cups were found to be radiographically loose without clinical symptoms. All stems were well fixed with no evidence of loosening. The mean rate of polyethylene wear was 0.08 mm/year (range 0.02–0.23 mm/year).
Discussion
Cup coverage can be accomplished by using small implants, by placing the cup medially beyond Koehler's line or higher in the ilium, by using a lateral bone graft. A small cemented [17] or cementless cup with screw augmentation [1] is the preferred reconstruction method when there is adequate acetabular bone stock. However, the severely dysplastic acetabulum is traditionally reconstructed with small cemented implants and structural bone grafts to enhance superolateral coverage. Harris et al. [8] popularized this technique and initially reported satisfactory early results [6]. The same group found that at an average follow-up of 16.6 years, 29% of the cups had been revised and a further 31% were radiologically loose [23]. The risk of cup failure was greater in younger patients and when the graft covered a large proportion of the cup.
Other authors, however, have reported superior results using structural grafting. Gross and Catre, reporting on 15 hips with DDH, found a 6% failure rate with the use of femoral autografts, at a follow-up of 99 months [7]. Kerboull et al. reported on 118 cemented THAs for high dislocation with a mean follow-up of 13 years [12]. In 81 hips structural grafts had been used. One stem and seven cups had been revised for aseptic loosening, and in total 15 hips (12.7%) had been revised for any reason. Iida et al. reported on 133 hips with DDH that were reconstructed with cemented THA and acetabular bone grafting, at a mean follow-up of 12.3 years [11]. Survivorship analysis predicted a 15-year acetabular survival rate of 96% and 75% with revision for aseptic loosening and radiological loosening as the endpoints respectively. Kobayashi et al. reported on 37 hips with DDH that were followed up for a mean of 19 years. There were no revisions and no loose cups [13]. These mixed results are attributed to a number of variables that make direct comparison difficult. These studies include variable follow-up periods, different patient populations, and different age groups. Patient age and activity level are important factors affecting mechanical failure. The severity of hip dysplasia and the percentage of cup coverage by the graft also vary in these series. Most authors agree that less than 30–40% of the cup should be covered by graft. In Harris's series the average coverage was 46%. Loose or revised cups had an average coverage of 49%, whereas the well-fixed cups had an average coverage of 36%. Finally, studies with long-term follow-up may include the initial learning curve of some authors with respect to structural bone grafting.
Cup coverage by host bone can be increased by medialization via a controlled fracture of the medial acetabular wall. Hartofilakidis et al. reported excellent results utilizing this technique with a cemented cup. At a mean follow-up of seven years only two of the 86 dysplastic hips were revised for aseptic loosening [10]. We have used this technique in five cases and it enabled us to limit the percentage of cup covered by graft.
Reconstructing the acetabulum at the anatomical level has several advantages. Besides being usually the site of the best available bone stock, this position restores normal hip biomechanics and abductor function and enables leg length equalization. Russoti and Harris and Anderson and Harris have maintained that a proximal but not lateral hip center of rotation is an acceptable alternative to structural graft use [1, 21], and McKenzie et al. could not detect any difference in the rate of loosening in relation to cup position [17]. However, Pagnano et al. suggested that superior positioning of the acetabular component, even without lateral displacement, leads to increased rates of loosening of the femoral and acetabular components [19]. A high hip center reconstruction does not restore normal hip biomechanics, necessitates the use of small cups with thin polyethylene, and predisposes to impingement. In addition, the existing bone stock is diminished and equalization of leg lengths is difficult.
When a high hip dislocation is reconstructed at the level of the true acetabulum, shortening of the femur is necessary to enable reduction of arthroplasty components and to reduce the risk of a sciatic nerve traction injury. We have used metaphyseal shortening via a lower neck cut at the level of or slightly distal to the lesser trochanter. We found it to be technically easy and have combined it with a trochanteric osteotomy and distal reattachment without any problems regarding bone union or sciatic nerve palsy. We consider the technique of subtrochanteric shortening [20] to be unsuitable for cemented stems.
Cemented stems have provided satisfactory results in dysplastic femora. McKenzie, reporting on 59 dysplastic hips with a mean follow-up of 16 years, found that 3.4% of the stems were revised and that 5% of the stems were radiographically loose [17]. Iidas et al., reporting on 133 hips at a mean follow-up of 12.3 years, found a 4% rate of femoral loosening and a 3% stem revision rate [11].
Cementless stems have been used in DDH in the hope that better results could be obtained in these young patients by biological fixation. Cementless stems can also be used in cases of narrow femoral canals, where the use of a cemented stem would lead to a cement mantle of inadequate thickness. Lai et al. reported on 56 Crowe type IV hips treated with a cementless total hip arthroplasty. At an average of 12.3 years (range 7–15.4 years) after operation there were no stem revisions [14]. Modular stems allow reorientation of femoral anteversion irrespective of the proximal metaphyseal morphology and have been used with satisfactory short-term results [4]. Another alternative is a conical tapered stem that allows orientation of anteversion by simple rotation. The Wagner cone prosthesis has been used with encouraging short-term results [24].
We attribute the good results of the present study to a number of factors. We strove to achieve less than 40% coverage of the cup by graft in all cases, medializing the cup and employing the cotyloplasty technique whenever necessary. Graft orientation with alignment of its trabeculae to those of the ilium may also have been a factor. Finally, the relatively high age of the patients in our study group and their less active lifestyle may have played a part. The high incidence of DVT that we observed is probably related to the long period of postoperative bed rest. We currently mobilise our patients 24 h after surgery and advise them to use two crutches for six weeks.
In conclusion, total hip arthroplasty for DDH is a demanding procedure. Most cases with significant proximal migration can be reconstructed at the level of the true acetabulum, yielding satisfactory results in terms of pain relief and function.
References
Anderson MJ, Harris WH (1999) Total hip arthroplasty with insertion of the acetabular component without cement in hips with total congenital dislocation or marked congenital dysplasia. J Bone Joint Surg Am 81:347–354
Aronson J (1986) Osteoarthritis of the young adult hip: etiology and treatment. Instr Course Lect 35:119–128
Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55:1629–1632
Cameron HU, Botsford DJ, Park YS (1996) Influence of the Crowe rating on the outcome of total hip arthroplasty in congenital hip dysplasia. J Arthroplasty 11:582–587
Crowe JF, Mani VJ, Ranawat CS (1979) Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am 61:15–23
Gerber SD, Harris WH (1986) Femoral head autografting to augment acetabular deficiency in patients requiring total hip replacement. A minimum five-year and an average seven-year follow-up study. J Bone Joint Surg Am 68:1241–1248
Gross AE, Catre MG (1994) The use of femoral head autograft shelf reconstruction and cemented acetabular components in the dysplastic hip. Clin Orthop Relat Res 298:60–66
Harris WH, Crothers O, Oh I (1977) Total hip replacement and femoral-head bone-grafting for severe acetabular deficiency in adults. J Bone Joint Surg Am 59:752–759
Harris WH, McGann WA (1986) Loosening of the femoral component after use of the medullary-plug cementing technique. Follow-up note with a minimum five-year follow-up. J Bone Joint Surg Am 68:1064–1066
Hartofilakidis G, Stamos K, Ioannidis TT (1988) Low friction arthroplasty for old untreated congenital dislocation of the hip. J Bone Joint Surg Br 70:182–186
Iida H, Matsusue Y, Kawanabe K, Okumura H, Yamamuro T, Nakamura T (2000) Cemented total hip arthroplasty with acetabular bone graft for developmental dysplasia. Long-term results and survivorship analysis. J Bone Joint Surg Br 82:176–184
Kerboull M, Hamadouche M, Kerboull L (2001) Total hip arthroplasty for Crowe type IV developmental hip dysplasia: a long-term follow-up study. J Arthroplasty 16 (8 Suppl 1):170–176
Kobayashi S, Saito N, Nawata M, Horiuchi H, Iorio R, Takaoka K (2003) Total hip arthroplasty with bulk femoral head autograft for acetabular reconstruction in developmental dysplasia of the hip. J Bone Joint Surg Am 85:615–621
Lai KA, Shen WJ, Huang LW, Chen MY (2005) Cementless total hip arthroplasty and limb-length equalization in patients with unilateral Crowe type-IV hip dislocation. J Bone Joint Surg Am 87:339–345
Lewallen DG (1998) Neurovascular injury associated with hip arthroplasty. Instr Course Lect 47:275–283
Livermore J, Ilstrup D, Morrey B (1990) Effect of femoral head size on wear of the polyethylene acetabular component. J Bone Joint Surg Am 72:518–528
MacKenzie JR, Kelley SS, Johnston RC (1996) Total hip replacement for coxarthrosis secondary to congenital dysplasia and dislocation of the hip. Long-term results. J Bone Joint Surg Am 78:55–61
Merle d' Aubigne R, Postel M (1954) Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am 36:451–475
Pagnano W, Hanssen AD, Lewallen DG, Shaughnessy WJ (1996) The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. J Bone Joint Surg Am 78:1004–1014
Reikeraas O, Lereim P, Gabor I, Gunderson R, Bjerkreim I (1996) Femoral shortening in total arthroplasty for completely dislocated hips: 3–7 year results in 25 cases. Acta Orthop Scand 67:33–36
Russotti GM, Harris WH (1991) Proximal placement of the acetabular component in total hip arthroplasty. A long-term follow-up study. J Bone Joint Surg Am 73:587–592
Sharp IK (1961) Acetabular dysplasia: the acetabular angle. J Bone Joint Surg Br 43:268–272
Shinar AA, Harris WH (1997) Bulk structural autogenous grafts and allografts for reconstruction of the acetabulum in total hip arthroplasty. Sixteen-year-average follow-up. J Bone Joint Surg Am 79:159–168
Strom H, Mallmin H, Milbrink J, Petren-Mallmin M, Nivbrant B, Kolstad K (2003) The cone hip stem: a prospective study of 13 patients followed for 5 years with RSA. Acta Orthop Scand 74:525–530
Sugano N, Noble PC, Kamaric E, Salama JK, Ochi T, Tullos HS (1998) The morphology of the femur in developmental dysplasia of the hip. J Bone Joint Surg Br 80:711–7119
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Papachristou, G., Hatzigrigoris, P., Panousis, K. et al. Total hip arthroplasty for developmental hip dysplasia. International Orthopaedics (SICO 30, 21–25 (2006). https://doi.org/10.1007/s00264-005-0027-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-005-0027-1