Abstract
A series of 179 closed femoral fractures treated by static interlocking nailing (Grosse-Kempf nail) was reviewed to evaluate the effect of dynamization on the time to bony union. In 75 patients, dynamization was performed whereas in 104 the implant was left static. Union occurred in 178 patients. We observed one infection. Time to union was significantly shorter in the static group (103 days) compared to the dynamized group (126 days).
Résumé
Une série de 179 fractures fémorales fermées traitées par enclouage verrouillé centro-médullaire statique (clou de Grosse-Kempf) a été examinée pour évaluer l’effet de la dynamisation sur le temps de consolidation osseuse. Chez 75 malades la dynamisation a été exécuté, alors que pour 104 l’implant était laissé statique. La consolidation s’est effectuée chez 178 malades. Nous avons observé une infection. Le temps de consolidation était significativement plus court dans le groupe statique (103 jours) comparé au groupe dynamisé (126 jours).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Using interlocking nailing for femoral shaft fractures has become popular over the past two decades, expanding the indications for closed intramedullary fixation [7]. Interlocking nails use supplementary fixation with screws, which may be inserted at the proximal, distal, or both ends of the nail. When the nail is stabilized with screws at both ends, the fixation is static. This kind of fixation avoids the problems of loss of stabilization, shortening, and rotation that may be observed with a simple intramedullary nail. The most common indication for interlocking nailing is a comminuted fracture [6]. In fact, by stabilizing the extremities of the nail, stresses on the fracture are minimized, and the fracture is protected during rehabilitation. The principles of this technique require the fixation to be converted from static to dynamic by removing the screw or screws farthest from the fracture site [3, 6, 7] some weeks after nailing. Weight bearing is allowed only after this procedure in comminuted fractures. The effect of dynamization is to promote callus remodeling and prevent the fixation device from breaking [10]. The literature in the 1980s strongly advocated dynamization 10–16 weeks after nailing [6, 9, 11]. The most recent experimental [4] and clinical [2] reports do not consider dynamization mandatory, and some even consider it harmful [12, 13]. In contrast, the recent studies by Basumallick and Bandopadhyay [1] suggest that while dynamization does not change the union rate when compared to static nailing, it definitely shortens the mean time to union in open interlocking nailing of femoral fractures. They further draw attention to the frequent occurrence of limb shortening after dynamization. The aim of this study was to compare cases that had undergone dynamization with those that had not and to find the real indications for this supplementary surgical stage in fractures of the femoral diaphysis.
Materials and methods
One hundred and seventy-nine patients with fractures of the femoral diaphysis were treated in Bologna (Rizzoli Orthopaedic Institute and Pizzardi Maggiore Hospital), Italy. Patients from Rizzoli were treated between 1982 and 2001 whereas those from Maggiore Hospital were treated between 1988 and 2001. Thirty-nine patients were female and 140 were male. Their ages ranged between 14 and 87 (mean 30) years. All cases were treated with the Grosse-Kempf static interlocking nail (Stryker-Howmedica). The causes of injury included 139 traffic accidents, six falls from heights, and 34 falls at ground level. Most patients had multiple associated injuries. Ipsilateral fractures were presented in 21 cases, upper arm fractures in 11, head trauma in 14, and 18 patients were considered polytraumatised.
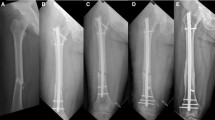
Patients were divided into two main groups according to postoperative treatment. The first group included patients who had undergone nail dynamization (dynamized group). Dynamization was performed by removing the screws farthest away from the fracture as soon as sparse callus formation was noted at the fracture site. Dynamization was carried out in 75 cases at a mean of 86.2 days after nailing (SD±37.3). The second group (static group) included 104 patients who had not undergone this procedure. The dynamized group included 12 female and 63 male patients with a mean age of 30 (15–76) years. There were 62 closed, five type I, and eight type II open fractures [5]. According to the AO classification, 21 fractures were 32A type (seven 32A1, six 32A2, eight 32A3), 33 were 32B type (14 32B1, seven 32B2, 12 32B3), and 21 were 32C type (nine 32C1, four 32C2, eight 32C3). The static group included 104 patients with a mean age of 30 (14–87) years. There were 27 female and 77 male patients. There were 90 closed fractures, 11 type I, and three type II open fractures. According to the AO classification [8], 47 fractures were 32A type (eleven 32A1, fourteen 32A2, twentytwo 32A3), 42 were 32B type (ten 32B1, twenty 32B2, twelve 32B3), and 15 were 32C type (six 32C1, three 32C2, six 32C3). In this group, we included six patients who had the distal screws removed 6 months after surgery, after the fracture had healed, due to persistent pain at the site of the screws. Fracture union was defined as follows. Clinically, there was no pain and no tenderness, and patients were walking without aids; radiographically, solid callus with cortical density had bridged the fracture fragments [12].
Statistical analysis was carried out using regression analysis and Pearson’s correlation coefficient to test for correlations between the two groups. Where data was not homogeneous, the Mann–Whitney and Kruskal–Wallis tests were used and evaluated by the Monte Carlo method for small samples. Significance was set at p<0.05. All data were analyzed using commercially available software SPSS 7.5.
Results
All cases but one healed. The only case of nonunion required the removal of the nail and internal fixation by a plate with grafting. This resulted in a limb shortening of 2 cm. This patient had undergone proximal dynamization of the nail before there was any evidence of periosteal callus continuity. In this case, the nail had also broken. There was one septic complication, which completely resolved after removal of the nail 13 months after the initial procedure.
A diagram describing the incidence of dynamization in our series is shown in Fig. 1. On the whole, time to union was significantly shorter in the static group (p=0.005), which was 103 days (SD±23.4), compared to 126 days in the dynamized group (SD±42.8) (Fig. 2). This trend remained even when there were factors that interfered with the healing process (fracture of the ipsilateral limb, pelvis, head injury, and suboptimal reduction of the fracture). Of the 108 patients in this series (Fig. 3), the 74 of the static group had a mean time to union of 95 days (SD±14.2) compared with 104 days in the dynamized group (SD±21.4).
Table 1 shows mean time to union and standard deviation of the whole series divided according to the AO classification. For group 32A, healing was significantly faster in subgroup 32A3 (p=0.005). With regard to the so-called complex fractures (group 32B), although healing was faster in all three subgroups, it was statistically significant only for subgroups 32B2 (p=0.005) and 32B3 (p=0.004). In group 32C, we found no statistically significant difference either for the main group or for the separate subgroups. Union times were, however, shorter in the static group for type 32C3 fractures.
We observed seven cases of limb shortening in the dynamized group and six cases in the static group. In the first group, limb-length discrepancy was less than 1 cm in four cases and more than 2 cm in the remaining three cases. The six patients of the static group had a shortening always less than 6 cm. In three of the dynamized group, the nail broke. Two of these nails were of the first generation type; in both cases, the nail broke after fracture union at the upper end of the slot. In two of the static group cases, the distal screws of the nail broke; in both cases, the nail was locked distally with only one screw.
Discussion
The need to dynamize a static intramedullary fixation of a femoral fracture is a moot point. Some authors advocate converting the static fixation into a dynamic one from 10 [3, 7] to 16 weeks [6] after nailing whereas others [2, 4] consider this procedure unnecessary or even harmful [12, 13]. In some cases, shortening was observed when the system had been dynamized before appropriate callus formation [2, 13]. Wu and Chen [13] reported that in only half of their cases of segmental femoral fractures was dynamization successful and suggested that in the presence of delayed union early, cancellous grafting should be considered. At the end of the 1980s, Dagrenat et al. [4] carried out an in vivo experimental study to assess the effect of dynamization on interlocking nailing. They reproduced comminuted fractures in the tibias of 20 Swiss alpine sheep weighing 40–60 kg and divided them into two groups: ten sheep underwent static fixation and ten underwent dynamic fixation. All the sheep were suspended in hammocks for 5 weeks. After 35 days, the sheep were brought back down to the ground. The authors concluded that there were no statistically significant differences between cases dynamized and those with static fixation and that dynamization is only necessary in cases of a persistent gap between the fragments.
Brumback [2] studied 87 diaphyseal fractures of the femur treated by interlocking nailing. They obtained union in 98% of cases without converting the static fixation to a dynamic one. Two patients needed conversion from static to dynamic interlocking fixation because of inadequate fracture healing, and both progressed to uneventful union. The authors concluded that conversion from static to dynamic interlocking fixation is rarely necessary in femoral fractures. Static interlocking nails apparently do not restrict micromotion enough to inhibit healing, and full weight bearing can often be started early. No deformation or failure of the static interlocking nails occurred when these patients began to walk. In the past, other studies documented failure of the static interlocking nails using first-generation Grosse-Kempf nails. These nails were weakened by a combination of the welding at the proximal end (between the cylindrical and the triflanged portion of the nail), the hole for the transverse screw, and the end of the slot [2].
Our study over a period of about 20 years shows that in most femoral fractures, time to union was shorter in the nondynamized (static group) compared with the dynamized group. This characteristic is statistically significant in the series as a whole and even in those cases where there were factors that interfere with the healing process. By detailed analysis of the type of fracture according to the AO classification, we found that group 32A and 32B fractures healed faster if fixation was not dynamized. In these cases, early weight-bearing, even on a static fixation device, probably promoted faster formation of the callus as noted by other authors [2].
Healing times were significantly faster, especially in group 32A, subgroup 32A3 (p=0.005). With regard to complex fractures (group 32B), although healing was constantly faster in all three subgroups, only 32B2 (p=0.005) and 32B3 (p=0.004) were statistically significant. In group 32C, healing times were not significantly faster either in the main group or in separate subgroups. Time to union was only longer in nondynamized nails for type 32C3 fractures.
One problem that may be encountered with static fixation is the irritation of soft tissues around the screw heads. Although we encouraged patients to wait for at least a year for the fracture to heal in order to remove the fixation device and locking screws in a single stage, we were obliged to remove the distal screws in six cases before removing the nail.
References
Basumallick MN, Bandopadhyay A (2002) Effect of dynamization in open interlocking nailing of femoral fractures. A prospective randomized comparative study of 50 cases with a 2-year follow-up. Acta Orthop Belg 68:42–48
Brumback RJ (1988) Intramedullary nailing of femoral shaft fractures. Part II: Fracture-healing with static interlocking fixation. J Bone Joint Surg Am 70:1453–1462
Brumback RJ (1996) The rationales of interlocking nailing of the femur, tibia and humerus. An overview. Clin Ortop 324:292–320
Dagrenat D, Moncade N, Cordey J, Rahn BA, Kempf I, Perren SM (1988) Effects of the dynamization of static bolt nailing. In vivo experimentation. Rev Chir Orthop Repar Appar Mot (Suppl) 2:100–104
Gustillo RB, Anderson JT (1976) Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones. J Bone Joint Surg Am 58:453–458
Kempf I, Grosse A, Beck G (1985) Closed locked intramedullary nailing. Its application to comminuted fractures of the femur. J Bone Joint Surg Am 47:709–720
Kempf I, Grosse A, Laffourge D (1978) L’apport du verrouillage dans l’enclouage centromédullaire des os longs. Rev Chir Orthop Repar Appar Mot 64:635–651
Muller M, Nazarian S, Koch P (1978) Classification AO des Fracturens. Springer Verlag, Berlin Heidelberg New York
Tigani D, Giunti A, Boriani S (1986) Ostesintesi con chiodo di endomidollare avvitato: difficoltà, limiti, prospettive. Chir Organi Mov 71:227–233
Tigani D, Moscato M, Sabetta E, Padovani G, Boriani S (1989) Breakage of the Grosse-Kempf nail: causes and remedies. Ital J Orthop Traumatol 15:185–190
Winquist RA, Hansen ST (1980) Comminuted fractures of the femoral shaft treated by intramedullary nailing. Orthop Clin North Am 11:633–640
Wu CC (1997) The effect of dynamization on slowing the healing of femur shaft fractures after interlocking nailing. J Trauma 43:263–267
Wu CC, Chen W (1997) Healing of 56 segmental femoral shaft fractures after locked nailing. Acta Orthop Scand 68:541–544
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tigani, D., Fravisini, M., Stagni, C. et al. Interlocking nail for femoral shaft fractures: is dynamization always necessary?. International Orthopaedics (SICOT) 29, 101–104 (2005). https://doi.org/10.1007/s00264-004-0627-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-004-0627-1