Abstract
We retrospectively reviewed 31 neurologically intact patients with burst L1 fractures. We obtained a follow-up clinical evaluation after a mean of 43 (14–80) months from 26 patients—11 treated surgically and 15 managed non-surgically. Patients were assessed with regard to pain, employment status, recreational activities and overall satisfaction. At final follow-up of 15 patients managed non-surgically, six had little or no pain; 12 had returned to work with six declaring little or no restrictions, and eight had returned to the same level of recreational activity as prior to injury with seven declaring little or no restrictions. Of 11 patients treated surgically, four had little or no pain; seven had returned to work with three declaring little or no restrictions, three had returned to the same level of recreational activity as prior to injury and four declared little or no restrictions. There was no correlation found between vertebral collapse, kyphosis, retropulsion and clinical outcome. Patients who had non-operative management reported a good functional outcome. However, patients who required surgical stabilisation due to different fracture characteristics reported a poorer functional outcome.
Résumé
Nous avons examiné rétrospectivement 31 malades avec une burst fracture de L1, sans trouble neurologique. Nous avons obtenu une évaluation clinique après un suivi moyen de 43 mois (14–80) pour 26 malades, 11 traités chirurgicalement et 15 non-chirurgicalement. Les malades ont été répartis selon la douleur, le statut de l’emploi, les activités de loisirs et la satisfaction globale. Au dernier examen des 15 malades traités non-chirurgicalement, six avaient peu ou aucune douleur; 12 avaient repris leur travail avec six déclarant peu ou aucune restriction et huit étaient revenus, pour les activités de loisirs, au même niveau qu’avant la fracture avec sept déclarant peu ou aucune restriction. Parmi les 11 malades traités chirurgicalement, quatre avaient peu ou aucune douleur; sept avaient repris le travail avec trois déclarant peu ou aucune restriction, trois étaient revenus au même niveau d’activité de loisirs et quatre déclaraient peu ou aucune restriction. Aucune corrélation n’a été trouvé entre le collapsus vertébral, la cyphose, la rétropulsion et le résultat clinique. Les malades qui avaient été traité non-chirurgicalement ont rapporté un bon résultat fonctionnel. Les malades qui ont nécessité une stabilisation chirurgicale à cause des caractéristiques de la fracture ont rapporté un résultat fonctionnel moins bon.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Burst fractures involve compression failure of the anterior and middle columns [2]. These fractures commonly occur in the thoracolumbar spine due to the relative immobility of the thoracic spine compared to the lumbar spine. The upper thoracic spine (T1–T10) is stabilised by the ribs and facet orientation and is less susceptible to trauma. However, at the T12–L1 junction, there is a fulcrum of increased motion, and this area is more commonly affected.
The management of thoracolumbar burst fractures is controversial, with advocates of operative and non-operative approaches [7, 8]. One of the complications of burst thoracolumbar fractures is the residual and potentially progressive kyphotic deformity arising post-reduction. Post-mobilisation and 3-month follow-up radiographs of the patients included in this report objectively assessed this problem. Other complications considered included residual pain, impaired working capacity and recreational restrictions.
Materials and methods
Medical records, radiographs and CT scans of 31 patients with burst fractures of L1 from 1996 through 2001 were reviewed. The criteria for selection were neurologically intact patients under 65 years of age. Pathological fractures were excluded. We obtained clinical follow-up evaluation at 1 year or more on 26 patients; five patients were lost to follow-up.
At the National Spinal Injuries Unit of Ireland, there are agreed selection criteria for the surgical management of burst lumbar fractures. Injuries displaying one of the three following features are treated surgically: greater than 50% anterior body compression, greater than 15° kyphosis or greater than 50% spinal canal compromise. Patients not meeting these criteria are managed conservatively.
The non-surgical group [1] is treated initially with bed rest and log rolled every 2 h. No attempt is made to reduce their fracture. A specially fitted anterior hyper-extension cast is applied with maximal lordosis at the thoracolumbar spine. Early ambulation is encouraged, as tolerated by pain, with physiotherapy supervision. Patients wear their thoracolumbar cast for 3 months are advised to continue with an additional 6–12 weeks of bracing with a hyper-extension orthosis. They are also advised against heavy work and sports for 3 months but are allowed activities of daily living and sedentary work.
The surgical group has posterior stabilisation and fusion of the thoracolumbar junction. This procedure consists of a posterior mid-line incision centred over the fractured vertebra; exposure out to the tips of the transverse processes; placement of pedicle screws in the level above (T12), in the fractured vertebra (L1) and in the level below the fractured vertebra (L2); and instrumentation with variable screw placement or rods bent into a lordotic configuration. Postural and instrumental reduction is performed. Post-operative management is the same as the non-surgical group.
Medical records were reviewed for patient’s age, gender, mechanism of injury, level of injury, presence of associated injuries, method of treatment and duration of hospitalisation. Radiographs were reviewed from the time of injury, time of surgical fusion or cast application, time of mobilisation and at 3-month follow-up evaluation. Computed tomography of the spine was used to assess the initial degree of spinal canal compromise.
The lateral radiograph was used to measure the amount of anterior body compression and degree of vertebral kyphosis. The percentage of anterior body compression was measured with respect to the next adjacent intact vertebrae above and below the fractured vertebra. Sagittal plane kyphosis was measured from the inferior end plate of the vertebral body above the fracture to the inferior end plate of the fractured body [6]. The degree of retropulsion was measured on CT scans at the mid-sagittal line, in 10% increments, on the cut that showed the maximum retropulsion. Comparisons were made using the follow-up cut most similar in level to the initial maximum cut.
Clinical follow-up evaluation was performed using a questionnaire in which patients were asked to rate their pain on a scale from one to five modified from the pain scale of Denis [3], with five being no pain at all, four being mild pain rarely needing non-narcotic medications, three being moderate pain occasionally needing non-narcotic medications, two being significant pain occasionally needing narcotic medications and one being severe pain needing narcotic medication regularly. Patients were asked to rate their ability to work on a scale of one to five, with five being no restrictions, four being mild restrictions, three being moderate restrictions, two being significant restrictions and one being severe restrictions. Patients pre-injury and post-injury employment status was noted. Patients who had become unemployed since their injury were asked if this was as a result of restrictions associated with their injury. Patients who were still employed were asked if their current job was more, equally or less physically demanding than prior to their injury. Patients were asked to rate their ability to participate in recreational activities on a scale of one to five, with five being no restrictions, four being mild restrictions, three being moderate restrictions, two being significant restrictions and one being severe restrictions. Patient’s pre-injury and post-injury recreational activities were noted. Patients were asked to rate their overall satisfaction with their outcome. This they graded as very satisfied, slightly satisfied, slightly dissatisfied or very dissatisfied.
Results
Thirty-one patients meeting the selection criteria were treated for burst fractures of L1 between September 1996 and December 2001 at the National Spinal Injuries Unit. Five patients could not be followed-up; of these, three were foreign nationals who had returned home, one was deceased and one was homeless and living in sheltered accommodation. Of the five patients lost to follow-up, three had been treated operatively and two managed conservatively.
Of the overall 31 patients, there were 21 men and ten women; ages ranged from 18 to 62 (mean 36) years. The mechanism of injury involved falls from height in 17 patients, road traffic accidents in seven, minor falls on stair cases in three, a slip on ice in one, a fall from farm machinery in one, being struck by a heavy object in one and an unwitnessed alcohol-induced seizure in one. Associated injuries included fractures of the calcaneus (one), talus (one), medial and lateral malleoli (two), radius and ulna (two), ribs (one), sternum (one), pelvis (one—stable fracture), facial bones (one), skull (one), spinous and transverse processes of cervical vertebrae (one) and spinous and transverse processes of adjacent thoracolumbar vertebrae (two).
The duration of hospitalisation ranged from 2 to 22 days, with a mean hospitalisation time of 8 days for the non-surgically treated group compared with a mean of 13 days for the surgically treated group. The follow-up clinical evaluation was carried out on 26 patients: 15 were patients managed non-operatively and 11 were treated operatively. Follow-up time ranged from 14 to 80 months, with a mean of 43 months. The follow-up clinical evaluation took into account pain, ability to work, ability to partake in recreational activities (Table 1) and overall satisfaction with outcome.
Radiographic outcome
At the time of injury, the mean anterior body compression was 31% (range 3–63%) The initial retropulsion as determined on CT scan averaged 29% of the mid-sagittal canal diameter. The mean retropulsion for the non-surgical group was 16% as compared with 40% in the surgical group. The mean kyphotic deformity in the non-surgical group was 9.5° at the time of injury, 8.4° post-mobilisation and 14.4° at 3-month follow-up. In contrast to this, the mean kyphotic deformity in the surgical group was 15.6° at the time of injury, 2.1° post-mobilisation and 9.6° at 3-month follow-up.
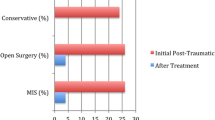
Pain
Of the 15 patients followed up in the non-surgical group, one rated his pain as “severe”, five rated their pain as “significant”, three as “moderate”, four as “mild” and two reported “no pain”. However, in the 11-patient surgical group, three rated their pain as “severe”, one as “significant”, three as “moderate” and four as “mild” (Table 1).
Return to work
Of the patients in the non-surgical group, 12 had returned to work and three had become unemployed due to their injury. Eleven of the patients returning to work had done so at a job with the same physical demands as prior to their injury. One had been a student at the time of injury and is now a barman. Of the three patients who had become unemployed subsequent to their injury, their previous employments were as roofer, building labourer and truck driver. All reported pain and restrictions due to their injury as the primary cause of their unemployment. With regard to work restrictions, three patients reported “severe” restrictions, four “significant” restrictions, two “moderate” restrictions, five “mild” restrictions and one “no restrictions”.
In the surgical group, seven had returned to work and four had become unemployed due to their injury. Five of the patients returning to work had done so at a job with the same physical demands as prior to their injury. Two patients had returned to work in positions less physically demanding: one had been a building labourer and had become a trainee supervisor whilst the other had been a warehouse worker and had become a computer operator. The previous employments of the four patients who had become unemployed were truck driver, steel erector, hotel manager and student. All reported the effects of their injury to be the primary cause of their unemployment. Regarding work restrictions, four patients reported “severe” restrictions, one “significant” restriction, three “moderate” restrictions and three “mild” restrictions (Table 1).
Recreational abilities
In the non-surgical group, eight had returned to the same level of recreational activity as prior to their injury, and seven had returned to a diminished level of participation. When asked to grade their restriction in recreational activity, three reported “severe” restrictions, four “significant” restrictions, one “moderate” restrictions, five “mild” restrictions and two “no restrictions”. In the surgical group, three had returned to the same level of recreational activity as prior to their injury, and eight had returned to a diminished level of recreational activity. When grading their recreational restrictions, five reported “severe” restrictions, two “moderate” restrictions, three “mild” restrictions and one “no restrictions” (Table 1).
Satisfaction level
In the non-surgical group, nine reported being “very satisfied”, four “slightly satisfied” and two “very dissatisfied”. Both of the “very dissatisfied” patients had become unemployed. One was a 23-year-old roofer. The other was a 62-year-old builder who required posterior stabilisation 17 months post-injury due to persistent severe pain. In the surgical group, nine reported being “very satisfied”, one “slightly satisfied” and one “very dissatisfied”. The one “very dissatisfied” patient had been a very active 20-year-old man who described having “significant” work restrictions, “severe” recreational restrictions and required counselling post-injury. No correlation was found between kyphotic deformity, extent of canal compromise and clinical outcome.
Discussion
This study looks at the functional outcome of patients following burst fractures of L1. These patients range from those with minimal compression to those with extensive traumatic destruction. Various criteria have been suggested for operative and non-operative treatment, including the percentage of anterior body compression, the degree of kyphotic deformity, the amount of canal compromise and neurological impairment.
Our study has shown that patients for whom conservative management is indicated, using the above criteria, generally have a highly satisfactory clinical outcome [5, 7]. Hyper-extension casting with early mobilisation was shown to reduce hospitalisation time, avoid the costs and risks of surgery and return patients to the functional activities of daily living quicker than surgical treatment. The patients in our non-operative group reported better pain assessment results on clinical follow-up, with more patients reporting “mild” or “no pain” and less patients reporting “severe pain”. The non-surgical group was also shown to have a higher rate of return to employment. Of those returning to work, there was a higher proportion of patients returning to a job with the same physical demands as prior to their injury. Additionally, a higher proportion of patients reported “mild” or “no restrictions” in their ability to work and in their ability to partake in recreational activities.
Surgical treatment with short segment pedicle screw fixation was shown to have superior results with respect to initial correction of kyphotic deformity, as displayed in the post-mobilisation radiographs [4]. However, much of this correction was soon lost, and the kyphosis increased while the hardware remained intact. We found that the increase in kyphosis over the subsequent 3 months in the surgical group was comparable to that displayed in the conservatively managed group.
This study does not intend to compare the results of operative and non-operative management of burst lumbar fractures because both groups of patients have different fracture characteristics. It does, however, aim to highlight the discrepancy in functional outcome achieved by both groups. This data allows the prognosis of burst lumbar fractures, managed either surgically or conservatively, to be assessed with greater accuracy and provides patients with a more accurate indication of their expected outcome.
However, the enhanced functional outcome of conservatively managed patients may pose the question as to whether the indications for surgical treatment should be narrower [7, 8]. It may be suggested that the surgical fusion of two mobile spinal segments contributes to the poorer clinical outcome.
Occasionally patients barely meet the radiographic criteria for surgical management. Should those in the “grey zone” be treated preferentially by closed treatment and thus avoid instrumenting T12–L2 key motion segments?
References
Chow GH, Nelson BJ, Gebhard JS, Brugman JL, Brown CW, Donaldson DH (1996) Functional outcome of thoracolumbar burst fractures managed with hyperextension casting or bracing and early mobilisation. Spine 21:2170–2175
Denis F (1983) The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine 8:817–831
Denis F, Armstrong GWD, Searls K, Matta L (1984) Acute thoracolumbar burst fractures in the absence of neurological deficit: a comparison between operative and nonoperative treatment. Clin Orthop 189:142–149
Leferink VJ, Keizer HJ, Oosterhuis JK, van der Sluis CK, ten Duis HJ (2003) Functional outcome in patients with thoracolumbar burst fractures treated by dorsal instrumentation and transpedicular cancellous bone grafting. Eur Spine J 12:261–267
Shen W, Shen Y (1999) Nonsurgical treatment of three-column thoracolumbar junction burst fractures without neurological deficit. Spine 24:412–415
Shen W, Liu T, Shen Y (2001) Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine 26:1038–1045
Tropiano P, Huang RC, Louis CA, Poitout DG, Louis RP (2003) Functional and radiographic outcome of thoracolumbar and lumbar burst fractures managed by closed orthopaedic reduction and casting. Spine 28:2459–2465
Wood K, Butterman G, Mehbod A, Garvey T, Jhanjee R, Sechriest V (2003) Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomised study. J Bone Joint Surg Am 85:773–781
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Butler, J.S., Walsh, A. & O’Byrne, J. Functional outcome of burst fractures of the first lumbar vertebra managed surgically and conservatively. International Orthopaedics (SICOT) 29, 51–54 (2005). https://doi.org/10.1007/s00264-004-0602-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-004-0602-x