Abstract
We analysed 133 patients treated with resection and endoprosthetic proximal tibial replacement from 1988 to 2000. Mean age was 22.3 years and osteosarcoma was the most common tumour. Average follow-up was 59.4 months. An excellent functional result was achieved in 63 patients and a good result in 36. The number of patients who had no evidence of disease was 102. Twenty-four patients died due to disease. Infection was the most common complication, followed by periprosthetic fracture and aseptic loosening. The 5-year limb survival rate was 85.5%.
Résumé
Nous avons analysé 133 malades, traités par résection et remplacement endoprothétique du tibia proximal de 1988 à 2000. L'âge moyen était 22.3 ans et l'ostéosarcome était la tumeur la plus fréquente. Le délai moyen de suivi était 59.4 mois. Un excellent résultat fonctionnel a été obtenu pour 63 malades et un bon résultat pour 36. Le nombre de malades qui n'avaient pas de signe de maladie était 102. Vingt-quatre malades sont morts à cause de la maladie. L'infection était la complication la plus fréquente, suivi par les fractures périprothétiques et le descellement aseptique. La présence du membre à 5 ans était de 85.5%.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Limb salvage surgery has been established as an alternative to amputation in patients with both low-grade and high-grade malignant tumours and also aggressive benign tumours due to technical advances in diagnostic imaging, chemotherapy and radiotherapy, and improved surgical methods [25]. With the advent of effective adjuvant chemotherapy, cure rates in excess of 60% can be expected for osteosarcoma and Ewing's sarcoma [3, 21]. This improvement in patient survival has presented to the orthopaedic surgeon the challenge of maintaining the function and integrity of the involved limb for longer periods.
Management of proximal tibial tumours present the most challenging problems in limb salvage surgery due to various factors like lack of local musculature and the paucity of soft tissue available for covering the defects after tumour removal [25]. We have chosen to undertake endoprosthetic replacement, as it has been demonstrated to provide a good functional outcome in most cases.
Materials and methods
One hundred and thirty-three patients who underwent resection and endoprosthetic proximal tibial replacement between 1988 and 2000 and who had a minimum follow up of 24 months were analysed by us. Eighty-six patients were men and 47 were women. Five were lost to follow-up. Mean age was 22.3 (7–54) years. Osteosarcoma was the most common tumour and comprised 66% of the patients. Giant cell tumour was present in 35% of the patients. The other tumours encountered were chondrosarcoma, malignant fibrous histiocytoma and Ewing's sarcoma. Histopathological diagnoses are shown in Table 1. Patients were followed up at regular intervals—monthly during the first year, every 6 months in the second year and yearly thereafter. The mean follow-up period was 59 (24–152) months.
Staging evaluation consisted of plain radiography, CT scan, Technetium 99m bone scans and digital subtraction angiography when appropriate. In the later part of the series, MRI was preferred to CT scan in the evaluation. Closed needle biopsy was the preferred method of biopsy. However, a majority of patients were referred to us after an open biopsy performed elsewhere.
Staging was done according to the Musculoskeletal Tumour Society (MSTS) system [8]. The majority of patients belonged to stage II; 39 had stage I and two had stage III tumours.
Pre-operative chemotherapy was administered to 81 patients according to the regimen in use at that particular time. Two patients with giant cell tumour presented to us after receiving radiotherapy. Fifty-six patients received post-operative chemotherapy.
Measurement radiography and, in some cases, CT scan and MRI, were used to estimate the size of the prosthesis to be used. All prostheses were indigenously manufactured, using stainless steel in 108 and titanium in 25. The total knee prosthesis was used most commonly and the intercalary prosthesis in the remaining patients. A more constrained type of prosthesis was used initially, which was later modified to a rotating hinge variety.
Surgically, an anterior midline incision encircling the biopsy scar was used. A wide margin of resection was achieved in 100 patients, while a marginal margin was accepted in 33. In 81 patients the tibial length resected was between 100–150 mm, and 38 had resection lengths between 151 and 200 mm.
A medial gastrocnemius rotation flap was used routinely in all patients. The extensor mechanism was repaired by direct suturing of the patellar tendon to the transposed flap. Preoperative and postoperative radiographs are shown in Figs. 1 and 2.
Results
The functional outcome was analysed based on the modified rating system of the MSTS [9]. An excellent result was achieved in 63 patients, good in 36, fair in 8 and poor in 21 (Table 1).
At the latest follow-up, 102 patients had no evidence of disease, 24 had died due to disease and two were alive with disease (Table 1).
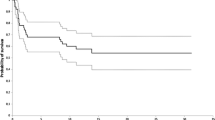
Survivorship analysis was done using the Kaplan–Meier estimator; and prosthesis, limb and patient survival was analysed. The 5-year prosthetic survival was 84.5%, the 5-year limb survival 85.5% and the 5-year patient survival was 79.1%.
Complications
Infection was the most common, present in 16 patients. It was controlled in three by antibiotics, ten underwent amputation and the prosthesis was removed in three. Flap necrosis occurred in five patients.
Periprosthetic fracture occurred in 12 patients, of whom revision was done in seven. Fracture incidence was high in the early part of the series, which declined over the years, probably due to advances in implant design and manufacture. Aseptic loosening was present in five patients, four of whom underwent revision and one had an excellent functional outcome despite evidence of loosening. Disassembly and bending of the prosthesis occurred in one patient each.
Ten patients with osteosarcoma developed pulmonary metastasis; eight of them died, one was lost to follow-up and one is alive. Local recurrence was encountered in four patients, all of whom had osteosarcoma. Amputation was done in three patients, of whom two died.
Discussion
The issue of limb salvage versus amputation has been raised by several authors during the past decade. The overall survival, quality of life, function and disability have been found to be the same for both procedures [11, 20], although there is an increased risk of local recurrence in patients with limb salvage [22]. Limb salvage, however, has a definite cosmetic advantage when compared to amputation [20].
There are various options available for reconstruction after proximal tibial tumour resection. Rotationplasty [10] gives excellent functional success in children [16] but has a very low patient acceptability [13]. Resection arthrodesis achieves excellent stability but has the major drawback of lack of knee motion [2]. Osteochondral allografts have been used for benign and low-grade malignant tumours but have several complications like a high rate of infection, allograft fracture, non-union and joint instability [5, 18, 25].
The advantages of endoprosthetic replacement are cost-effectiveness [11], early resumption of knee function and unassisted ambulation [1, 6, 13, 25] and lower energy expenditure than an above-knee amputation and fitting with a prosthesis [19]. Gait and stride length are, however, not significantly different between endoprosthetic replacement and above-knee amputation using an external prosthesis [26]. Endoprosthetic replacement is also associated with several possible complications like failure of primary wound healing, flap necrosis, secondary infection, aseptic loosening, fracture and breakage [1, 13, 15, 24, 25].
The proximal tibia is the most technically demanding site for limb salvage surgery. The medial gastrocnemius rotation flap has provided a very satisfactory method of overcoming the two major problems in managing proximal tibial tumours, namely, providing soft-tissue cover for the metallic endoprosthesis and maintaining continuity of the extensor mechanism [6, 17]. The method described by Malawer and McHale [17] has been used by us, and we have achieved an excellent MSTS functional outcome in 49.6% and good in 27% of patients. The issue of extensor lag still remains one of the major causes for a decreased functional outcome after proximal tibial endoprosthetic replacement [23]. The mean extensor lag in our series was 18 (10–35)°. The use of extramedullary porous coating materials in the endoprosthesis has been shown by several authors to overcome this mechanical disadvantage. This is because a pseudocapsule forms around the prosthesis and the soft tissues adhere to it by scar tissue and exert their pull through the pseudocapsule, moving the limb more effectively [7].
The 5-year prosthetic survival in our series was 84.5% and patient survival 79.1%. Horowitz et al. [14], in a series of 16 patients, used a constrained prosthetic design for the proximal tibia and reported a 5-year prosthetic survival of 54% and patient survival of 93%. The 5-year survival of patients with proximal tibial tumours is superior to other sites, as observed by several authors, and is probably due to the smaller lesion size at presentation due to earlier detection [14, 17].
The most common complication encountered by us was infection, which is consistent with other series [12, 24], occurring in 16 (12%) patients. Grimer et al. [12] reported a 33% infection rate in endoprosthetic proximal tibial replacement, which—with improved soft-tissue cover techniques like the medial gastrocnemius flap—decreased to 12% [13]. The various factors contributing to the high rate of infection are duration of surgery, extensive tissue exposure and immunocompromise due to chemotherapy and pre-operative radiotherapy [13]. Periprosthetic fracture occurred in 12 (9%) of our patients and is probably due to the increased demands posed by return to normal activity in young patients [13, 14].
Four patients with osteosarcoma had local recurrence, three of whom underwent amputation; two died within a year, indicating that local recurrence is a poor prognostic factor for survival [4]. Aseptic loosening was observed in five of our patients. Unwin et al. [24] have stated that the risk of aseptic loosening of proximal tibial endoprosthesis was higher in younger patients and in patients who had a greater percentage of tibial shaft resection. We used the rotating hinge prosthesis in the majority of patients, and this design has been proved to dramatically reduce the incidence of aseptic loosening [4].
The management of proximal tibial tumours still continues to be one of the most challenging areas in orthopaedic oncology. Achieving optimal results, by any method, proves to be a daunting task due to the various anatomical factors unique to this site. Though there are several methods of reconstruction available, all of them have several drawbacks that outweigh the potential benefits. Custom megaprosthetic replacement has emerged as the accepted modality of treatment for malignant proximal tumours, as it has been proved to produce a good functional result with an acceptable rate of complications. However, careful patient selection, a precise pre-operative work-up and a meticulous surgical technique are essential to achieve the desired outcome.
References
Abudu A, Carter SR, Grimer RJ (1996) The outcome and functional results of diaphyseal endoprosthesis after tumour excision. J Bone Joint Surg [Br] 78:652–657
Benevenia J, Makley JT, Locke M, Gentili A, Heiner J (1994) Resection arthrodesis of the knee for tumour: large intercalary allografts and long intramedullary nail technique. Semin Arthroplasty 5:76–84
Bramwell VH, Burgers M, Sneath R, et al (1992) A comparison of two short intensive adjuvant chemotherapy regimens in operable osteosarcoma of limbs in children and young adults. J Clin Orthop 10:1579–1591
Cannon SR (1997) Massive prosthesis for malignant bone tumours of the limbs. J Bone Joint Surg [Br] 79:497–506
Clohisy DR, Mankin HJ (1994) Osteoarticular allografts for reconstruction after resection of a musculoskeletal tumour in the proximal end of the tibia. J Bone Joint Surg [Am] 76:549–554
Eckardt JJ, Matthews JG, Eilber FR (1991) Endoprosthetic reconstruction after bone tumour resections of the proximal tibia. Orthop Clin North Am 22:149–160
Eckardt JJ, Yang R, Ward WG, Kelly C, Eilber FR (1995) Endoprosthetic reconstruction for malignant bone tumours and nonmalignant tumourous conditions of bone. Advances in operative orthopaedics vol 3, Mosby, pp 61–83
Enneking WF (1986) A system of staging musculoskeletal neoplasms. Clin Orthop 204:9–24
Enneking WF, Dunham W, Gebhardt MC, Malawer M, Pritchard DJ (1993) A system for the functional evaluation of reconstructive procedures after surgical treatment of tumours of the musculoskeletal system. Clin Orthop 286:241–246
Gottasauner-Wolf F, Kotz R, Knahr K, et al (1991) Rotationplasty for limb salvage in the treatment of malignant tumours at the knee: a follow-up of seventy patients. J Bone Joint Surg [Am] 73:1365–1375
Grimer RJ, Carter SR, Pynsent (1997) The cost-effectiveness of limb salvage for bone tumours. J Bone Joint Surg [Br] 79:558–561
Grimer RJ, Carter SR, Sneath RS (1989) Endoprosthetic replacements of the proximal tibia. In: Langlais F, Tomeno B (eds) Limb salvage: major reconstructions in oncologic and non-tumoral conditions. Springer, Berlin, Heidelberg, New York, pp 285–292
Grimer RJ, Carter SR, Tillman RM, Sneath RS, Walker PS, Unwin PS, Shewell PC (1999) Endoprosthetic replacement of the proximal tibia. J Bone Joint Surg [Br] 81:488–494
Horowitz SM, Glasser DB, Lane Jm, Healey JH (1993) Prosthetic and extremity survivorship after limb salvage for sarcoma. How long do the reconstructions last? Clin Orthop 293:280–286
Illyas I, Younge D, Pant R, Moeau P (2000) Limb salvage for proximal tibial tumours using modular endoprosthesis. Int Orthop 24:208–211
Kotz R. (1997) Rotation plasty. Semin Surg Oncol 13:34–40
Malawer MM, McHale WA (1989) Limb sparing surgery for high-grade malignant tumours of the proximal tibia: Surgical technique and a method of extensor mechanism reconstruction. Clin Orthop 239:231–248
Mankin HJ, Gebhardt MC, Tomford NW (1987) The use of frozen cadaveric allografts in the management of patients with bone tumours of the extremities. Orthop Clin North Am 18:275–289
Otis JC, Lane JM, Kroll MA (1985) Energy cost during gait in osteosarcoma patients after resection and knee replacement and after above-knee amputation. J Bone Joint Surg [Am] 67:606–611
Postma A, Kingma A, De Ruiter JH, et al (1992) Quality of life in bone tumour patients comparing limb salvage and amputation of the lower extremity. J Surg Oncol 51:47–51
Rosun G, Nirenberg A (1985) Neoadjuvant chemotherapy for osteogenic sarcoma: A five year follow up (T-10) and preliminary report of New studies (T-12). Prog Clin Biol Res 201:39–51
Rougraff BT, Simon MA, Kneisl JS, Greenberg DB, Mankin HJ (1994) Limb salvage compared with amputation for osteosarcoma of the distal end of the femur. J Bone Joint Surg [Am] 76:649–656
Sanjay BK, Moreau.PG (1999) Limb salvage in bone tumour with modular endoprosthesis. Int Orthop 23:41–46
Unwin PS, Cannon SR, Grimer RJ, Kemp KBS, Sneath RS, Walker PS (1996) Aseptic loosening in cemented custom—made replacements for bone tumours of the lower limb. J Bone Joint Surg [Br] 78:5–13
Yaw KM, Wurtz LD (1991) Resection and reconstruction for bone tumours in the proximal tibia. Orthop Clin North Am 22:133–48
Zohman YL, Boardmon DL, Eckardt JJ, Lane JM (1997) Stride analysis after proximal tibial replacement. Clin Orthop 339:180–184
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Natarajan, M.V., Sivaseelam, A., Rajkumar, G. et al. Custom megaprosthetic replacement for proximal tibial tumours. International Orthopaedics (SICOT) 27, 334–337 (2003). https://doi.org/10.1007/s00264-003-0484-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-003-0484-3