Abstract
Twelve adult New Zealand white rabbits were randomly divided into two groups. In group 1, 30% of the central mass of the right patellar tendon was removed. In group 2, 60% was removed. The left knees served as controls. The animals were killed 1 year later. The patella–patellar tendon–tibial tuberosity units of all knees were studied using histological and morphometric analysis. In both groups, the tendons had lengthened. Lengthening average was 2.50 mm in group 1 and 8.17 mm in group 2. In both groups, histology revealed poor alignment of the collagen fibres and high cellularity, although the findings in group 1 were nearer the normal histological pattern. The results suggest that removal of significant portions of the patellar tendon leads to lengthening of the resulting tendon. In clinical practice, it seems prudent to pay attention to the dimensions of the patellar tendon when harvesting a graft.
Résumé
Douze lapins adultes blancs (Nouvelle Zélande) étaient divisés au hasard en deux groupes. Dans le groupe 1 30% de la masse centrale du tendon rotulien droit ont été enlevés. Dans le groupe 2 60% ont été enlevés. Les genoux gauches ont servi comme contrôle. Les animaux ont été sacrifiés une année plus tard. Les unités "rotule—tendon rotulien—tubérosité tibiale" de tous les genoux ont été étudiés avec histologie et analyse morphométrique. Dans les deux groupes les tendons s'étaient allongés. La moyenne de l'allongement était 2.50 mm dans le groupe 1 et 8.17 mm dans le groupe 2. Dans les deux groupes l'histologie a révélé un mauvais alignement des fibres collagènes et une cellularité haute, bien que les résultats dans le groupe 1 étaient plus proches du modèle histologique normal. Les résultats suggèrent que la suppression d'une partie importante du tendon rotulien conduit à son allongement. En pratique clinique il paraît prudent de faire attention aux dimensions du tendon rotulien quand on prélève une greffe.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
The central third of the patellar tendon (PT) is one of the preferred sites for reconstruction of the knee anterior cruciate ligament (ACL) due to its biomechanical qualities [5, 6, 8, 12, 15].The usual dimensions of these bone-tendon-bone grafts tend to oscillate between 9 and 11 mm [8] while the PT has an average width of 3 cm at its proximal origin and 2 cm at the distal insertion, although with notable variations between individuals [18].
A growing number of complications in surgical reconstruction of the ACL are related to alterations produced in the donor site of the graft [2, 3, 10, 14, 15, 16, 17, 19]. Several studies have analysed healing mechanisms and biomechanics of the PT after extraction of a third of its mass [1, 4, 9, 11, 13]. However, repercussions on the final length of the tendon have been seldom studied.
The objective of the present study is to analyse in an experimental model the morphological and histological repercussions that provoke the removal of grafts of different widths on the residual PT.
Material and methods
Twelve New Zealand white rabbits (eight males and four females) with mature skeletal bone were used. They were randomly divided into two groups. The rabbit was selected because of the anatomical analogy of its extensor mechanism with the human [7]. Care recommendations of our local animal experimentation ethical committee were followed throughout. The animals were operated on and subsequently caged in the experimental surgery area of our institution.
Surgical technique
Anaesthesia was a mixture of intramuscular anaesthetic (ketamine) and droperidol-fentanyl. After preparing a standard surgical field, an average longitudinal approach of approximately 3 cm was made in the right knee. The left knee was kept as a healthy control. The paritenon was divided and the PT individualised, registering its width with a calliper of 0.05 cm precision. The experiment consisted of creating longitudinal surgical defects in the central aspect of the PT that were analogous to those carried out in clinics in order to obtain bone-PT-bone grafts, although without bone blocks. The defects involved the whole length of the PT and randomly corresponded to 30% (group 1) or 60% (group 2) of its width. The tendon defect was left opened and the peritenon was sutured with Vicryl 3–0. After surgery, the animals were held until sacrifice in standard laboratory cages where they could move about without restriction. They were killed 1 year after surgery with a lethal dose of intracardiac ketamine.
Morphometric study
Immediately after killing, the patella-PT-tibial tuberosity unit was removed. After tensing to 20 N with the help of an Instron 4507 Universal Materials Testing Machine (Canton, Mass., USA), we went on to the measuring process. The length of the PT was taken as the distance between the patella and the tibial tuberosity. The initial and final weight of each animal showed no significant differences between the groups at the beginning or the end of the study (Table 1).
Histological study
Once the morphometric study was carried out, we proceeded to the histological study. The patella-PT-tibial tuberosity units of both the intervened and contralateral knees were fixed on fragments of expanded polyurethane with needles placed at their extremes to maintain tissue orientation. Thereupon, they were fixed by immersion in a solution of formaldehyde at 10% for 24 h for subsequent processing and embedded in paraffin. The cuts were stained with three different techniques: hematoxylin-eosin, Masson trichromic (to show collagen fibres) and Alcian blue (for acid mucopolysaccharides). A qualitative study of cellularity, the characteristics of the extra-cellular matrix and vascularisation was carried out on each specimen. We took the non-intervened contralateral tendon as the normal pattern and reference.
Statistical study
The size of the sample was calculated as statistically significant (p<0.05) with a statistical strength of 80%, a difference between the lengths of the healthy tendon and the one operated on of 5 mm with a standard deviation (SD) of 2 mm. A statistical analysis was done by comparing the length of the operated tendons (groups 1 and 2) with respect to their controls, and the length differences between the operated tendons of group 1 with respect to those of group 2. Student's t-test for analysis of independent data was used.
Results
Defect
The average defect was 5.8 mm in group 1 and 8.3 mm in group 2. There were no significant differences between the original PT widths of either group. However, width difference in the surgically created defects were significant (Table 2).
Final tendon length
The average post-surgical length for group 1 was 12.5% greater than control, without statistical significance. The post-surgical length in group 2 was 38% greater than its control reaching statistical significance (Table 3).
Histology
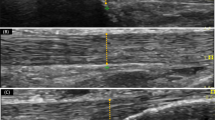
Control tendons showed a constant pattern and well-defined homogenous collagen fibres arranged in a parallel way amongst them in the direction of traction with hardly any extracellular matrix or vascular structures. There was also a low nuclear density that reflected scarce cellularity. Identical characteristics, corresponding to mature tendinous tissue could be seen in the peripheral zones of sections of the intervened PTs, independently of the created defect size.
Regenerated tissue did not reproduce this normal micro-anatomy but did show different degrees of alteration. Thus, the central part of the histological cuts showed newly formed collagen in diverse states of maturity and orientation. The newly formed tissue evidenced great density of cellular nucleus and an extracellular matrix with an abundant mucopolysaccharide component. Group 1 showed a histological pattern (Fig. 1) closer to normality than that of group 2 (Fig. 2), understanding this as the observed in a healthy tendon in terms of number of cells, characteristics of the extra-cellular matrix and orientation of collagen fibres.
Discussion
Modification of PT length in which a third of its mass is extracted has received little attention in medical literature. However, these changes in length have potentially great importance, as they cause modifications in the position of the patella that can induce abnormal loads on the patellar joint and anterior knee pain.
Burks et al. reported in a canine model that 6 six months after removal of the central third, the PT shortened by 10% and showed a loss of resistance up to 60% of control [4]. Beynnon et al., with a similar approach and utilising the rabbit, obtained similar results in terms of the loss of PT strength after 6 months. However, they did not mention any change of length [1]. It was hypothesised that immobilisation and lack of active quadriceps contraction could favour shortening of the PT. Kamps et al. [9] studied in rabbits the repercussion on regenerated tendon from a forced rehabilitation protocol in front of another of postoperative immobilisation. In the tendons subjected to early mobility, results showed the appearance of micro-lesions and an increase of the tendon section by ×4.1 and a longitudinal lengthening by ×1.2 with respect to control. Meanwhile, the cross-section area and lengthening were inferior in the immobilised group. Histologically, tendons from the immobilised group showed better alignment of collagen fibres and a reduction in extension of the remodelled tissue.
O'Brien et al. were the first to report elongations of the PT after removal of its middle third in human beings. In their series, up to 20% of patients suffered lengthening of the PT, and a direct correlation between these increases in length and the presence of patellofemoral problems could be established [12]. Shelbourne et al. evaluated the height of the patella and the length of the PT in a series of 71 ACL reconstructions carried out with bone-PT-bone autografts. They found an average PT shortening less than 1% of initial length [17]. On the other hand, the same group specifically studied morbidity linked to extraction of the middle third of the PT. They obtained grafts from the uninjured contralateral knee and concluded that morbidity induced by graft extraction appeared to be of short duration and reversible. However, they recognised that the patient experienced quadriceps weakness and tendonitis in the operated PT for at least 6 months [15].
Follow-ups by MRI of the PT of which the middle third had been extracted usually coincide with the tendency of progressive filling of the defect with scar tissue [11]. In a goat model, 21 months after the extraction, the PT showed swelling of the section area by 300% with respect to control, while the ultimate strength of regenerated tissue hardly reached 50% of the original one [13].
Results of the present work show that defects of 30% of the mass of the PT lead to its significant lengthening in rabbits, and this agrees with results obtained by Kamps et al.[9] Presumably, this is due to a worsening of biomechanical properties. Although in clinical practice grafts of between 9 and 11 mm wide are normally taken, few works make reference to the total width of the PT. Given that humans possess notable inter-individual anatomical differences, it is probable that, sometimes, grafts of more than 30% of the tendon mass can be obtained. This fact may help explain lengthenings and tears or breakages of the PT secondary to taking grafts. These alterations may be explained by the histological changes observed, especially disorganisation of the collagen fibre network, last structure to give the tendon its biomechanical tensile strength, tear resistance and elasticity characteristics [20].
Although the rate of complications induced by extraction of a significant portion of the PT is probably very low in relation to the large number of reconstructions carried out, the potential importance of these complications advise caution in the extraction of these types of grafts. Special attention should be paid to the width of the PT in its tibial insertion where it is anatomically narrower.
References
Beynnon BD, Proffer D, Drez DJ, Stankewich CJ, Johnson RJ (1995) Biomechanical assessment of the healing response of the rabbit patellar tendon after removal of its central third. Am J Sports Med 23:452–457
Bonamo JJ, Krinick RM, Sporn AA (1984) Rupture of the patellar ligament after use of its central third for anterior cruciate reconstruction. J Bone Joint Surg [Am] 66:1294–1297
Bonatus TJ, Alexander AH (1991) Patellar fracture and avulsion of the patellar ligament complicating arthroscopic anterior cruciate ligament reconstruction. Orthop Rev 20:770–774
Burks RT, Haut RC, Lancaster RL (1990) Biomechanical and histological observations of the dog patellar tendon after removal of its central one-third. Am J Sports Med 18:146–153
Clancy WG, Nelson DA, Reider B, Narechania RG (1982) Anterior cruciate ligament reconstruction using one-third of the patellar ligament, augmented by extra-articular tendon transfers. J Bone Joint Surg [Am] 64:352–359
Frank C, Jackson DW (1997) The Science of reconstruction of the anterior cruciate ligament. Current Concepts Review. J Bone Joint Surg [Am] 79:1556–1576
Gomez-Barrena E, Fernandez-Baillo N, Ordoñez JM, Martinez E (1991) La rodilla en el animal de experimentación. Morfología y cinemática comparadas y su aplicación a los modelos experimentales de rodilla. Rev Ortop Traum 35:100–112
Jackson DW, Lemos MRJ (1993) Autograft reconstruction of the anterior cruciate ligament. Bone-patellar tendon-bone. In: Jackson DW (ed) The anterior cruciate ligament: current and future concepts. Raven, New York, pp 291–303
Kamps BS, Linder LH, De Camp CE, Haut RC (1994) The influence of immobilization versus exercise on scar formation in the rabbit patellar tendon after excision of the central third. Am J Sports Med 22:803–811
Marumoto JM, Mitsunaga MM, Richardson AB, Medoff RJ, Mayfield GW (1996) Late patellar tendon ruptures after removal of the central third for anterior cruciate ligament reconstruction. Am J Sports Med 24:698–701
Nixon RG, SeGall GK, Sax SL, Cain TE, Tullos HS (1995) Reconstitution of the patellar tendon donor site after graft harvest. Clin Orthop 317:162–171
O'Brien SJ, Warren RS, Paulov H, Panariello R, Wickiewicz TL (1991) Reconstruction of the chronically insufficient anterior cruciate ligament with the central third of the patellar ligament. J Bone Joint Surg [Am] 73:278–286
Proctor CS, Jackson DW, Simon TM (1997) Characterization of the replacement tissue after harvesting the central one-third of the goat patellar tendon. Trans Orthop Res Soc 74:13
Recht MP, Piraino DW, Applegate G, Richmond BJ, Yu J, Parker RD, Andrisch JT (1996) Complications after anterior cruciate ligament reconstruction: radiographic and MR findings. Am J Roentgenol 167:705–710
Rubinstein RA, Shelbourne D, VanMeter ChD, McCarroll JC, Rettig AC (1994) Isolated autogenous bone-patellar tendon-bone graft site morbidity. Am J Sports Med 22:324–327
Sachs RA, Daniel DM, Stone ML, Garfein RF (1989) Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med 17:760–765
Shelbourne KD, Patel DV (1996) Prevention of complications after autogenous bone-patellar tendon-bone ACL reconstruction. In: Pritchard DJ (ed) Instructional course lectures, vol 45. American Academy of Orthopaedic Surgeons, pp 253–262
Testut L, Latarjet A (eds) (1979) Tratado de Anatomía Humana. Tomo I. Salvat Editores, S.A. Barcelona
Wojtys EM, Oakes B, Lindenfeld TN, Bach BR (1997) Patella Infera Syndrome: an analysis of the patellar tendon pathology. In: Springfield DS (ed) Instructional course lectures, vol 46. American Academy of Orthopaedic Surgeons, pp 241–250
Woo SLY, Young EP (1991) Structure and function of tendons and ligaments. In: Mow VC, Hayes WC (eds) Basic orthopaedic biomechanics. Raven, New York, pp 199–243
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Monllau, J.C., Hinarejos, P., Alvarez, P. et al. Influence of autograft removal on rabbit patellar tendon length. International Orthopaedics (SICOT) 28, 7–10 (2004). https://doi.org/10.1007/s00264-003-0448-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-003-0448-7