Abstract
Background
We conducted a phase I dose escalation study to evaluate the safety and immunologic response to peptide immunomodulatory vaccines GL-0810 (HPV16) and GL-0817 (MAGE-A3) in HPV16 and MAGE-A3-positive RM–SCCHN patients, respectively.
Methods
Three dose levels (500, 1,000, and 1,500 µg) of GL-0810 or GL-0817 with adjuvants Montanide (1.2 ml) and GM-CSF (100 µg/m2) were administered subcutaneously q2 weeks for a total of four vaccinations in HPV16 and MAGE-A3-positive RM–SCCHN patients, respectively.
Results
Nine and seven patients were enrolled in the HPV16 and MAGE-A3 cohorts, respectively. No dose-limiting toxicities were observed, and toxicity was predominantly local and grade 1 (erythema, pain, and itching at the injection site). In those patients who received all four vaccinations, 80 % (4/5) of the HPV16 cohort and 67 % (4/6) of the MAGE-A3 cohort developed antigen-specific T cell and antibody responses to the vaccine. Significant concordance between T cell and antibody responses was observed for both groups. No clear dose–response correlation was seen. All patients progressed by RECIST at first repeat imaging, except for one patient in the MAGE-A3 500 µg cohort who had stable disease for 10.5 months. The median PFS and OS for the MAGE-A3 cohorts were 79 and 183 days, respectively, and for the HPV16 cohort 80 and 196 days, respectively.
Conclusions
GL-0810 and GL-0817 were well tolerated in patients with RM–SCCHN with T cell and antibody responses observed in the majority of patients who received all four vaccinations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Squamous cell carcinoma of the head and neck (SCCHN) is the sixth most common malignancy worldwide [1]. Despite aggressive initial definitive therapy, select groups of patients with SCCHN are at high risk of the development of second primary tumors, and a significant proportion of patients will recur, commonly within the first 2 years [2]. Unfortunately, a significant proportion of these patients will not have a salvage surgical or radiation option, and the median survival for locoregionally recurrent or metastatic disease treated with palliative chemotherapy alone is a dismal 8–10 months [3]. New therapeutic modalities are desperately needed for this patient population.
In an effort to improve outcomes for recurrent/metastatic SCCHN patients, we developed two separate peptide immunomodulatory vaccines using HLA-I and HLA-II T cell epitopes of the human papillomavirus type 16 (HPV16) and melanoma antigen E (MAGE)-A3 tumor-associated antigens. The human papillomavirus (HPV) now has an established role in the etiology of squamous cell carcinoma of the oropharynx [4]. HPV16 was chosen because it accounts for the majority of cases (68–87 %) of HPV-positive head and neck cancer worldwide [5, 6] Additionally, tumor specificity and the presence of well-defined peptide epitopes make it an ideal target [7–9].
Melanoma antigen E (MAGE-A3) is a cancer–testis antigen. Cancer–testis antigens are expressed by human tumors of different histological types and have limited expression in normal parenchyma [10]. For example, MAGE-A3 was originally discovered in melanomas and has subsequently been identified in various epithelial cell malignancies including head and neck cancer where it has been found in upward of 51 % of cases [10, 11]. Importantly, MAGE-A3 expression may be associated with a more aggressive course, as several studies suggest that MAGE-A3 may be a negative prognostic indicator in hematologic malignancies [12, 13]. Additionally, expression has been associated with more advanced stage in squamous cell carcinoma of the larynx [11]. Therefore, MAGE-A3 was chosen based on its tumor specificity, high percent expression, and the existence of previously defined HLA-I and HLA-II immunostimulatory epitopes [14, 15].
In order to improve the efficacy of these vaccines, we incorporated several unique features into their design. First, we included a “penetrin” sequence derived from HIV-TAT (RKKRRQRRR) which facilitates peptide translocation through the cell membrane directly to the endoplasmic reticulum and golgi apparatus to form peptide-HLA complexes [16]. Additionally, the junction of multiple HLA-I and HLA-II peptide epitopes via furin-cleavable linkers allows the release of individual epitopes when cleaved in the Golgi [17, 18]. Furthermore, the inclusion of both HLA-I and HLA-II epitopes facilitates both cytotoxic T cell activation and stimulation of the CD4 T helper cell response, important for development of tumor-specific memory T cell and humoral immunity [19–22]. Finally, the combination of Montanide ISA 51 and granulocyte macrophage colony stimulating factor (GM-CSF) is postulated to enhance antigen presentation and promote dendritic cell migration to the site of vaccination [23].
Based on promising preclinical data with these immunomodulatory peptide vaccines [17], we initiated a pilot study in five patients with recurrent or metastatic SCCHN (RM–SCCHN). This pilot study demonstrated that these immunomodulatory peptide vaccines in combination with GM-CSF and Montanide adjuvant were well tolerated and able to stimulate antigen-specific cellular and humoral immunity. Although there were no documented responses, one patient was still alive 31 months post therapy [18]. In order to evaluate the safety of these vaccines in a larger patient cohort and investigate how peptide dose correlates with development of antigen-specific immunity, we performed the current phase I dose escalation trial. Our data from this study reaffirm the feasibility and safety of this vaccine-based approach and document a striking correlation between the development of antigen-specific T cell and humoral immunity which will facilitate monitoring of subsequent pivotal studies. Furthermore, the lack of clinical efficacy in the face of a clear immunological response suggests that these vaccines may be most clinically relevant in resected SCCHN patients at high risk of disease recurrence and/or in combination with manipulation of specific co-signaling pathways.
Materials and methods
We conducted a single center phase I dose escalation study at the University of Maryland Greenebaum Cancer Center (UMGCC) to evaluate the effect and safety of three dose levels (500, 1,000, and 1,500 µg) of HPV16 (GL-0810) or MAGE-A3 (GL-0817) immunomodulatory peptide vaccine in combination with adjuvant Montanide and GM-CSF in HPV16 or MAGE-A3 expressing RM-SCCHN patients, respectively. The primary objectives of the study were to establish safety and the adequate biologic dose for this vaccine defined by immune response (see below).
Patient selection
Eligibility criteria included age >18 years, PS 0–2, biopsy proven progressive, recurrent (postsurgical, radiation therapy, chemotherapy, and combination therapy) or metastatic SCCHN which by the judgment of the treating physician was incurable by standard treatment modalities, or the patient was unwilling to be treated with surgery, chemotherapy or radiation therapy. A patient’s tumor must have tested positive for either MAGE-A3 or HPV16. Main exclusion criteria included known HIV infection, patients with any malignant disease to the CNS or in a location that would put the patient at significant risk should an inflammatory response occur, patients undergoing treatment with systemic immunosuppressants and/or had an immunocompromising condition, or other active cancer requiring therapy or history of malignancy that was expected to effect life expectancy. Patients could not be treated with other cancer therapy concurrent with vaccine and could not have received chemotherapy, immunotherapy, biologic therapy, or radiation therapy within 4 weeks of the date of first vaccination.
Importantly, an HLA-A*02 genotype was not included as an entry criteria for this trial. The decision to eliminate HLA typing from the inclusion criteria was based on the fact that observed immunologic responses in the pilot study were predominantly directed against the HLA-II vaccine epitopes. Based on the knowledge that class II molecules have an open binding groove and, as such, have less stringent requirements for recognition we anticipated that patients bearing diverse HLA-II genotypes could respond to the class II vaccine epitopes [18].
Study design
Patients meeting initial inclusion/exclusion criteria underwent a biopsy of accessible tumor for determination of HPV16 and MAGE-A3 status. Patients with HPV16-positive tumors were assigned to cohort 1 and were treated with HPV16 immunomodulatory peptide vaccine GL-0810 plus adjuvant, and those with MAGE-A3-positive tumors were assigned to cohort 2 and treated with MAGE-A3 immunomodulatory peptide vaccine GL-0817 plus adjuvant. If a patient’s tumor was both MAGE-A3 and HPV16 positive, they were enrolled in the cohort with the fewest patients.
Both cohorts 1 and 2 ran independently of each other. Three dose levels (500, 1,000, and 1,500 µg) of HPV16 or MAGE-A3 immunomodulatory vaccines were tested in sequential groups of patients. Each peptide was admixed with fixed doses of the adjuvants Montanide (1.2 ml) and GM-CSF (100 µg/m2) and given together as one injection. A total of four vaccinations were administered subcutaneously in the inguinal region at 2-week intervals. Dose escalation occurred in each cohort once three subjects from the preceding dose level received at least two of the planned four vaccinations, and no patient experienced a dose-limiting toxicity (DLT). Doses were not escalated in any individual patient. If two or more patients experienced a DLT at a given dose level, accrual at that dose would be halted, and the preceding dose level would be expanded to six patients. Data were to be analyzed after at least three vaccinated patients had received a dose that was tolerated. The dose that provided an adequate immunologic response was to be expanded by nine patients for a total of 12 patients at that particular dose. Therefore, the maximum number of subjects that could be enrolled in each of the two cohorts was 24 (6 + 6 + 12).
An adequate biological dose was to be defined by a fivefold increase in interferon (IFN)-γ expression level in the ELISPOT assay after the first 2 weeks of therapy. If an adequate biological response was not generated in a majority of patients at any dosage, then the dose at which the greatest increase in IFN-γ would be expanded.
Screening of patients took place within 30 days prior and baseline evaluations within 7 days prior to the first vaccination. During the screening phase, patients underwent PET/CT for baseline radiographic evaluation (up to 6 weeks prior to the first vaccination) as well as tumor biopsy to determine MAGE-A3 and HPV16 expression. After each vaccination, the patient was observed for 4 h with vital signs and evaluation of the injection site pre dose, immediately post injection, 0.5, 1, 2 and 4 h post dosage. Subjects were evaluated at each vaccination visit, 2 and 6 weeks after the fourth vaccination, and thereafter every 3 months through month 24. At these visits, history and physical examination, adverse event recording, ECOG performance status, physical tumor measurements (if applicable) and blood draws for immune response evaluations were taken. A repeat PET/CT was done 6 weeks (±7 days) after the fourth vaccination (3 months after first vaccination).
Patients who, prior to completing the allotted number of peptide vaccinations, had disease progression, intolerable toxicity, or refused further treatment, had treatment discontinued and were followed until the end of the study.
Adverse events monitoring
Toxicity was defined as per the NCI Common Toxicity criteria for adverse events (CTCAE) version 3.0. Dose-limiting toxicity criteria are shown in supplemental Table 1. Discontinuation of an individual patient from the study was based on adverse events deemed related to the study medication as detailed in supplemental Table 2.
Disease monitoring
A maximum of three measurable lesions were identified as target lesions in each patient and were measured and recorded at baseline by physical examination and/or intravenous contrast enhanced PET/CT. Definition of complete response (CR), partial response (PR), stable disease (SD), or progressive disease (PD) was based on response evaluation criteria in solid tumors (RECIST 1.1).
Laboratory methods
Descriptions of MAGE-A3 and HPV16 peptides, isolation of peripheral blood mononuclear cells, MAGE-A3 and HPV16 analysis by PCR, Trojan-specific T cell response monitoring, Interferon-γ restimulation ELISPOT assay, MAGE-Trojan and HPV16-Trojan ELISA used in this study are found in our previously published pilot study [18]. Importantly, all ELISPOT assay results reported in this study included in vitro stimulation, to enhance response detection.
Statistical analysis
This phase I study was designed to evaluate the safety of the vaccines and establish an adequate biological dose of the HPV16 and MAGE-A3 peptide immunomodulatory vaccines. Based on the results of the pilot study [18], we did not anticipate serious toxicity, and therefore a true MTD was not anticipated, but an adequate biologic dose was sought. Descriptive statistics were utilized to describe the incidence of adverse effects as defined by CTCAE version 3.0.
A biological (immunological) response was defined as a binary (positive vs. negative) response measured in each patient after treatment with either HPV16 or MAGE-A3 immunomodulatory peptide vaccine. Positive response was defined as an at least fivefold increase in interferon (IFN)-γ expression level in the ELISPOT assay after the first 2 weeks of therapy. An adequate dose was defined as a dose that provided a high response rate. The goal of the design was to find a biologically ‘adequate’ dose, while using a very small number of patients, because optimal biological dose may not exist or require a large number of patients.
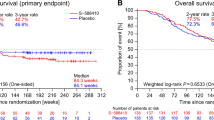
Additional endpoints included progression-free survival (PFS), response and overall survival (OS). PFS and OS functions were estimated using the Kaplan–Meier approach. PFS time was defined as the time from first treatment to documentation of progression or death. If a patient died without a progression documented, the patient would be considered to have progressed on their death date. OS time was defined as the time from first treatment until death or censored at the last date of patient contact. Response evaluations including CR, PR, SD, and PD were defined as detailed above.
The exact McNemar test at the 0.05 level of significance was used to assess whether there was a concordance between T cell and antibody responses for patients treated with the HPV16 and MAGE-A3 vaccines. Statistical analysis was conducting using R (v.3.0.2).
Results
Patient demographics
Between 2008 and 2012, 56 patients were screened for enrollment on the clinical trial. Forty-four patients underwent biopsy for evaluation and nine patients tested positive for MAGE-A3, 12 for HPV16, and two were positive for both HPV16 and MAGE-A3. A total of 17 patients were enrolled on the protocol. One patient was subsequently discovered to be ineligible and was taken off of the study. Therefore, there were 16 evaluable patients including nine patients in the HPV16 cohort and seven patients in the MAGE-A3 cohort (Fig. 1). The study was closed prematurely on 7/11/13 due to poor accrual. All patients enrolled had completed treatment by this time, and one patient remained in survival follow-up.
Baseline patient characteristics are shown for the HPV16 and MAGE-A3-positive cohorts in Tables 1 and 2, respectively. The median age of the entire study population was 60, and all patients were male and predominantly white. In the HPV16 cohort, 89 % of patients had an oropharyngeal primary, whereas in the MAGE-A3 cohort, the primary site varied between oropharynx, hypopharynx, and larynx. The HPV16 cohort contained younger patients with disease that was predominantly metastatic, whereas MAGE-A3-positive patients had predominantly locoregional recurrence. HPV16-positive patients were more heavily pretreated with palliative chemotherapy compared to the MAGE-A3-positive patients.
Feasibility and toxicity
In the HPV16 cohort, three patients were vaccinated at each dose level (500, 1,000, and 1,500 µg). In the MAGE-A3 cohort, three patients were vaccinated at the 500 and 1,000 µg dose levels, while only one patient was treated at the 1,500 µg dose level. Eleven out of the 16 treated patients received all four vaccinations. In the HPV16 cohort, five out of nine patients completed all four vaccinations, and in the MAGE-A3 cohort, six out of seven patients received all four vaccines. Five patients progressed during vaccine therapy and therefore did not receive all four vaccinations.
Toxicity data are shown in Tables 3 and 4 for HPV16 and MAGE-A3 cohorts, respectively. Overall, the vaccine was well tolerated with predominantly local grade 1 toxicity including erythema, pain, and itching at the injection site. The patient receiving the MAGE-A3 vaccine at the highest dosage did experience grade 1 systemic symptoms including headache, nausea and chills. One patient receiving the MAGE-A3 vaccine at 500 µg, developed a pharyngocutaneous fistula 7 days after his first vaccination. This was treated conservatively and he received all remaining doses. No patients discontinued treatment early because of toxicity.
Immunologic outcomes
Interferon gamma (IFNγ) ELISPOT and ELISA assays were used to evaluate post vaccination peptide vaccine-specific T cell and antibody responses, respectively. ELISPOT and ELISA results for individual responding patients at the three vaccine dosages in the HPV16 cohort and MAGE-A3 cohort are shown in Figs. 2 and 3, respectively, and a summary of immunologic responses is shown in Table 5. In the HPV16 cohort, all patients who had a T cell response also had an antibody response, with 44 % (4/9) of patients having both a T cell and antibody response to the Trojan peptide vaccine. One patient (043) had a T cell response and antibody to HPV16 at baseline, which increased after the fourth vaccination. One patient (003) had an antibody response, but not a T cell response, and four patients had no detectable immunologic response to the vaccine. Amongst patients who received all four vaccinations, 80 % (4/5) had both T cell and antibody responses.
ELISPOT and ELISA results from HPV16-positive patients who had a response to vaccine. ELISPOT Assay: Collection of peripheral blood mononuclear cells (PBMCs) occurred before and after vaccination at time points shown in Figure 2. T cell reactivity measurements were carried out against human papillomavirus (HPV16)—Trojan- and individual Trojan-specific HLA class I (HPV–CTL) and Class II (HPV–HTL) using interferon-γ (IFN-γ) ELISPOT assays. Control values are shown without subtraction from experimental values. ELISPOT assays were performed with in vitro stimulation. Number of spots per 100,000 PBMCs is shown on the Y-axis. Antigen concentration was 10 μg/ml. Due to variation in response, some figures contain different increments for the Y-axis. ELISA Assay: HPV16-Trojan-specific immunoglobulin G (IgG) antibody response was evaluated before and after vaccination at time points shown in Figure 2. Absorbance data on the Y-axis represent mean optical density (OD) results from triplicate wells from three different plasma dilutions. a HPV16 500 µg cohort. b HPV16 1,000 µg cohort. c HPV16 1,500 µg cohort. *Patient 003 did not have a T cell response
ELISPOT and ELISA results from MAGE-A3-positive patients who had a response to vaccine. ELISPOT Assay: Collection of peripheral blood mononuclear cells (PBMCs) occurred before and after vaccination at time points shown in Figure 3. T cell reactivity measurements were carried out against MAGE-A3—Trojan- and individual Trojan-specific HLA class I (MAGE–CTL) and Class II (MAGE–HTL) using interferon-γ (IFN-γ) ELISPOT assays. Control values are shown without subtraction from experimental values. ELISPOT assays were performed with in vitro stimulation. Number of spots per 100,000 PBMCs is shown on the Y-axis. Antigen concentration was 10 μg/ml. Due to variation in response, some figures contain different increments for the Y-axis. ELISA Assay: MAGE-A3-Trojan-specific immunoglobulin G (IgG) antibody response was evaluated before and after vaccination at time points shown in Figure 3. Absorbance data on the Y-axis represent mean optical density (OD) results from triplicate wells from three different plasma dilutions. a MAGE-A3 500 µg cohort. b MAGE-A3 1,000 µg cohort. c MAGE-A3 1,500 µg cohort. *Patient 004 did not have a T cell response
In the MAGE-A3 cohort, all patients who had a T cell response also had an antibody response, with 57 % (4/7) of patients having both a T cell and antibody response to the peptide immunomodulatory vaccine. One patient (004) did not have a T cell response, but had antibody to MAGE-A3 at baseline. Two patients had no response to the peptide antigens by either ELISPOT or ELISA. Amongst patients who received all four vaccinations, 67 % (4/6) of patients had both a T cell and antibody response.
For both groups, there was significant concordance between T cell and antibody responses (p < 0.001), with T cell responses preceding antibody detection. Antibody titers were sustained in responding patients at the last time point of evaluation, with some patients having rising titers even at 3 months after the first vaccination. Higher dosages of vaccine did not appear to increase response rate but may lead to a more rapid T cell response. Due to the lower accrual, we were unable to determine the adequate biologic dosage based on our preplanned analysis parameters; however, given that all dosages were well tolerated, we anticipate that the highest dosage of 1,500 µg will be selected for further study in both cohorts.
Clinical outcomes
There were no complete or partial responses by RECIST. All patients progressed at first repeat imaging except for one patient in the MAGE 500 µg cohort (patient 017) who had stable disease. This patient withdrew consent but did continue to follow-up at UMGCC, and his disease was stable for 10.5 months off any therapy before progressing. The median PFS and OS for the MAGE-A3 cohort were 79 and 183 days, respectively, and for the HPV16 cohort 80 and 196 days, respectively.
Discussion
This novel phase I dose escalation trial, evaluated the safety and immune response at three different dose levels of MAGE-A3 (GL-0817) or HPV16 (GL-0810) immunomodulatory peptide vaccines with adjuvants Montanide and GM-CSF in patients with locally recurrent or metastatic MAGE-A3 or HPV16-positive SCCHN, respectively. The vaccines were well tolerated, and no dose-limiting toxicity was reached. In patients who received all four vaccinations, 80 % of HPV16 positive and 67 % of MAGE-A3-positive patients developed both a T cell and antibody response. In both groups, there was a significant correlation between T cell response and subsequent antibody response. However, these immune responses did not translate into any clinical responses as measured by RECIST.
Consistent with our findings from our pilot study [18], the preponderance of T cell responses were directed against the whole Trojan vaccine or the class II epitopes. The increased recognition of the whole Trojan vaccine may reflect an intrinsic bias in our assay design, necessitated by limited sample availability, in which PBMC were initially stimulated by the whole Trojan vaccine in vitro, with secondary stimulation using the intrinsic Class I and II peptide epitopes. Alternatively, it is possible that the increased responses to the whole vaccine are a result of “neo epitopes” generated by artificial linking of multiple epitopes. Finally, since this trial was conducted in patients with existing disease, if peptide T cells trafficked to the tumor site, their actual numbers could be artificially reduced in the peripheral blood. Unfortunately, we were unable to distinguish these possibilities in our study secondary to limited sample availability.
There was a significant correlation between T cell and antibody responses. As anticipated, in the majority of responding patients, the T cell response preceded the antibody response. While some T cell responses began to wane, most antibody responses continued to increase after the last vaccination. Higher doses in both the MAGE-A3 and HPV16 cohorts appeared to generate earlier, but not more robust responses. Although lower than expected accrual prevented statistical analysis to determine an adequate biologic dosage, given that all dosages were well tolerated and higher dosages may be associated with an earlier response, we anticipate that the 1,500 µg dosage will be used in subsequent trials.
Interestingly, two patients (one in HPV16 cohort and one in MAGE-A3 cohort) had baseline antibodies against their respective peptide vaccine. While antibodies to HPV16 E6 have been reported in up to 35 % of patients with squamous cell carcinoma of the oropharynx, even upward of 10 years before a diagnosis of cancer [24], baseline antibodies to MAGE-A3 are rarely found [21, 25].
Despite a T cell and antibody response in the majority of patients who completed all four vaccinations, we observed no clinical responses in either cohort. One patient in the MAGE-A3 500 µg cohort did have stable disease for 10.5 months. While appropriate endpoints for trials continue to be debated, despite the efficacy and recent approval of Sipuleucel-T for the treatment of metastatic castrate resistant prostate cancer, a pooled analysis of therapeutic vaccine trials published since 2004, involving multiple tumor types with a total of 973 patients, found an overall response rate of 3.6 % and a response rate of 3.7 % in trials that included only peptide vaccines [26]. Similar to our findings, analysis of published therapeutic cancer vaccine trials have shown that evidence of activation of the immune system by laboratory correlates has not translated into clinical responses [26].
To our knowledge, this trial as well as our previously published pilot study [18] represent the first published experience using therapeutic immunomodulatory peptide vaccines to treat RM-SCCHN. However, MAGE-A3 and HPV16 peptide vaccinations have been evaluated in the treatment of other cancers. For example, vaccination with MAGE-A3 peptide vaccines can stimulate cellular and humoral immune responses in both melanoma and NSCLC. [27, 28] While in NSCLC, the use of this vaccine has only been tested in the adjuvant setting [28], data evaluating the clinical efficacy of a MAGE-A3 peptide vaccine against active macroscopic disease exist in metastatic melanoma, demonstrating some activity in cutaneous or lymph node metastasis, but not visceral metastasis [25, 29, 30]. For example, Marchand et al. analyzed clinical response in 33 patients with stage III or IV metastatic melanoma treated with recombinant MAGE-A3 protein with immunological adjuvant SBAS-2. There were two partial responses and two mixed responses; however, there were no clinical responses in any patients who had visceral metastasis [29]. Therapeutic vaccines targeted against HPV have shown some clinical efficacy for precancerous lesions [31].
Potential reasons for lack of clinical efficacy in the face of an active immune response must be understood in order to effectively inform subsequent studies. Two of the major impediments to clinical efficacy are immunologic tolerance and patient selection. The causes of immunologic tolerance in SCCHN are the result of both tumor expression of molecules which dampen the immune response and active cellular suppression. For example, SCCHN cells can secrete immunosuppressive cytokines such as TGF-B, IL-10, and prostaglandin E2 (PGE2) [32, 33]. Additionally, tumor expression of B7-H1 (PD-L1) which inhibits the activity of PD-1 expressing CD4 and CD8 T cells, has been shown to be expressed in 40–70 % of SCCHN patients with higher expression in HPV-positive patients [34–36]. Furthermore, in HPV-positive SCCHN, early viral oncogenes E5, E6 and E7 can downregulate antigen processing and presentation [37, 38]. E5 and E7 can decrease cell surface expression of HLA-I, and E7 can downregulate expression of transporter associated with antigen processing (TAP) [37, 38]. Importantly, direct down regulation of MAGE-A3 expression may prove unlikely, as in melanoma patients treated in the therapeutic trials discussed above, MAGE-A3 expression was still present in the combined 25 patients who underwent subsequent resection of cutaneous metastasis [23, 29].
Vaccine induced antitumor immunity also competes with and may actually augment regulatory immune responses. For example, regulatory T cells (Tregs), which suppress effector T cells and mediate peripheral tolerance are increased in the blood and tumor microenvironment in SCCHN patients [39, 40]. Myeloid derived suppressor cells (MDSC), which also have been found to be increased in the SCCHN tumor microenvironment, are known to suppress the immune response through secretion of IL-10, increasing Tregs and decreasing T cell activation and migration [32, 41]. Our understanding of the role that each of these elements plays, alone and collectively in the regulation of antitumor vaccine-based immune responses, is hindered by the lack of post treatment tissue analysis, as findings in peripheral blood may not correlate with responses in the tumor microenvironment.
The second factor that likely contributes to the lack of observed efficacy was the patient cohort selected for study. The majority of the studied patient population had progressed through multiple lines of therapy and represents a population where advancement of disease is typically rapid. For example, progression-free survival with second-line chemotherapy in recurrent/metastatic SCCHN is 1–3 months [42, 43]. In this heavily pretreated population, the immune response to vaccination did not develop until weeks, and in some cases, months after the start of vaccine therapy—mitigating its potential efficacy in the face of actively progressing disease. For example, five patients (four in HPV 16 and one in MAGE-A3 cohort) progressed before they could even receive all four vaccinations.
The potential means to surmount these hurdles include combining the peptide-based vaccine with other immunotherapy agents known to inhibit death of antitumor effector T cells e.g., anti-B7-H1 or to mitigate the effects of cellular suppression e.g., Cytoxan [44, 45]. In addition, the delay between vaccination and development of the immune response suggests that the efficacy/utility of this regimen may best be determined in the adjuvant setting.
In conclusion, peptide immunomodulatory vaccines against HPV16 (GL-0810) and MAGE-A3 (GL-0817) in recurrent/metastatic SCCHN are well tolerated and stimulated potentially meaningful T cell and antibody responses in the majority of patients who completed all four vaccinations. In responding patients, T cell responses significantly correlated with antibody responses in both the HPV16 and MAGE-A3 cohorts—a finding with important biologic implications, which may also simplify monitoring of subsequent studies. While clinical efficacy was lacking in this refractory patient population, protocol development is underway to evaluate the efficacy of the MAGE-A3 immunomodulatory peptide vaccine in the adjuvant setting after definitive therapy in high-risk squamous cell carcinoma of the oral cavity.
Abbreviations
- B7H1:
-
B7 homolog 1
- CNS:
-
Central nervous system
- CR:
-
Complete response
- CTCAE:
-
Common toxicity criteria for adverse events
- DLT:
-
Dose-limiting toxicity
- ECOG:
-
Eastern Cooperative Oncology Group
- ELISA:
-
Enzyme-linked immunosorbent assay
- ELISPOT:
-
Enzyme-linked immunospot
- GM-CSF:
-
Granulocyte macrophage colony stimulating factor
- HIV:
-
Human immunodeficiency virus
- HLA:
-
Human leukocyte antigen
- HPV16:
-
Human papillomavirus 16
- IFN-γ:
-
Interferon gamma
- IL-10:
-
Interleukin 10
- MAGE:
-
Melanoma antigen E
- MDSC:
-
Myeloid derived suppressor cells
- ml:
-
Milliliter
- m2:
-
Meter squared
- MTD:
-
Maximum tolerated dose
- NSCLC:
-
Non-small cell lung cancer
- OS:
-
Overall survival
- PD:
-
Progressive disease
- PD-1:
-
Programmed death 1
- PD-L1:
-
Programmed death-ligand 1
- PET/CT:
-
Positron emission tomography–computed tomography
- PGE2:
-
Prostaglandin E2
- PR:
-
Partial response
- RECIST:
-
Response evaluation criteria in solid tumors
- R/M:
-
Recurrent/metastatic
- SCCHN:
-
Squamous cell carcinoma of the head and neck
- SD:
-
Stable disease
- TAP:
-
Transporter associated with antigen processing
- TGF-β:
-
Transforming growth factor beta
- Tregs:
-
Regulatory T cells
- UMGCC:
-
University of Maryland Greenebaum Cancer Center
- μg:
-
Microgram
References
Jemal A, Bray F, Center MM et al (2011) Global cancer statistics. CA Cancer J Clin 61:69–90. doi:10.3322/caac.20107
McDonald MW, Lawson J, Garg MK et al (2011) ACR appropriateness criteria retreatment of recurrent head and neck cancer after prior definitive radiation expert panel on radiation oncology-head and neck cancer. Int J Radiat Oncol Biol Phys 80:1292–1298. doi:10.1016/j.ijrobp.2011.02.014
Vermorken JB, Specenier P (2010) Optimal treatment for recurrent/metastatic head and neck cancer. Ann Oncol 21 Suppl 7: vii252–261. doi 10.1093/annonc/mdq453
Gillison ML, Koch WM, Capone RB et al (2000) Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst 92:709–720. doi:10.1093/jnci/92.9.709
Kreimer AR, Clifford GM, Boyle P, Franceschi S (2005) Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer Epidemiol Biomarkers Prev 14:467–475. doi:10.1007/s12105-010-0171-9
Munoz N, Bosch FX, de Sanjose S et al (2003) Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med 348:518–527. doi:10.1056/NEJMoa021641
Kenter GG, Welters MJ, Valentijn AR et al (2008) Phase I immunotherapeutic trial with long peptides spanning the E6 and E7 sequences of high-risk human papillomavirus 16 in end-stage cervical cancer patients shows low toxicity and robust immunogenicity. Clin Cancer Res 14:169–177. doi:10.1158/1078-0432.CCR-07-1881
Ressing ME, Sette A, Brandt RM et al (1995) Human CTL epitopes encoded by human papillomavirus type 16 E6 and E7 identified through in vivo and in vitro immunogenicity studies of HLA-A*0201-binding peptides. J Immunol 154:5934–5943
van der Burg SH, Ressing ME, Kwappenberg KM et al (2001) Natural T-helper immunity against human papillomavirus type 16 (HPV16) E7-derived peptide epitopes in patients with HPV16-positive cervical lesions: identification of 3 human leukocyte antigen class II-restricted epitopes. Int J Cancer 91:612–618. doi:10.1002/1097-0215
Cuffel C, Rivals JP, Zaugg Y et al (2011) Pattern and clinical significance of cancer-testis gene expression in head and neck squamous cell carcinoma. Int J Cancer 128:2625–2634. doi:10.1002/ijc.25607
Figueiredo DL, Mamede RC, Spagnoli GC et al (2011) High expression of cancer testis antigens MAGE-A, MAGE-C1/CT7, MAGE-C2/CT10, NY-ESO-1, and gage in advanced squamous cell carcinoma of the larynx. Head Neck 33:702–707. doi:10.1002/hed.21522
Jungbluth AA, Ely S, DiLiberto M et al (2005) The cancer-testis antigens CT7 (MAGE-C1) and MAGE-A3/6 are commonly expressed in multiple myeloma and correlate with plasma-cell proliferation. Blood 106:167–174. doi:10.1182/blood-2004-12-4931
Condomines M, Hose D, Raynaud P et al (2007) Cancer/testis genes in multiple myeloma: expression patterns and prognosis value determined by microarray analysis. J Immunol 178:3307–3315. doi:10.4049/jimmunol.178.5.3307
van der Bruggen P, Traversari C, Chomez P et al (1991) A gene encoding an antigen recognized by cytolytic T lymphocytes on a human melanoma. Science 254:1643–1647. doi:10.1126/science.1840703
Kobayashi H, Song Y, Hoon DS et al (2001) Tumor-reactive T helper lymphocytes recognize a promiscuous MAGE-A3 epitope presented by various major histocompatibility complex class II alleles. Cancer Res 61:4773–4778
Lu J, Wettstein PJ, Higashimoto Y et al (2001) TAP-independent presentation of CTL epitopes by Trojan antigens. J Immunol 166:7063–7071. doi:10.4049/jimmunol.166.12.7063
Lu J, Higashimoto Y, Appella E, Celis E (2004) Multiepitope Trojan antigen peptide vaccines for the induction of antitumor CTL and Th immune responses. J Immunol 172:4575–4582. doi:10.4049/jimmunol.172.7.4575
Voskens CJ, Sewell D, Hertzano R et al (2012) Induction of MAGE-A3 and HPV-16 immunity by Trojan vaccines in patients with head and neck carcinoma. Head Neck 34:1734–1746. doi:10.1002/hed.22004
Fruh K, Yang Y (1999) Antigen presentation by MHC class I and its regulation by interferon gamma. Curr Opin Immunol 11:76–81. doi:10.1016/S0952-7915(99)80014-4
Cheever MA, Chen W (1997) Therapy with cultured T cells: principles revisited. Immunol Rev 157:177–194. doi:10.1111/j.1600-065X.1997.tb00982.x
Gao FG, Khammanivong V, Liu WJ et al (2002) Antigen-specific CD4 + T-cell help is required to activate a memory CD8 + T cell to a fully functional tumor killer cell. Cancer Res 62:6438–6441
Voskens CJ, Strome SE, Sewell DA (2009) Synthetic peptide-based cancer vaccines: lessons learned and hurdles to overcome. Curr Mol Med 9:683–693
Pichichero ME (2008) Improving vaccine delivery using novel adjuvant systems. Hum Vaccin 4:262–270. doi:10.4161/hv.4.4.5742
Kreimer AR, Johansson M, Waterboer T et al (2013) Evaluation of human papillomavirus antibodies and risk of subsequent head and neck cancer. J Clin Oncol 31:2708–2715. doi:10.1200/JCO.2012.47.2738
Kruit WH, van Ojik HH, Brichard VG et al (2005) Phase 1/2 study of subcutaneous and intradermal immunization with a recombinant MAGE-3 protein in patients with detectable metastatic melanoma. Int J Cancer 117:596–604. doi:10.1002/ijc.21264
Klebanoff CA, Acquavella N, Yu Z, Restifo NP (2011) Therapeutic cancer vaccines: are we there yet? Immunol Rev 239:27–44. doi:10.1111/j.1600-065X.2010.00979.x
Atanackovic D, Altorki NK, Stockert E et al (2004) Vaccine-induced CD4 + T cell responses to MAGE-3 protein in lung cancer patients. J Immunol 172:3289–3296. doi:10.4049/jimmunol.172.5.3289
Vansteenkiste J, Zielinski M, Linder A et al (2013) Adjuvant MAGE-A3 immunotherapy in resected non-small-cell lung cancer: phase II randomized study results. J Clin Oncol 31:2396–2403. doi:10.1200/JCO.2012.43.7103
Marchand M, Punt CJ, Aamdal S et al (2003) Immunisation of metastatic cancer patients with MAGE-3 protein combined with adjuvant SBAS-2: a clinical report. Eur J Cancer 39:70–77. doi:10.1016/S0959-8049(02)00479-3
Kruit WH, Suciu S, Dreno B et al (2013) Selection of immunostimulant AS15 for active immunization with MAGE-A3 protein: results of a randomized phase II study of the European Organisation for Research and Treatment of Cancer Melanoma Group in Metastatic Melanoma. J Clin Oncol 31:2413–2420. doi:10.1200/JCO.2012.43.7111
Brinkman JA, Hughes SH, Stone P et al (2007) Therapeutic vaccination for HPV induced cervical cancers. Dis Markers 23:337–352. doi:10.1155/2007/245146
Allen CT, Judd NP, Bui JD, Uppaluri R (2012) The clinical implications of antitumor immunity in head and neck cancer. Laryngoscope 122:144–157. doi:10.1002/lary.21913
Young MR (2006) Protective mechanisms of head and neck squamous cell carcinomas from immune assault. Head Neck 28:462–470. doi:10.1002/hed.20331
Lyford-Pike S, Peng S, Young GD et al (2013) Evidence for a role of the PD-1: PD-L1 pathway in immune resistance of HPV-associated head and neck squamous cell carcinoma. Cancer Res 73:1733–1741. doi:10.1158/0008-5472.CAN-12-2384
Strome SE, Dong H, Tamura H et al (2003) B7-H1 blockade augments adoptive T-cell immunotherapy for squamous cell carcinoma. Cancer Res 63:6501–6505
Ukpo OC, Thorstad WL, Lewis JS Jr (2012) B7-H1 expression model for immune evasion in human papillomavirus-related oropharyngeal squamous cell carcinoma. Head Neck Pathol 7:113–121. doi:10.1007/s12105-012-0406-z
Li W, Deng XM, Wang CX et al (2010) Down-regulation of HLA class I antigen in human papillomavirus type 16 E7 expressing HaCaT cells: correlate with TAP-1 expression. Int J Gynecol Cancer 20:227–232. doi:10.1111/IGC.0b013e3181cceec5
Campo MS, Graham SV, Cortese MS et al (2010) HPV-16 E5 down-regulates expression of surface HLA class I and reduces recognition by CD8 T cells. Virology 407:137–142. doi:10.1016/j.virol.2010.07.044
Schott AK, Pries R, Wollenberg B (2010) Permanent up-regulation of regulatory T-lymphocytes in patients with head and neck cancer. Int J Mol Med 26:67–75. doi:10.3892/ijmm_00000436
Strauss L, Bergmann C, Szczepanski M et al (2007) A unique subset of CD4 + CD25highFoxp3 + T cells secreting interleukin-10 and transforming growth factor-beta1 mediates suppression in the tumor microenvironment. Clin Cancer Res 13:4345–4354. doi:10.1158/1078-0432.CCR-07-0472
Ostrand-Rosenberg S, Sinha P, Beury DW, Clements VK (2012) Cross-talk between myeloid-derived suppressor cells (MDSC), macrophages, and dendritic cells enhances tumor-induced immune suppression. Semin Cancer Biol 22:275–281. doi:10.1016/j.semcancer.2012.01.011
Herbst RS, Arquette M, Shin DM et al (2005) Phase II multicenter study of the epidermal growth factor receptor antibody cetuximab and cisplatin for recurrent and refractory squamous cell carcinoma of the head and neck. J Clin Oncol 23:5578–5587. doi:10.1200/JCO.2005.07.120
Zenda S, Onozawa Y, Boku N et al (2007) Single-agent docetaxel in patients with platinum-refractory metastatic or recurrent squamous cell carcinoma of the head and neck (SCCHN). Jpn J Clin Oncol 37:477–481. doi:10.1093/jjco/hym059
Le DT, Jaffee EM (2012) Regulatory T-cell modulation using cyclophosphamide in vaccine approaches: a current perspective. Cancer Res 72:3439–3444. doi:10.1158/0008-5472.CAN-11-3912
Lutsiak ME, Semnani RT, De Pascalis R et al (2005) Inhibition of CD4(+)25 + T regulatory cell function implicated in enhanced immune response by low-dose cyclophosphamide. Blood 105:2862–2868. doi:10.1182/blood-2004-06-2410
Conflict of interest
Dr. Strome is a co-founder and stockholder of Gliknik Inc., a biotechnology company and licensee of the Trojan Peptide Vaccines. Dr. Strome also receives royalties from the Mayo Clinic College of Medicine for intellectual property related to B7-H1 (PD-L1). All other authors have no disclosures.
Author information
Authors and Affiliations
Corresponding author
Additional information
Scott E. Strome and Martin J. Edelman have share senior authorship.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zandberg, D.P., Rollins, S., Goloubeva, O. et al. A phase I dose escalation trial of MAGE-A3- and HPV16-specific peptide immunomodulatory vaccines in patients with recurrent/metastatic (RM) squamous cell carcinoma of the head and neck (SCCHN). Cancer Immunol Immunother 64, 367–379 (2015). https://doi.org/10.1007/s00262-014-1640-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-014-1640-x