Abstract
The association between the CD8+ T-cell responses to human papillomavirus type 16 (HPV-16) E6 protein and a favorable clinical trend has been demonstrated previously. The roles of human papillomavirus (HPV)-specific CD4+ T-cell responses and of regulatory T-cells (Tregs) were examined. Subjects with a recent history of abnormal Papanicolaou smear were eligible, and colposcopy-guided biopsy was performed at enrollment. Interferon-γ enzyme-linked immunospot assay and fluorescent-activated cell sorter analysis to measure the frequencies of Tregs were performed. Subjects with histological diagnoses of cervical intraepithelial neoplasia 1, 2, or 3 were considered to have short-term persistence of cervical abnormality and were called “persistors” (n = 51) while those of normal histology were designated to be “regressors” (n = 33). A significantly higher percentage CD4+ T-cell response was detected in the regressors (15/33 or 45.5%) compared with the persistors (10/51 or 19.6%) (P = .015) for the E6 peptides but not for the E7 peptides. The CD4+ responses to certain E6 regions [E6(16–40), E6(91–115), E6(106–130), and E6(136–158)] were also significantly higher in the regressors. Although there was no difference in the frequencies of Tregs between the two groups, low frequencies of Tregs were significantly associated with positive CD4+ T-cell responses within certain E6 regions [E6(16–40), E6(31–55), E6(76–100), E6(91–115), and E6(106–130)]. The CD4+ and CD8+ T-cell responses to the HPV-16 E6 protein are associated with a favorable clinical trend. The HPV-16 E6 protein should be incorporated in the design of an HPV therapeutic vaccine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is the second most common cancer in women worldwide and accounts for almost 12% of all cancers in women [1]. Globally, it is estimated that cervical cancer affects approximately 500,000 women each year, of whom, 80% live in developing countries [2]. In the United States, approximately 12,200 women are diagnosed with invasive cervical cancer and about 4,210 deaths from the disease are reported each year [3]. There is clear a molecular epidemiologic evidence that links human papillomavirus (HPV) to invasive cervical cancer [4, 5], and HPV is found in 99.7% of cervical cancer cases [5].
The lifetime risk of acquiring high-risk HPV is 50% and that of developing precursor lesions of cervical cancer requiring treatment is 10% [6]. Precursor lesions are abnormal growths of squamous cells of the cervix and are graded as either low-grade squamous intraepithelial lesions [LSILs or cervical intraepithelial neoplasia 1 (CIN1)] or high-grade squamous intraepithelial lesions [HSILs or cervical intraepithelial neoplasia 2 (CIN2)–cervical intraepithelial neoplasia 3 (CIN3)]. Most LSILs regress spontaneously, and therefore, patients with LSILs are observed closely [7, 8]. However, some LSILs do progress to HSILs. As LSILs progress to HSILs, viral DNA integration takes place and initiates transformation events mediated by two oncogenic proteins: E6 and E7 [9]. Approximately two-thirds of HSILs are expected to persist, and the likelihood of untreated HSILs, particularly CIN 3, progressing to invasive cancer is greater than 12% [9–11]. Women with HSILs are therefore typically treated with loop electrosurgical excision procedure.
Cell-mediated immune responses involving CD4+ and CD8+ T-cells are thought to be responsible for eradicating established HPV infections resulting in spontaneous regression of approximately 50–90% of CIN 1, 40% of CIN 2, and 30% of CIN 3 [9, 12, 13]. Specifically, immune responses against E6 and E7 may play a role in modulating HPV infection and HPV-associated disease [14]. Cytotoxic CD8+ T-cell responses to human papillomavirus type 16 (HPV-16) E6 or E7 protein have been detected in HPV-16-positive women without CIN lesions more commonly than in HPV-16-positive women with CIN, suggesting that CD8+ T cells have a protective role against disease [15]. Moreover, CD8+ T-cell responses to the HPV-16 E6 protein, but not the E7 protein, have been shown to be significantly associated with viral clearance of HPV-16 in women with no evidence of squamous intraepithelial lesion (SIL) [16]. In our most recent work, we evaluated women with cervical abnormalities and demonstrated that a favorable clinical outcome is significantly associated with CD8+ T-cell responses to HPV-16 E6 protein, but not E7 protein [17]. Surprisingly, these responses were detected not only in women with HPV-16 infection, but also in women with other high-risk HPV types, raising a possibility that these responses may be cross-reactive among high-risk HPV types. Regulatory T cells (Tregs), well known for their role in the modulation of immune responses, have also been shown to influence HPV pathogenesis [18, 19]. The goals of the current study were to examine the roles of CD4+ T-cell responses to the HPV-16 E6 and E7 proteins and of Tregs in the outcomes of subjects being studied for abnormal Papanicolaou (Pap) smear results.
Materials and methods
Study design and subjects
The study protocol was approved by the institutional review board of the University of Arkansas for Medical Sciences (UAMS). Patients were recruited from the Obstetrics and Gynecology clinics at UAMS. Informed consent was obtained from all participants. Eighty-eight patients were enrolled for having a recent history of abnormal Pap test results which had not been treated. Colposcopy-guided biopsy was performed at the enrollment visit. The exclusion criteria were pregnancy, immunodeficiency, and inability to give consent. On the day of enrollment, cervical cytology specimens were collected in a ThinPrep® liquid PAP vial (Cytyc Corp., Boxborough, MA) for HPV-DNA testing. In addition, 60 ml of heparinized whole blood was collected to perform interferon-γ (IFN-γ) enzyme-linked immunospot (ELISPOT) assay, and fluorescence-activated cell sorting (FACS) analysis of Tregs. Subjects were classified as “regressors” (n = 33) if the histologic evaluation on the day of enrollment showed negative results, or as “persistors” (n = 51) of short-term cervical abnormalities if the histologic diagnosis was CIN 1, 2, or 3. Other subjects who did not meet the criteria for either group due to inadequate sample collection or equivocal diagnosis were classified as “indeterminates” (n = 4).
HPV-DNA testing
HPV-DNA testing was performed using the Linear Array HPV Genotyping Test (Roche Diagnostics, Indianapolis, IN) according to manufacturer’s instructions. This test detects 37 anogenital HPV types: 6, 11, 16, 18, 26, 31, 33, 35, 39, 40, 42, 45, 51, 52, 53, 54, 55, 56, 58, 59, 61, 62, 64, 66, 67, 68, 69, 70, 71, 72, 73 [MM9], 81, 82 [MM4], 83 [MM7], 84 [MM8], IS39, and CP6108. The human β-globin signal was also assayed as a positive control for sample adequacy of DNA content. Subjects were categorized for being positive for HPV-16, HPV-16-related types (16, 31, 33, 35, 52, 58, and 67) [20], and/or high-risk HPV types (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, and 82) [21].
Establishing CD4+ T-cell lines
An in vitro stimulation protocol previously developed for establishing CD8+ T-cell lines was modified [22]. Peripheral blood mononuclear cells (PBMC) were isolated from heparinized whole blood. CD14+ monocytes were magnetically selected from PBMC using a commercially available kit (CD14 MicroBeads, Miltenyi Biotec, Auburn, CA). CD14+ monocytes, CD14-depleted PBMC, and PBMC (for Treg analyses) were cryopreserved. Autologous immature dendritic cells (DCs) were established by growing thawed monocytes in the presence of granulocyte–macrophage colony-stimulating factor (50 ng/ml) and recombinant interleukin-4 (100 U/ml) for 5 days. They were matured by 48-h culture in wells containing irradiated mouse L cells expressing CD40 ligands and containing exogenous E6-GST and E7-GST proteins (5 μg/ml each) [15]. CD4+ T cells were selected from thawed CD14-depleted PBMC using a commercially available magnetic kit (CD4 T-cell Isolation Kit, Miltenyi Biotec). CD4+ T-cell lines were established by combining the CD4+ T cells with the autologous mature DCs pulsed with the recombinant E6-GST and E7-GST proteins. After 7 days, another round of in vitro stimulation was repeated for additional 7 days.
IFN-γ ELISPOT assay
IFN-γ ELISPOT assay was performed as previously described [22]. Each peptide pool or region contained three 15-mer peptides overlapping by 10 central amino acids; for example, pool E6(1–25) contained 15-mer peptides E6(1–15), E6 (6–20), and E6 (11–25). The following were the regions covered by the E6 and E7 peptide pools: E6(1–25), E6(16–40), E6(31–55), E6(46–70), E6(61–85), E6(76–100), E6(91–115), E6(106–130), E6(121–145), E6(136–158), E7(1–25), E7(16–40), E7(31–55), E7(46–70), E7(61–85), and E7(76–98). Spot-forming units (SFUs) formed by IFN-γ-secreting cells were counted with an automated ELISPOT analyzer (Cell Technology Inc., Jessup, MD). Immune response was expressed as the ratio of the averaged number of SFUs in peptide wells divided by the averaged number of SFUs in no-peptide medium wells. A peptide region was considered to be positive if the ratio was equal to or greater than 2 [23].
Treg staining and analysis
Thawed PBMC were stained with relevant isotype controls and the following monoclonal antibodies: fluorescein isothiocyanate-labeled anti-human CD4 (clone RPA-T4), PerCP-Cy5.5-labeled anti-human CD25 (clone BC96), allophycocyanin-labeled anti-human Foxp3 (clone PCH101), and phycoerythrin-labeled anti-human CTLA-4 (clone 14D3). All of the antibodies were purchased from eBiosciences (San Diego, CA). PBMC were first stained with antibodies for surface markers CD4 and CD25. Intracellular Foxp3 and CTLA-4 staining was performed using the Foxp3 staining kit according to the manufacturer’s instructions (eBiosciences). Flow cytometric analysis was performed with a FACSCalibur using a CellQuest software (Becton–Dickinson Biosciences, San Jose, CA). Ten thousand events were analyzed per sample. Tregs were defined as CD4+CD25+Foxp3+ or CD4+CD25+Foxp3+CTLA-4+, and the frequency was expressed as a percentage of CD4+CD25+Foxp3+/CD4+ or CD4+CD25+Foxp3+CTLA-4+/CD4+.
Statistical analysis
Comparisons of demographic characteristics between the regressors and the persistors were made by the Wilcoxon rank-sum test on age, Fisher’s exact test on race and ethnicity, and Kruskal–Wallis test on the median number of days between the prior Pap test cytological diagnosis visit and the histologic diagnosis visit (enrollment visit). A comparison of any positive immune responses to HPV-16 E6 protein or E7 protein between the regressors and the persistors was conducted using the Fisher’s exact test in order to determine whether the CD4+ T-cell immune responses were associated with a favorable clinical outcome. The comparisons were repeated for subgroups of subjects based on the HPV-DNA results, i.e., high-risk HPV positive, HPV-16-related positive, and HPV-16 positive. Further comparisons were made for each of the regions covered by the E6 or E7 peptide pools. The relationship between the numbers of positive E6 or E7 regions and clinical trend was also evaluated using the Fisher’s exact test. To examine whether the positive CD4+ T-cell responses to HPV-16 E6 or E7 peptides may be attributed to cross-reactivity to other HPV types, HPV-16 infected subjects were removed in the analysis of CD4+ T-cell responses (non-HPV-16-positive subjects). In the non-HPV-16-positive group, a comparison of positive E6 or E7 CD4+ T-cell responses between the regressors and the persistors was conducted using the Fisher’s exact test.
With regard to frequencies of circulating Tregs, the regressors and the persistors were compared using the unpaired two-tailed Student’s t test. The comparisons were repeated for subgroups of subjects based on the HPV-DNA typing results. Furthermore, comparisons of mean Treg frequencies between those subjects with positive immune responses (E6 overall, each of the E6 regions, E7 overall, or each of the E7 regions) and those subjects with negative immune response to E6 overall or E7 overall were made using the unpaired two-tailed Student’s t test.
An analogous study, examining the CD8+ T-cell responses to HPV-16 E6 and E7 peptides in the same patient population, has been described [17]. Comparisons between CD4+ and CD8+ T-cell responses were made among regressors or persistors who were evaluated using Pap test prior to the enrollment and using biopsy on the day of enrollment. The Fisher’s exact test was performed. Significance was determined as P < 0.05. All of the analyses were performed with SAS 9.2 (SAS Institute Inc., Cary, NC).
Results
Patient characteristics
A summary of demographic characteristics of the regressors and the persistors is shown in Table 1. There were no significant differences for all characteristics including the median number of days between the prior Pap test cytological diagnosis (“previous” visit) and the histologic diagnosis (“enrollment” visit), which was 84 days [interquartile range (IQR) 60–119 days] for the regressors and 64 days (IQR 50–119 days) for the persistors.
HPV-DNA typing
HPV-DNA typing was performed on ThinPrep specimens collected on the day of enrollment from all 88 subjects. One sample had inadequate DNA for typing. Overall, at least 1 type of HPV-DNA was detected in 83 (95.4%) of 87 subjects. HPV-16 was the most commonly detected type (n = 22, 25.3%) followed by HPV-39 (n = 17, 19.5%), HPV-54 (n = 15, 17.2%), HPV-51 (n = 14, 16.1%), and HPV-35 (n = 13, 14.9%). In regard to the number of HPV types detected, 28 (32.2%) of 87 subjects had a single detectable HPV type; 2 HPV types were detected in 14 (16.1%) subjects; 3 HPV types in 14 (16.1%) subjects; and 4 or more types in 27 (31.0%) subjects. Fifty subjects (57.5%) were positive for at least 1 HPV-16-related types and 72 (82.8%) for high-risk HPV types.
CD4+ T-cell responses to HPV-16 E6 and E7
The CD4+ T-cell responses to HPV-16 E6 peptides were significantly higher in the regressors (15/33 or 45.5%) compared with the persistors (10/51 or 19.6%) (P = .015). Although the percentage in the CD4+ T-cell responses to HPV-16 E7 antigens was also higher in the regressor group (5/33 or 15.2%) compared with the persistor group (3/51 or 5.9%), the difference was not statistically significant (P = .25). Additional comparisons were made for subgroups of subjects based on HPV-DNA detected (Table 2).
Further comparisons were made for each of the ten E6 regions or six E7 regions. The comparisons reached statistical significance for the following regions between the regressors and the persistors: E6(16–40) (24% vs. 2%, P = .0020), E6(31–55) (21% vs. 6%, P = .044), E6(61–85) (12% vs. 0%, P = .021), and E6(91–115) (18% vs. 2%, P = .013). Among the subjects who were high-risk HPV-positive, the comparisons reached statistical significance for the following regions: E6(1–25) (18% vs. 2%, P = .035), E6(16–40) (23% vs. 2%, P = .012), E6(61–85) (14% vs. 0%, P = .031), E6(91–115) (23% vs. 2%, P = .012), E6(106–130) (27% vs. 4%, P = .012), and E6(136–158) (18% vs. 2%, P = .035). Among subjects who were positive for HPV-16 related types, the comparisons were significant for E6(1–25) (17% vs. 0%, P = .047), E6(16–40) (22% vs. 0%, P = .016), E6(61–85) (17% vs. 0%, P = .047), E6(91–115) (22% vs. 0%, P = .016), E6(106–130) (28% vs. 3%, P = .023), and E6 (136–158) (17% vs. 0%, P = .047). No comparisons were significant among the HPV-16 positive subjects.
Overall, 27 (32.1%) of 84 subjects demonstrated at least 1 positive peptide region within E6 and/or E7. Fourteen subjects (16.7%) were positive for 1 region; 3 subjects (3.6%) for 2 regions; 2 subjects (2.4%) for 3 regions; 3 subjects (3.6%) for 4 regions; 1 subject (1.2%) for 6 regions; 1 subject (1.2%) for 7 regions; 1 subject (1.2%) for 8 regions; 1 subject (1.2%) for 10 regions; and 1 subject (1.2%) for 12 regions. Additionally, the numbers of positive peptide regions within E6 or E7 were compared, and the regressors were more likely to have 2 or more E6-positive (P = .0035) or E7-positive (P = .042) peptide regions as compared with the persistors (Table 3).
To examine whether the positive CD4+ T-cell responses to HPV-16 E6 and E7 peptides may be attributed to cross-reactivity to other HPV types, HPV-16 infected subjects were removed in the analysis of CD4+ T-cell responses (non-HPV-16-positive subjects). Overall, positive CD4+ T-cell responses were detected against the HPV-16 E6 protein (20/63 or 31.7%) or the E7 protein (7/63 or 11.1%) in subjects without detectable HPV-16 infection. When the results were evaluated based on clinical trends, the CD4+ T-cell responses to the HPV-16 E6 peptides were detected in 12 of 23 regressors and 8 of 40 persistors (52.2% vs. 20.0%, P = .012). The responses to the HPV-16 E7 peptides were positive in 5 of 23 regressors and 2 of 40 persistors (21.7% vs. 5.0%, P = .089).
Frequencies of circulating Tregs
The frequencies of CD4+CD25+Foxp3+ or CD4+CD25+Foxp3+CTLA-4+ Tregs were analyzed in PBMC samples available from 75 subjects. The mean percentage of CD4+CD25+Foxp3+ Tregs was 3.01% (standard error of the mean [SEM] 0.21%) for the regressors (n = 30) and 2.96% (SEM 0.15%) for the persistors (n = 45, P = .86) (Table 4A). The results comparing the mean percentages of CD4+CD25+Foxp3+CTLA-4+ Tregs were similar (P = .83) (Table 4B). Additional comparisons in subgroups of subjects based on HPV status did not reveal any significant differences.
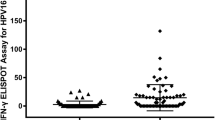
Whether the CD4+ T-cell immune responses against E6 or E7 peptides are associated with the low frequencies of circulating Tregs was examined. Mean percentage of CD4+CD25+Foxp3+ Tregs among subjects with positive CD4+ T-cell responses to E6 overall or to each of the E6 regions were compared with the Treg percentage in subjects with no E6 response (Fig. 1a). Significant associations were found for E6(16–40), E6(31–55), E6(76–100), E6(91–115), and E6(106–130) regions. In high-risk HPV-positive subjects, mean percentage of Tregs was significantly lower in subjects with positive responses to E6 overall (P = .0016) and to multiple E6 regions (Fig. 1b). In HPV-16-related-positive subjects, mean percentage of Tregs was significantly lower in subjects with positive responses to E6 overall (P = .024) and the E6(76–100) region (P = .023) (data not shown). In HPV-16-positive patients, no E6 region was significant (data not shown). No significant comparisons were found for any of the analyses for E7 (data not shown). The results were similar when mean percentages of CD4+CD25+Foxp3+CTLA-4+ were examined (data not shown).
a Comparison of the mean CD4+CD25+Foxp3+ Treg frequencies of patients (n = 75) with positive CD4+ T-cell responses to HPV-16 E6 or to different regions within E6 to those with no E6 response. b Comparison of the mean CD4+CD25+Foxp3+ Treg frequencies of high-risk HPV-positive patients (n = 60) with positive CD4+ T-cell responses to HPV-16 E6 or to different regions within E6 with those with no E6 response. *Significance was determined as P < 0.05. The bars represent the SEM
Comparisons of CD4+ and CD8+ T-cell immune responses
Previously, we used the same sets of HPV-16 E6 and E7 peptides to assess CD8+ T-cell responses in subjects who were recruited from the same clinics [17]. Comparisons between the CD4+ and CD8+ responses among the regressors or persistors (Fig. 2) revealed no significant difference except for the HPV-16 E7(46–70) region. Among the persistors, 3 of 21 subjects (14%) demonstrated CD8+ response to this region while none of 51 (0%) demonstrated CD4+ responses (P = .028).
Discussion
Our group has previously demonstrated that the CD8+ T-cell immune responses against the HPV-16 E6 protein but not the E7 protein were significantly associated with a favorable clinical trend in subjects being followed for cervical abnormalities [17]. The goals of the current study were to examine the roles of the CD4+ T-cell immune responses and the Tregs in the outcomes of the patients from the same clinics. For the CD4+ T-cell responses, not only were the responses to E6 overall (Table 2) associated with a favorable clinical outcome, but also to a number of regions within the E6 protein. Furthermore, the regressors were more likely to have 2 or more E6-positive or E7-positive peptide regions as compared with the persistors (P = .0035 or P = .042, respectively) (Table 3).
Other studies have also examined cell-mediated immunity against HPV-16 E6 and E7 antigens but did not reach the same conclusions. A study by Kadish et al. [24] evaluated cell-mediated immune response to HPV-16 E6 and E7 peptides in women with biopsy-confirmed CIN 1 and 2. Positive lymphoproliferative responses to E7(37–54) peptide were significantly associated with regression of cervical disease and viral clearance; however, they did not find a significant association between proliferative responses to the E6 peptides. Possible reasons for the different conclusions reached by us and by Kadish et al. include the different methods used for measuring the T-cell responses to HPV-16 E6 and E7 antigens, and the different manners by which the subjects were characterized. A study by Steele et al. [25] observed a high percentage (78%) of T-cell responses against HPV-16 antigens (E6, E7, E4, L1, and L2) in women with a spectrum of cervical diseases. In particular, CD8+ T-cell responses to the E6 peptides were frequently detected across all disease levels including cervical carcinoma. Therefore, the authors concluded that the E6-specific CD8+ T cells were not important in disease clearance. On the other hand, the overall CD4+ T-cell responses were less frequent among those with progressive disease, namely CIN 1, CIN 2, and CIN 3, possibly indicating the association between the lack of CD4+ T-cell response and disease progression. They concluded that the CD4+ T cells were important in controlling cervical disease. This was a cross-sectional study, and the subjects’ clinical status was not evaluated over time. Therefore, it is difficult to make a comparison with our study. Trimble et al. [26] reported that HPV-16 E6- and E7-specific responses measured in the peripheral blood by IFN-γ ELISPOT assay were detectable but did not correlate with spontaneous regression of lesions in patients with HPV-16 infection and CIN2/3 disease. This was in spite of the fact that one in four HPV-16+ CIN2/3 lesions underwent complete histologic regression within a 15-week period. Their in vitro stimulation protocol that involved incubating PBMC with HPV peptides and recombinant interleukin-2 for 9 days may not have been robust enough to expand sufficient numbers of memory HPV-specific T cells.
To determine whether the positive CD4+ T-cell responses to HPV-16 E6 or E7 peptides may be attributed to cross-reactivity to other HPV types, HPV-16 infected subjects were removed from the analysis of all subjects. In this non-HPV-16-positive group, positive CD4+ T-cell responses were detected against both HPV-16 E6 and E7. Moreover, a favorable clinical outcome remained significantly associated with positive responses to regions within the HPV-16 E6 protein. Since the sequences of these peptides were based on HPV-16, positive responses detected in the subjects with non-HPV-16 HPV types may be due either to memory HPV-16 E6-specific T cells from previous HPV-16 infection or to cross-recognition of HPV-16 E6 peptides by CD4+ T-cell-specific for homologous peptides of other HPV types. Kadish et al. [24] reported a similar finding in that they detected proliferative responses to HPV-16 E7(37–54) peptide in subjects infected with types other than HPV-16. We have previously demonstrated examples of cross-recognition of homologous E6 antigens of high-risk HPV types (HPV-35, -39, -45, -51, and -73) by a CD8+ T-cell clone specific for the HPV-16 E6(52–61) epitope [27].
In this study, we did not find correlations between the low frequencies of Tregs and the favorable clinical trend. However, significant correlations were uncovered between the low frequencies of Tregs and the CD4+ T-cell responses. The lack of association between the frequencies of Tregs and clinical trend could be due to the fact that Tregs are not directly responsible for the progression of lesions, but they are one of several contributors to the clinical outcome. Tregs contribute by suppressing and modulating other key immune cells, such as effector T-cells that are thought to be directly involved in the elimination of lesions. Therefore, the correlations between the low frequencies of Tregs with HPV-16 E6-specific CD4+ T-cell responses may have been more easily demonstrated than the correlation between the low frequencies of Tregs with clinical outcome. Interestingly, a significant association between HPV-specific Tregs and HPV-specific T-cell proliferative responses has been reported in a study of cervical cancer patients, but the authors did not report associations between Treg levels and clinical outcomes [28].
The prevalence of Tregs in circulation and in the tumor microenvironment of cancer subjects has been implicated in worse disease outcome. It is thought that cancers are associated with recruitment and expansion of Tregs that suppress tumor-specific immune responses [29]. In this study, we investigated whether lower frequencies of Tregs in the peripheral blood of patients with pre-malignant cervical disease are associated with favorable disease outcome. The limitation of our study was that we evaluated Treg frequency by sampling circulating Tregs in the peripheral blood, which is an indirect measurement of Tregs in the cervical lesion microenvironment.
The comparisons of CD4+ and CD8+ T-cell responses did not reveal significant differences among the regressors or persistors except in the E7(47–70) region among the persistors. To our knowledge, this is the first side by side comparisons of immune responses to regions within the HPV-16 E6 and E7 proteins. While performing both CD4+ and CD8+ analyses on the same individuals would have been preferable, which would not have been feasible since 60 ml of whole blood is required for each analysis. Given that the E7 protein overall is much less immunogenic than the E6 protein, the significance of more frequent CD8+ T-cell responses to the E7(47–70) region among persistors is unclear.
In summary, we have demonstrated that the CD4+ T-cell immune responses to HPV-16 E6 antigens, but not to E7 antigens, are significantly associated with a favorable clinical trend. In addition, CD4+ T-cell responses to specific regions within the HPV-16 E6 protein were significantly associated with a favorable outcome. Also, significantly lower percentages of circulating Tregs were detected in subjects with positive CD4+ T-cell immune responses against a number of E6 regions compared with subjects with no E6 response. Our results suggest that the CD4+ and CD8+ T-cell responses to the HPV-16 E6 antigens are associated with a favorable clinical trend and that they should be incorporated into a therapeutic vaccine for prevention of cervical cancer.
References
Pisani P, Bray F, Parkin DM (2002) Estimates of the world-wide prevalence of cancer for 25 sites in the adult population. Int J Cancer 97(1):72–81. doi:10.1002/ijc.1571
Cutts FT, Franceschi S, Goldie S, Castellsague X, de Sanjose S, Garnett G, Edmunds WJ, Claeys P, Goldenthal KL, Harper DM, Markowitz L (2007) Human papillomavirus and HPV vaccines: a review. Bull World Health Organ 85(9):719–726. doi:S0042-96862007000900018
Cancer Facts & Figures (2010) American Cancer Society
Bosch FX, Lorincz A, Munoz N, Meijer CJ, Shah KV (2002) The causal relation between human papillomavirus and cervical cancer. J Clin Pathol 55(4):244–265
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Munoz N (1999) Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 189(1):12–19. doi:10.1002/(SICI)1096-9896(199909)189:1<12:AID-PATH431>3.0.CO;2-F
Crum C (ed) (2004) Robbins & cotran pathologic basis of disease. 7th edn, W.B. Saunders Co., Philadelphia
Koutsky LA, Holmes KK, Critchlow CW, Stevens CE, Paavonen J, Beckmann AM, DeRouen TA, Galloway DA, Vernon D, Kiviat NB (1992) A cohort study of the risk of cervical intraepithelial neoplasia grade 2 or 3 in relation to papillomavirus infection. N Engl J Med 327(18):1272–1278. doi:10.1056/NEJM199210293271804
Richart RM, Barron BA (1969) A follow-up study of patients with cervical dysplasia. Am J Obstet Gynecol 105(3):386–393. doi:0002-9378(69)90268-3
Ostor AG (1993) Natural history of cervical intraepithelial neoplasia: a critical review. Int J Gynecol Pathol 12(2):186–192
Nash JD, Burke TW, Hoskins WJ (1987) Biologic course of cervical human papillomavirus infection. Obstet Gynecol 69(2):160–162
Campion MJ, McCance DJ, Cuzick J, Singer A (1986) Progressive potential of mild cervical atypia: prospective cytological, colposcopic, and virological study. Lancet 2(8501):237–240. doi:S0140-6736(86)92067-2
Melnikow J, Nuovo J, Willan AR, Chan BK, Howell LP (1998) Natural history of cervical squamous intraepithelial lesions: a meta-analysis. Obstet Gynecol 92(4 Pt 2):727–735
Moscicki AB, Shiboski S, Hills NK, Powell KJ, Jay N, Hanson EN, Miller S, Canjura-Clayton KL, Farhat S, Broering JM, Darragh TM (2004) Regression of low-grade squamous intra-epithelial lesions in young women. Lancet 364(9446):1678–1683. doi:10.1016/S0140-6736(04)17354-6
Moscicki AB, Schiffman M, Kjaer S, Villa LL (2006) Chapter 5: Updating the natural history of HPV and anogenital cancer. Vaccine 24(suppl 3):S3/42–S3/51. doi:10.1016/j.vaccine.2006.06.018
Nakagawa M, Stites DP, Farhat S, Sisler JR, Moss B, Kong F, Moscicki AB, Palefsky JM (1997) Cytotoxic T lymphocyte responses to E6 and E7 proteins of human papillomavirus type 16: relationship to cervical intraepithelial neoplasia. J Infect Dis 175(4):927–931
Nakagawa M, Stites DP, Patel S, Farhat S, Scott M, Hills NK, Palefsky JM, Moscicki AB (2000) Persistence of human papillomavirus type 16 infection is associated with lack of cytotoxic T lymphocyte response to the E6 antigens. J Infect Dis 182(2):595–598. doi:10.1086/315706
Nakagawa M, Gupta SK, Coleman HN, Sellers MA, Banken JA, Greenfield WW (2010) A favorable clinical trend is associated with CD8 T-cell immune responses to the human papillomavirus type 16 e6 antigens in women being studied for abnormal pap smear results. J Low Genit Tract Dis 14(2):124–129. doi:10.1097/LGT.0b013e3181c6f01e
Molling JW, de Gruijl TD, Glim J, Moreno M, Rozendaal L, Meijer CJ, van den Eertwegh AJ, Scheper RJ, von Blomberg ME, Bontkes HJ (2007) CD4(+)CD25hi regulatory T-cell frequency correlates with persistence of human papillomavirus type 16 and T helper cell responses in patients with cervical intraepithelial neoplasia. Int J Cancer 121(8):1749–1755. doi:10.1002/ijc.22894
van der Burg SH, Piersma SJ, de Jong A, van der Hulst JM, Kwappenberg KM, van den Hende M, Welters MJ, Van Rood JJ, Fleuren GJ, Melief CJ, Kenter GG, Offringa R (2007) Association of cervical cancer with the presence of CD4+ regulatory T cells specific for human papillomavirus antigens. Proc Natl Acad Sci USA 104(29):12087–12092. doi:10.1073/pnas.0704672104
de Villiers EM, Fauquet C, Broker TR, Bernard HU, zur Hausen H (2004) Classification of papillomaviruses. Virology 324(1):17–27. doi:10.1016/j.virol.2004.03.033
Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV, Snijders PJ, Meijer CJ (2003) Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med 348(6):518–527. doi:10.1056/NEJMoa021641
Nakagawa M, Kim KH, Moscicki AB (2005) Patterns of CD8 T-cell epitopes within the human papillomavirus type 16 (HPV 16) E6 protein among young women whose HPV 16 infection has become undetectable. Clin Diagn Lab Immunol 12(8):1003–1005. doi:10.1128/CDLI.12.8.1003-1005.2005
Kaul R, Dong T, Plummer FA, Kimani J, Rostron T, Kiama P, Njagi E, Irungu E, Farah B, Oyugi J, Chakraborty R, MacDonald KS, Bwayo JJ, McMichael A, Rowland-Jones SL (2001) CD8(+) lymphocytes respond to different HIV epitopes in seronegative and infected subjects. J Clin Invest 107(10):1303–1310. doi:10.1172/JCI12433
Kadish AS, Timmins P, Wang Y, Ho GY, Burk RD, Ketz J, He W, Romney SL, Johnson A, Angeletti R, Abadi M (2002) Regression of cervical intraepithelial neoplasia and loss of human papillomavirus (HPV) infection is associated with cell-mediated immune responses to an HPV type 16 E7 peptide. Cancer Epidemiol Biomarkers Prev 11(5):483–488
Steele JC, Mann CH, Rookes S, Rollason T, Murphy D, Freeth MG, Gallimore PH, Roberts S (2005) T-cell responses to human papillomavirus type 16 among women with different grades of cervical neoplasia. Br J Cancer 93(2):248–259. doi:10.1038/sj.bjc.6602679
Trimble CL, Peng S, Thoburn C, Kos F, Wu TC (2010) Naturally occurring systemic immune responses to HPV antigens do not predict regression of CIN2/3. Cancer Immunol Immunother 59(5):799–803. doi:10.1007/s00262-009-0806-4
Kim KH, Dishongh R, Santin AD, Cannon MJ, Bellone S, Nakagawa M (2006) Recognition of a cervical cancer derived tumor cell line by a human papillomavirus type 16 E6 52–61-specific CD8 T cell clone. Cancer Immun 6:9. doi:060609
Heusinkveld M, Welters MJ, van Poelgeest MI, van der Hulst JM, Melief CJ, Fleuren GJ, Kenter GG, van der Burg SH (2011) The detection of circulating human papillomavirus-specific T cells is associated with improved survival of patients with deeply infiltrating tumors. Int J Cancer 128(2):379–389. doi:10.1002/ijc.25361
Mougiakakos D, Choudhury A, Lladser A, Kiessling R, Johansson CC (2010) Regulatory T cells in cancer. Adv Cancer Res 107:57–117. doi:10.1016/S0065-230X(10)07003-X
Acknowledgments
This study was supported by an American Cancer Society Scholars Award (RSG-06-180-01-MBC) and NIH grants (R01 CA143130 and UL1RR029884). The authors would like to thank the subjects for participating in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, K.H., Greenfield, W.W., Cannon, M.J. et al. CD4+ T-cell response against human papillomavirus type 16 E6 protein is associated with a favorable clinical trend. Cancer Immunol Immunother 61, 63–70 (2012). https://doi.org/10.1007/s00262-011-1092-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-011-1092-5