Abstract
The collapsin response mediator protein 5 (CRMP5) antibody is usually associated with paraneoplastic neurological syndrome (PNS) and small-cell lung cancer (SCLC) or thymoma. The objective of this study was to assess the frequency of CRMP5 antibodies in patients with such tumours and to see if the presence of antibodies was associated with prognosis in these cancers. A multi-well adapted immunoprecipitation assay using radiolabelled recombinant CRMP5 protein, produced by coupled in vitro transcription/translation, was used for the detection of CRMP5 antibodies. Sera from 200 patients with SCLC, 73 patients with thymoma and myasthenia gravis (MG) and from 300 healthy blood donors were examined for CRMP5 antibodies. Positive sera were also examined by immunofluorescence and immune blots. The serological results were compared with disease severity of the patients with thymoma or SCLC. CRMP5 antibodies were detected in 10/200 (5%) of the SCLC, 9/73 (12%) of the thymomas and in 2/300 (0.6%) of the healthy controls by immunoprecipitation. The antibodies were less frequently detected by immunofluorescence or immune blots. There was no significant correlation between CRMP5 antibodies and disease severity. CRMP5 antibodies are more than twice as frequent, and the antibody levels are higher in patients with thymoma and MG than in patients with SCLC. The antibodies are correlated to these tumours, but not to disease severity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antitumor immune responses initiated by neuronal antigens expressed by cancer cells may result in marker antibodies that can be detected in serum. These onconeural antibodies are often associated with paraneoplastic neurological syndrome (PNS) (for a review see [1]), but such antibodies can also be found in cancer patients without neurological symptoms [2–7].
Antibodies against collapsin response mediator protein 5 (CRMP5) are commonly associated with PNS [8]. These antibodies are directed against a cytoplasmic phosphoprotein which is involved in signal transduction in neural cells. CRMP5 antibodies are found in different PNS, usually associated with small-cell lung cancer (SCLC) or less frequently thymoma [8] and is reported to be almost as frequent as anti-Hu [4].
The common techniques used for detection of onconeural antibodies are immunhistochemistry and immune blot with neuronal extracts or recombinant proteins. We have recently established a very sensitive immunoprecipitation technique for the detection of Hu, Yo and Ri antibodies [5–7, 9]. In this study we have applied the same immunoprecipitation technique to examine the prevalence of CRMP5 antibodies in 200 patients with SCLC, 73 patients with thymoma and myasthenia gravis (MG) and 300 blood donors. We have also correlated the results of the immunoprecipitation technique with the results of immunofluorescence and immune blot, as well as with disease severity. The results showed that the immunoprecipitation assay was the most sensitive for detecting CRMP5 antibodies, but these antibodies could not be used as prognostic disease markers.
Patients and methods
Patients
Two hundred unselected patients with newly diagnosed SCLC (age 39–79, mean 62.3 years; 64.5% males and 35.5% females) admitted to four hospitals in the “Copenhagen Lung Cancer Study group”, Denmark, in the period June 1990 to January 1993 were included in the study, see [5] for clinical details. Survival was determined from start of treatment to death or last visit. Follow up time for long time survivors was at least 9 years.
Seventy-three patients with thymoma and MG (age 19–74, mean 50.5 years (the age of 7 patients were missing), 55% males and 45% females) admitted to the Department of Neurology, Haukeland University Hospital, Bergen, Norway (33 patients), Institute of Neurology, Catholic University, Rome, Italy (32 patients) and Neurologische Universität Klinik, Hamburg, Germany (8 patients) in the period 1980–2004, were included in the study. The patients were positive for AChR antibodies and had surgical resection of thymic epithelial tumours. Twenty-one (28%) of the thymomas were invasive and 30 (41%) were non-invasive. The histology of the other 22 thymomas was not available. All patients received conventional treatment with pyridostigmine and severe cases also with prednisolone and azathioprine. All patients but three survived during the study period. The MG symptoms were available for 58 (78 %) and were classified as previously described [10].
Sera were obtained before start of treatment and kept at −80°C until use. All patients signed informed consent for participation in the study.
Sera from 300 healthy blood donors at the Haukeland University Hospital were used as normal controls.
CRMP5 antibody detection
In vitro transcription–translation and immunoprecipitation
A Bluescript SK plasmid containing the CRMP5 cDNA (kindly provided by Dr Jerome Honnorat, Hôpital Neurologique, Lyon, France) was multiplied and purified following procedures previously described [5].
Recombinant 35S labelled (35S methionine, Amersham Biosciences, Uppsala, Sweden) CRMP5 protein was produced in a coupled transcription/translation system (ITT) with a T3 RNA polymerase and nuclease treated rabbit reticulocyte lysate (Promega, Madison, WI, USA). The amount of radiolabelled CRMP5 produced was determined by trichloroacetic acid precipitation on glass–fibre filters (Millipore, Bedford, MA, USA) followed by vacuum filtration and liquid scintillation counting (Packard Tri-Carb, Packard Biosciences B.V., Groningen, the Netherlands). The ITT product was quality checked by SDS-PAGE and visualized by photostimulated luminescence imaging (Bio-image analyzer Bas 2000; Fuji Photo Film, Tokyo, Japan). The radiolabelled product had the expected molecular weight of 62 kDa [8].
Patient sera were screened by immunoprecipitation [6], employing 35S labelled CRMP5 (20,000–30,000 cpm/well) and a 1:20 dilution of sera.
Pooled sera from 100 blood donors were used as a negative control. A polyclonal rabbit antibody (Eurogentec s.a., Seraing, Belgium) against two synthetic peptides corresponding to amino acid 512–526 (ADTPTRPVTRHGGMRD) and amino acid 549–564 (SARILAPPGGRSSGIW) of the human CRMP5 sequence was used as positive control. The peptides were coupled to keyhole limpet hemocyanin (KLH). Control tests using preimmune rabbit sera were negative.
Each patient serum sample was run in triplicate and the mean value of these three was used. The results were expressed as a CRMP5 index: (cpm sample − cpm negative control)/(cpm positive control − cpm negative control) × 1,000. A CRMP5 index greater than 213 was considered as positive, based on the mean + 3SD of 300 normal sera controls. Positive results were repeated by immunoprecipitation for verification.
Immunofluorescence and immune blot
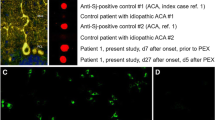
Sera from patients with CRMP5 antibodies detected by immunoprecipitation were also examined by immunofluorescence (IF) and immune blots. Rat cerebellar and brainstem tissue was fixed post mortem by immersion in 4% paraformaldehyde in 0.1 M phosphate buffer for 48 h. The brain tissue was subsequently rinsed in 0.1 M phosphate buffer, cryoprotected by 20% sucrose in 0.1 M phosphate buffer and snap-frozen. Microscope slides with cryostat sections of fixed tissue were incubated with patient sera diluted 1:100 and 1:500 in PBT (PBS with 1% BSA and 0.2% Triton X), in a moist chamber at 4°C o/n. The slides were washed with PBT and incubated with Alexa fluor 488 goat anti-human IgG (Molecular probes, Eugene, OR, USA) diluted 1:100 in PBT, for 90 min at room temperature. Finally, the slides were washed in PBS, covered and examined by fluorescence microscopy (Leica DM IL, Leica Microsystems Ltd, Heerbrugg, Switzerland). Cytoplasmic staining of oligodendrocytes and neurones was suggestive of CRMP5 antibody reactivity.
Sera were also tested by line blot, employing a commercial kit (Ravo Diagnostika, Freiburg, Germany) that contains the recombinant proteins HuD, Yo (cdr2), Ri (Nova-1) CV2 (CRMP5), Ma2 and amphiphysin. The samples were diluted 1:2,000 following the instructions of the manufacturer. Distinct bands corresponding to the CRMP5 position in the line blot were interpreted as positive. Furthermore, the sera (diluted 1:50 or 1:100 in PBS) were tested by Western blot as recently described [6], using rat cerebrum homogenate or purified bacterial recombinant CRMP5 (kindly provided by Dr Jerome Honnorat, Hôpital Neurologique, Lyon, France). Distinct bands corresponding to a molecular weight of approximately 62 kDa were considered positive [8].
Results
Controls
The mean CRMP5 index of the 300 blood donors was −19. A CRMP5 index of 213 was set as the upper normal limit (mean CRMP5 index of the 300 sera + 3SD). Two of the 300 controls (0.6%) had a CRMP5 index of 438 and 394, respectively. One of them was positive on Western blot with cerebrum homogenate, but none of them were tested with recombinant protein because of shortage of this protein. The remaining 298 controls were below the cut-off limit. None of the control sera were positive by IF or the commercial line-blot.
SCLC
CRMP5 antibodies were detected in sera from 10 of 200 SCLC patients (5%). The CRMP5-index ranged from 282 to 1,058; mean 512, median 459 (Fig. 1). High CRMP5 index (>500) was found in five of the SCLC patients. Only one of the SCLC samples was positive by the commercial line-blot, and revealed clear oligodendrocyte staining by IF. By Western blot, six were positive with cerebrum homogenate and eight by purified recombinant CRMP5 (Table 1).
The mean age of the CRMP5 positive SCLC patients was 66 years (7 men and 3 women) which was similar to the CRMP5 negative patients (P = 0.16, independent sample t test). There was no significant difference between CRMP5 positive and CRMP5 negative patients with limited (6/94) (6.4%) and advanced (4/106) (3.8%) disease (P = 0.52, Fisher’s Exact Test). Kaplan–Meier survival curves for CRMP5 positive or negative patients are illustrated in Fig. 2. There was a no significant trend towards longer survival among the CRMP5 negative SCLC patients (P = 0.09, Log-Rank test), but this trend was reduced in a multivariate cox-regression model including extent of disease (P = 0.21).
Thymoma
CRMP5 antibodies were detected in serum from 9 of 73 (12%) patients with thymoma and MG (range 332–1336, mean 803, median 864). The frequency of CRMP5 antibodies in thymoma was almost significantly higher than in SCLC (P = 0.056, Fisher’s Exact Test), and the median CRMP5 index was significantly higher in thymoma than in SCLC sera (P = 0.042, independent sample Mann–Whitney test). High CRMP5 indices (>500) was found in eight of the thymomas. By IF, CRMP5 antibodies were detected in five of the thymoma samples, while four sera were positive by the commercial line-blot technique (Table 1). By Western blot, five were positive with cerebrum homogenate and eight by purified recombinant CRMP5.
The mean age of the CRMP5 positive patients was 47.4 years (5 men and 4 women), which was similar to the CRMP5 negative patients (P = 0.49, independent sample t test). Six patients with CRMP5 antibodies had a non-invasive thymoma, one had an invasive thymoma while the histology of the last two were not known. Non-invasive thymoma was not correlated to CRMP5 antibodies (P = 0.22, Fisher’s Exact Test), but the number of observations was low (statistical test power = 0.5). Three of the CRMP5 positive patients had additional inflammatory diseases (1 myocarditis, 1 pemphigus and 1 limbic encephalitis), whereas only one of the CRMP5 negative patients had polymyositis. All four patients with additional inflammatory diseases had a non-invasive thymoma. There was no correlation between the presence of CRMP5 antibodies and the severity of MG symptoms (P = 0.93, Fisher’s Exact Test).
Discussion
We have analysed serum samples from 200 patients with SCLC, 73 patients with thymoma and MG, and 300 blood donors for the presence of CRMP5 antibodies. This is, to our knowledge, the largest tumour and normal serum material that has been systematically analysed for CRMP5 antibodies.
The immunoprecipitation technique was more sensitive in detecting CRMP5 antibodies than IF and immune blots. The increased sensitivity of immunoprecipitation may be due to the use of radioactive labelling, the native property of the technique [6] as well as lower dilutions of serum. The dilution of 1:20 is in the same range as used for the detection of antibodies such as GAD65 and 21 hydroxylase [11, 12]. The various techniques employed for the detection of CRMP5 antibodies are optimised with quite different dilutions of sera, and using a common dilution in all leads to either loss of specificity or sensitivity of the different methods [9]. Onconeural antibodies are strongly related to tumours, and it is therefore important to use as sensitive serological assay as possible.
Two of the blood donors harboured CRMP5 antibodies detected by immunoprecipitation, and one of them also by Western blot with cerebrum homogenate. Unfortunately, we do not have any clinical information about these individuals.
CRMP5 antibodies were more than twice as frequent in thymoma with MG than in SCLC, and the levels of CRMP5 antibodies were higher in thymoma with MG than in SCLC. These findings could be partly due to the fact that all thymoma patients had MG, whereas it is not known if any of the SCLC patients also had neurological symptoms. In a recent study on autoantibody profiles in thymoma, CRMP5 antibodies were found in 17% of thymoma patients with MG and in 7% of thymoma patients without neurological disease [13]. However, CRMP5 antibodies were found in 7/74 (9%) SCLC patients with no PNS and in 18/167 (11%) patients with PNS and SCLC or other neuroendocrine tumours [14]. Taken together, the results indicate that CRMP5 antibodies are almost as frequently found in SCLC patients with or without PNS whereas CRMP5 antibodies in thymoma patients are much more common in patients who also have MG.
CRMP5 antibodies have previously been detected in 121 of 68,000 patients evaluated for possible PNS; 77% of these had lung cancer and only 6% had thymoma [8]. Since SCLC is much more common than thymoma in a general population, SCLC patients with CRMP5 antibodies are much more frequently encountered in such a study and the distribution of CRMP5 antibodies is therefore biased towards SCLC. The frequency of CRMP5 antibody detection in paraneoplastic diagnostic service is 2 of 1,000, which is approximately the same as for anti-Yo [8]. However, in a more recent report from the same group, CRMP5 antibodies were detected twice as common as Yo antibodies, and were found in 208 of 60,000 sera [4]. This gives a CRMP5 prevalence of 0.35%, whilst the prevalence of Hu was 0.36% and Yo 0.17% in the same material [4]. Recently, we detected Yo antibodies in 13 of 557 (2.3%) of ovarian cancer and 4 of 253 (1.6%) of breast cancer [6], which makes CRMP5 antibodies in thymoma and SCLC much more common than Yo antibodies are in ovarian and breast cancer.
In an earlier report, we found Hu antibodies in 25.5% of patients with SCLC using immunoprecipitation [5]. In comparison, we found CRMP5 antibodies in 5% of the same SCLC patients in this study. Six of the 200 SCLC patients (3%) harboured both Hu and CRMP5 antibodies, but this was not correlated (data not shown). SCLC is associated with several different PNS and numerous onconeural antibodies [15], and the HuD protein is expressed by all SCLC tumours [16, 17]. The CRMP5 protein has been detected in 20 of 20 SCLC cell lines [8], and is probably present in all SCLC. However, the CRMP5 protein has not been detected in 17 thymomas indicating that thymomas do not express CRMP5 or only express CRMP5 at a low level or in an altered form [18]. Thus, there may be a major difference in CRMP5 expression in thymoma and SCLC.
The presence of CRMP5 antibodies did not correlate to the severity of MG. However we found CRMP5 antibodies mainly in patients with non-invasive thymoma suggesting an association between CRMP5 and benign disease, although no significant. CRMP5 antibodies did not correlate with the prognosis of the SCLC, but there was a trend towards longer survival for the CRMP5 negative patients. However, since the mortality is high among SCLC patients and the number of CRMP5 positive patients is low, a very large number of patients are needed to determine if CRMP5 antibodies have an impact on the prognosis of SCLC.
References
Roberts WK, Darnell RB (2004) Neuroimmunology of the paraneoplastic neurological degenerations. Curr Opin Immunol 16:616–622
Graus F, Dalmau J, Rene R, Tora M, Malats N, Verschuuren JJ, Cardenal F, Vinolas N, Garcia del Muro J, Vadell C, Mason WP, Rosell R, Posner JB, Real FX (1997) Anti-Hu antibodies in patients with small-cell lung cancer: association with complete response to therapy and improved survival. J Clin Oncol 15:2866–2872
Drlicek M, Bianchi G, Bogliun G, Casati B, Grisold W, Kolig C, Liszka-Setinek U, Marzorati L, Wondrusch E, Cavaletti G (1997) Antibodies of the anti-Yo and anti-Ri type in the absence of paraneoplastic neurological syndromes: a long-term survey of ovarian cancer patients. J Neurol 244:85–89
Pittock SJ, Kryzer TJ, Lennon VA (2004) Paraneoplastic antibodies coexist and predict cancer, not neurological syndrome. Ann Neurol 56:715–719
Monstad SE, Drivsholm L, Storstein A, Aarseth JH, Haugen M, Lang B, Vincent A, Vedeler CA (2004) Hu and voltage-gated calcium channel (VGCC) antibodies related to the prognosis of small-cell lung cancer. J Clin Oncol 22:795–800
Monstad SE, Storstein A, Dorum A, Knudsen A, Lonning PE, Salvesen HB, Aarseth JH, Vedeler CA (2006) Yo antibodies in ovarian and breast cancer patients detected by a sensitive immunoprecipitation technique. Clin Exp Immunol 144:53–58
Knudsen A, Monstad SE, Dorum A, Lonning PE, Salvesen HB, Drivsholm L, Aarseth JH, Vedeler CA (2006) Ri antibodies in patients with breast, ovarian or small cell lung cancer determined by a sensitive immunoprecipitation technique. Cancer Immunol Immunother 55:1280–1284
Yu Z, Kryzer TJ, Griesmann GE, Kim K, Benarroch EE, Lennon VA (2001) CRMP-5 neuronal autoantibody: marker of lung cancer and thymoma-related autoimmunity. Ann Neurol 49:146–154
Storstein A, Monstad SE, Nakkestad HL, Husebye ES, Vedeler CA (2004) Paraneoplastic antibodies against HuD detected by a sensitive radiobinding assay. J Neurol 251:197–203
Mygland A, Aarli JA, Matre R, Gilhus NE (1994) Ryanodine receptor antibodies related to severity of thymoma associated myasthenia gravis. J Neurol Neurosurg Psychiatr 57:843–846
Falorni A, Nikoshkov A, Laureti S, Grenback E, Hulting AL, Casucci G, Santeusanio F, Brunetti P, Luthman H, Lernmark A (1995) High diagnostic accuracy for idiopathic Addison’s disease with a sensitive radiobinding assay for autoantibodies against recombinant human 21-hydroxylase. J Clin Endocrinol Metab 80:2752–2755
Falorni A, Ortqvist E, Persson B, Lernmark A (1995) Radioimmunoassays for glutamic acid decarboxylase (GAD65) and GAD65 autoantibodies using 35S or 3H recombinant human ligands. J Immunol Methods 186:89–99
Vernino S, Lennon VA (2004) Autoantibody profiles and neurological correlations of thymoma. Clin Cancer Res 10:7270–7275
Bataller L, Wade DF, Graus F, Stacey HD, Rosenfeld MR, Dalmau J (2004) Antibodies to Zic4 in paraneoplastic neurologic disorders and small-cell lung cancer. Neurology 62:778–782
Graus F, Delattre JY, Antoine JC, Dalmau J, Giometto B, Grisold W, Honnorat J, Smitt PS, Vedeler C, Verschuuren JJ, Vincent A, Voltz R (2004) Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatr 75:1135–1140
Dalmau J, Furneaux HM, Cordon-Cardo C, Posner JB (1992) The expression of the Hu (paraneoplastic encephalomyelitis/sensory neuronopathy) antigen in human normal and tumor tissues. Am J Pathol 141:881–886
Dalmau J, Graus F, Cheung NK, Rosenblum MK, Ho A, Canete A, Delattre JY, Thompson SJ, Posner JB (1995) Major histocompatibility proteins, anti-Hu antibodies, and paraneoplastic encephalomyelitis in neuroblastoma and small cell lung cancer. Cancer 75:99–109
Camdessanche JP, Lassabliere F, Meyronnet D, Ferraud K, Absi L, Honnorat J, Antoine JC (2006) Expression of the onconeural CV2/CRMP5 antigen in thymus and thymoma. J Neuroimmunol 174:168–173
Acknowledgments
The authors thank Cecilie Totland, Mette Haugen and Kibret Mazengia for technical assistance. We also wish to tank professor Jerome Honnorat, Hospital Neurologique, Lyon, France for kindly providing us with a CRMP5 plasmid and purified recombinant CRMP5 protein, Professor Amelia Evoli, Institute of Neurology, Catholic University, Rome, Italy and Dr Janzen, Neurologische Universität Klinik, Hamburg, Germany for providing some of the thymoma patient sera. This study was supported by grants from Haukeland University Hospital and the University of Bergen, Norway.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Monstad, S.E., Drivsholm, L., Skeie, G.O. et al. CRMP5 antibodies in patients with small-cell lung cancer or thymoma. Cancer Immunol Immunother 57, 227–232 (2008). https://doi.org/10.1007/s00262-007-0369-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-007-0369-1