Abstract
With the successful identification of many tumor-specific antigens, tumor-associated antigens, and the potential of using unfractioned tumor cell derivatives as tumor antigens, a system and/or adjuvant that can deliver these antigens and help them to induce strong and effective anti-tumor immune responses is greatly needed. Previously, we reported that a MHC class I-restricted peptide epitope derived from human papillomavirus (HPV) 16 E7 protein, when incorporated into a clinically proven safe LPD (liposome-polycation-DNA) particle, was able to effectively eradicate tumors established in mice. Cervical cancer is the second most common cancer among women worldwide. HPV infection is clearly linked to this cancer. Vaccines based on the early (E) gene products of HPV could be effective in controlling it. However, besides the fact that epitope vaccines have many limitations particularly, concerning the diverse HLAs in humans, the use of the epitope as an antigen prevented us from fully characterizing the immune responses induced by the LPD as a vaccine carrier and/or adjuvant in previous studies. In the present study, by using the HPV 16 E7 protein as an antigen, we first showed that LPD, as a vaccine carrier and adjuvant induced strong and robust immune responses, both cellular and antibody. We then showed that immunization with LPD particles incorporated with either the wild type HPV 16 E7 protein or a potentially safer mutant induced strong immune responses that caused complete regressions of a model cervical cancer tumor established in murines. LPD could be a potent vaccine carrier and/or adjuvant for many antigens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
After decades of debate over whether the immune system can actually fight tumors, growing and compelling evidence now suggests that the immune cells play an important role in the control of malignancy [1–3]. However, there still are many major hurdles in developing cancer vaccines, including the identification of antigens that induce immune responses specifically targeting tumor cells without harming normal cells and the development of methods that induce immune responses sufficient to eradicate tumors [4]. Over the last decade, numerous tumor-associated antigens (TAAs) and tumor-specific antigens (TSAs) recognized by tumor-reactive CTLs have been identified [5, 6]. Unfractionated tumor derivatives, such as total tumor lysates, peptides, or proteins, may also be used as tumor antigens. Studies have shown that immunization by reintroducing dendritic cells (DCs) pulsed with tumor antigens or total tumor derivatives into patients led to strong anti-tumor activities [7–18]. However, ex vivo vaccination with autologous patient DCs is not preferred because it is costly, time-consuming, and very inconvenient to patients. Novel delivery systems and/or adjuvants that allow direct injection of tumor antigens to induce anti-tumor immune responses are needed.
Cervical cancer is the second most common cancer among women worldwide. About 45% of cervical cancer patients die as a result of distant metastasis [19]. Over the last 20 years, the relationship between HPV infection and cervical cancer has been extensively investigated. More than 95% of cervical cancer cells contain HPV DNA, with HPV 16 being the most common type, accounting for about 50% of all cases [20]. HPV contains a double stranded DNA genome, which can be separated into three regions: the early genes (E), the late genes (L), and the non-coding upstream regulatory region (URR). L genes encode structural proteins such as the major capsid protein L1 and the minor capsid protein L2. The major transforming proteins are coded by the E genes such as E6 and E7; their expression induces cell immortalization and transformation in many cell types [21, 22]. E6 and E7 of the “high risk” viruses bind to p53 and pRB, respectively, and inhibit their tumor suppressor functions [23, 24]. For example, E7 targets pRB family proteins for ubiquitin-mediated proteolysis that leads to decreased pRB level [24]. Also, E7 protein has a strong affinity to pRB protein. Binding of E7 to pRB releases E2F factor. This eventually causes the cell growth to lose control [24, 25].
Vaccination has been suggested as an effective approach to prevent and treat cervical cancers caused by HPV. The recently developed HPV virus-like particles (VLP) by over expression of L1 alone or co expression of L1 and L2 have demonstrated a great potential as a prophylactic vaccine [26–29]. However, for therapeutic purpose, a HPV capsid protein-based vaccine is unlikely to have any significant benefit because these proteins are not detectable in the basal epithelial cells that developed into tumors. E6 and E7 proteins are expressed in almost all the cervical cancer cells and their precursors [30, 31]. They are excellent cervical cancer-specific antigens that may be developed into therapeutic vaccines. In fact, many animal studies have shown that immunization with either E7 protein, peptide epitopes derived from E7 protein, or E7 gene carried on a plasmid or a viral vector caused regression of experimentally grafted E7-expressing tumors [30, 32–47], if an appropriate adjuvant was used. Several clinical trials have also been completed [24, 48–52]. For example, in a phase I trial, 18 women with high grade cervical or vulvar intraepithelial neoplasia (CIN) and positive HPV-16 were given a HLA-A2-restricted peptide (E712-20) in Montanide ISA-51 (Seppic, Inc), which has been used many in clinical trials [52–64]. DC infiltrate was observed in 6 out of 6 patients. CTL response was observed in 10 out of 16 patients. Also, 3 out of 18 patients cleared their dysplasia after vaccination [50].
Previously, a liposome-based DNA delivery system named LPD, was developed by us [65, 66]. LPD was engineered by combining cationic liposomes and polycation condensed DNA. Upon mixing, the components rearrange to form a virus-like structure with the condensed DNA inside the lipid membrane [65, 66]. When administered systemically, the LPD rapidly initiates the production of several T helper type 1 (Th1) cytokines, most notably TNF-α, IL-12, and IFN-γ [67, 68]. This non-specific immunostimulation is associated with tumoristatic effects [67, 68]. More recently, we have found that when a MHC class I-restricted peptide epitope (E749-57) derived from the HPV 16 E7 protein was incorporated into the LPD and then used to immunize mice, strong anti-tumor responses, including CTL responses specific to E749-57, were observed [69]. Administration of LPD/E749-57 to tumor-bearing mice caused tumor regressions [69].
Although immunization with the E749-57 peptide epitope resulted in a potent anti-tumor activity, immunization with the whole E7 protein might be more effective because there are multiple MHC class I and II restricted epitopes on the E7 protein. The existence of highly diverse MHC I and II molecules among human populations also makes the whole E7 protein more attractive [70]. In addition, the E7 protein as an antigen will allow us to further characterize the immune responses induced by the LPD as a vaccine carrier and/or adjuvant. In the present study, using the E7 protein as an antigen, we have shown that the LPD as an antigen carrier induced very strong and robust CTL and antibody responses. The immune responses are sufficient to treat tumors pre-established in mice.
Materials and methods
Materials
Plasmid pET-E7 was a gift from Dr. Jeong-Im Sin at the Catholic University of Korea (Seoul, Korea). Dioleoyl trimethylammonium propane (DOTAP) and cholesterol were purchased from Avanti Polar Lipids, Inc. (Alabaster, AL). Protamine sulfate (fraction X from salmon) was purchased from Sigma-Aldrich (St. Louis, MO). Plasmid (pNGVL3) containing the CMV promoter without coding insert was obtained from the National Gene Vector Laboratory (Ann Arbor, MI). It was purified using Qiagen EndoFree Giga-Prep kit (Qiagen, Valencia, CA). TC-1 cells were obtained from Dr. T. C. Wu of the Johns Hopkins University. The cells were C57BL/6 mouse lung endothelial cells transformed with HPV 16 E6 and E7 oncogenes and activated H-ras gene. Cells were grown in RPMI 1640 medium (Invitrogen, Carlsbad, CA) supplemented with 10% fetal bovine serum (FBS), 100 U/ml of penicillin (Sigma-Aldrich, St. Louis, MO), and 100 μg/ml of streptomycin (Sigma).
Construction of mutants on the E7 gene
It has been shown that change of amino acid D21 into G21 in HPV 16 E7 protein dramatically decreased its tumor transformation ability, and that replacement of G22 of a ‘low risk’ HPV type 6 E7 protein by D22 increased its tumor transformation ability to a level comparable to that of “high risk” HPV type 16 E7 protein [71, 72]. Furthermore, in the C terminal of E7, there are two CXXC motifs, which form a zinc finger structure. Disruption of this structure by replacing one of the C residues with a G has been shown to severely reduce the cell immortalization ability of E7 [73, 74]. Overlapping PCR was used to introduce mutations in the E7 protein. Amino acids D21 and C94 on HPV 16 E7 protein were changed to G21 and G94 by changing their codons from GAT to GGT and TGT to GGT, respectively. The four primers used were P1, 5-TTGGGATCCACCATGCATGGAGATACACCTAC-3; P2, 5-CGGAATTCATTCTTATGGTTTCTGAGAACCGATGGGGCACACA-3; P3, 5-GAGACAACTGGTCTCTACTGTTAT-3; and P4, 5-ACAGTAGAGACCAGTTGTCTCTGG-3. Using pET-E7 as the template, two separate PCRs were completed using primer pairs P1/P4 and P2/P3. The PCR products were purified using QiaQuick PCR purification kit (Valencia, CA). Another PCR was completed using P1 and P2 as primers and molar equivalents of the products from the previous two PCRs as templates. The PCR conditions were 94°C for 5 min followed by 35 cycles of 94°C, 0.5 min, 56°C, 1 min, and 72°C, 0.5 min. Another 5 min of incubation at 72°C was included prior to the end of the PCR reaction. Taq DNA polymerase and dNTP were obtained from Promega (Madison, WI). After purification, the PCR product was then ligated to the pGEM-T vector from Promega. The ligation reaction was then transferred into E. coli DH5α strain. Positive colonies were selected using LB/ampicillin/IPTG/X-Gal plates. After confirmation of mutations on the E7 gene of the pGEM-T-E7m by DNA sequencing, the plasmid was digested with BamHI and EcoRI. The resulting DNA fragment was gel purified and then cloned into the BamHI and EcoRI site of pCDNA3.1(+) vector (Invitrogen) and pET vector (Novagen, Madison, WI), respectively. The plasmid constructs were transferred into E. coli DH5α and selected against ampicillin and kanamycin, respectively .
Purification of recombinant E7 and E7m proteins
His-tagged recombinant E7 and E7m proteins were purified as previously described [75]. To purify E7 and E7m proteins, the pET-E7 and pET-E7m plasmids were purified and transformed into BL21 (DE3) cells. A single colony was seeded into LB broth supplemented with kanamycin at a final concentration of 50 μg/ml. The cells were incubated at 37°C shaker until the absorbance at 600 nm was between 0.6 and 0.8. Protein production was induced using 0.5 mM of isopropy-1-thio-β-D-galactopyranoside for 4 h. The cell pellets were collected by centrifugation at 8,000 g for 20 min, frozen-thawed once at −20°C, and then re-suspended in 8 M urea buffer (pH 8.0) (5 ml per 1 mg of wet cell pellet). The cells were lysed by stirring at 37°C for 1 h. The lysate was centrifuged at 10,000 g for 30 min at room temperature. The supernatant was collected and mixed with 50% Ni-NTA slurry at a ratio of 4:1. The mixture was gently shaken for 1 h at room temperature. The lysate-resin mixture was then loaded into an empty column provided by Qiagen, and washed with 5 vol of Buffer B (8 M urea, pH 8.0), followed by 10 vol of Buffer C (8 M urea, pH 6.3). His-tagged proteins were eluted with 10 ml of Buffer C containing 200 mM imidazole. The protein solution was then dialyzed in 6 M urea buffer for 2 h followed by two more hours in 4 M urea buffer. After overnight dialysis in phosphate buffered saline (pH 7.0), the protein solution was collected and passed through a Detoxi-Gel endotoxin removing gel column from Pierce (Rockford, IL). The protein concentration was quantified using Coomassie Plus protein assay reagent (Pierce). The protein purity was confirmed by electrophoresis on a BioRad Ready Gel (4–20% SDS polyacrylamide gel) (Hercules, CA). Endotoxin was determined to be <100 EU/mg protein using the Limulus Amebocyte Lysate (LAL) pyrochrome kit from the Associates of Cape Cod Incorporated (Falmouth, MA). Similar to previous reports, the recombinant E7 protein migrated as a 23 KDa protein on SDS-PAGE gel [28]. The yield was roughly 1 mg/l of bacterial culture.
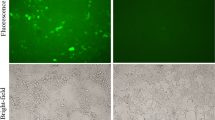
Verification of E7m protein’s inability to activate E2F driven genes
An indirect method was used to verify that the E7m is unable to activate E2F driven genes. E7 and E7m genes were inserted into the BamHI and EcoRI sites of pCDNA3.1(+) vector. The resulting plasmids were amplified in E. coli DH5α strain and purified. Plasmid cdc25A Sac I-luc, in which luciferase gene is driven by a 1173 (−755 to + 418) bp Sac I fragment of the cdc25A promoter, is a gift from Dr. D. DiMaio of Yale University [46]. The Sac I fragment has the E2F binding site. Plasmid cdc25A Sac I-luc, pCDNA3.1(+) with or without E7 or E7m insert, and a CMV driven β-galactosidase gene containing plasmid were co-transfected into confluent 293 cells (5×105 /well, incubated at 37°C and 5% CO2 overnight, DMEM medium with 10% FBS) with Lipofectamine (Invitrogen). The plasmid ratio was 2:1:10 (w/w/w) with pCDNA3.1(+) plasmid at 1 μg/well. Four hours after the addition of the plasmids, the medium was replaced with a fresh medium. After another 44 h, cells were washed with cold PBS (10 mM, pH 7.4) twice and lysed. Luciferase activity, β-galactosidase expression, and total protein amount were then determined. The same experiment was repeated three times.
Preparation of liposome and LPD
Liposomes and LPD were prepared as previously described [69]. Briefly, small unilamellar liposomes composed of DOTAP: cholesterol (molar ratio 1:1) were prepared by thin film hydration followed by membrane extrusion. DOTAP concentration was fixed at 10 mg/ml. The LPD was comprised of DOTAP/cholesterol liposomes, protamine, and plasmid DNA in a ratio of 9.0:0.6:1.0 (w/w/w). To prepare LPD, required amounts of liposome (43 μl) and protamine (15 μl, 2 mg/ml) were dispersed in 150 μl of aqueous solution containing 10% of dextrose (Sigma). Then, 150 μl aqueous solution containing pDNA (50 μg) with E7 protein or E7m protein (40 μg) was added drop wise into the mixture of liposome and protamine with gentle shaking. The complex was then allowed to stay at room temperature for at least 20 min prior to use. The incorporation efficiency of the protein was estimated by SDS-PAGE gel electrophoresis to be around 60%.
The particle size of the protein incorporated LPD particles were measured using a Coulter N4 Plus particle sizer (Beckman Coulter, San Francisco, CA). The size of the E7 incorporated LPD was 191±7 (polydispersity index, 0.001) nm; the size of the E7m incorporated LPD was 210±32 (PI, 0.026) nm. They were not significantly different from each other.
Mouse tumor treatment study
Six-week-old female C57BL/6 mice (Charles River Laboratories, Wilmington, MA) were used in all animal studies. National Institutes of Health guidelines for the care and use of laboratory animals were observed. Subcutaneous tumors were established by injecting 5×105 TC-1 cells in the flank on day 0. On specific day(s), mice were then subcutaneously injected with the E7 protein alone (20 μg/mouse), LPD/E7, or E7 adjuvanted with Alum (15 μg/mouse). One group of mice was left untreated. All formulations were in 150 μl of 5% dextrose to maintain isotonicity. The corresponding cationic liposome amount injected was about 140 μg. When Montanide ISA-51 was used, 50 μl (20 μg) E7m in 15% dextrose solution was mixed with 100 μl of Montanide ISA-51 (Seppic, Inc., France). The mixture is a very viscous white suspension. Tumor size was measured using a caliper and reported by multiplying the two largest dimensions of the tumor. Same experiment was repeated two or three times.
ELISA
Specific serum IgG levels against E7 and E7m proteins were determined using ELISA. Briefly, Costar high binding 96-well assay plates were coated with 100 μl (10 mM sodium phosphate buffer, pH 9.6) of E7 or E7m protein (1 μg/well) overnight at 4°C. The plates were then washed once with phosphate buffered saline (10 mM, pH 7.4) and blocked for 1 h at 37°C with 5% bovine serum albumin (BSA) (Sigma) solution (100 μl/well) made in sodium phosphate buffer as above. The plates were then washed five times with PBS/Tween 20 buffer. Mouse serum was diluted 10, 100, and 1000 times with 4% BSA, and 50 μl was added into the well and incubated for 2 h at 37°C. After washing five times with PBS/Tween 20 buffer, anti-mouse IgG HRP F(ab’)2 fragment from sheep (Southern Biotechnology Associates, Inc., Birmingham, AL) (diluted 1:5,000 in 1% BSA) was added (50 μl/well) and incubated for 1 h at 37°C. The plates were washed five times with PBS/Tween 20 buffer. Finally, the samples were developed with 100 μl TMB substrate (BioRad) for 30 min at room temperature and then stopped with 100 μl of 2% (w/v) oxalic acid. The OD of each well was measured using an Ultramark BioRad Microplate Imaging System at 405 nm.
CTL assay and cytokine release from splenocytes
CTL activity was measured using CytoTox 96 NonRadioactive Cytotoxicity Assay Kit (Promega, Madison, WI). Mice were immunized subcutaneously on days 0 and 14 as mentioned above. On day 28, they were sacrificed, and splenocytes were prepared and cultured in RPMI medium with 10% FBS, 50 U/ml penicillin/streptomycin, 2 mM L-glutamine, 1 mM sodium pyruvate, 2 mM nonessential amino acids, 40 U/ml IL-2, and 1 μg/ml a nine amino acid E7 peptide (aa 49–57, RAHYNIVTF) for 4 days. Effector cells were plated into 96-well plates at various effector/target (E:T) ratios. Targets used were EL4 cells pulsed with E7 peptide. Before being mixed with effectors, the targets were washed two times with the medium and re-suspended at 2×105 cells/ml. The lysis reaction was carried out for 4 h at 37°C, after which the plates were centrifuged, and 100 μl of medium was carefully removed from each well and assayed for lactate dehydrogenase activity. Specific lysis was calculated with the absorbance at 490 nm as suggested by the manufacturer.
Also, splenocytes (1×106 cells in 300 μl, n=6) were stimulated with 10 μg/mL of E7 protein for 48 h. The cells were spun down, and the IL-4 and IFN-γ level in the supernatant was measured using ELISA kits from Pierce (Rockford, IL).
Statistical analysis
Except where mentioned, statistical analyses were completed by performing a one-way analysis of variance (ANOVA) followed by pair-wise comparisons with Fisher’s protected least significant difference procedure (PLSD). The tumor regression curves were analyzed using GraphPad Prism 3.0 (GraphPad Software Inc., San Diego, CA). A p value of ≤ to 0.05 (two-tail) was considered to be significant.
Results
LPD/E7 induced strong cellular and antibody immune responses in mice
The use of a single MHC class I-restricted peptide epitope, E749-57, did not allow us to fully characterize the immune responses induced by the LPD as a vaccine carrier and/or adjuvant in previous studies. In the present study, purified HPV 16 E7 protein was incorporated into the LPD particles and used to immunize mice. E7 protein should allow us to characterize both CTL and antibody responses. As expected, a strong CTL response was induced when mice were immunized with the LPD/E7 protein (Fig. 1a). The significantly enhanced IFN-γ release,but not that of IL-4, from splenocytes isolated from the LPD/E7 protein immunized mice indicates that the immune response is biased toward Th1 (Fig 1b). Immunization with the LPD/E7 protein induced a strong E7-specific antibody response too (Fig. 1c). The E7 specific IgG level in the serum of mice immunized with LPD/E7 protein was significantly higher than that from mice immunized with E7 protein admixed with Alum (Fig. 1c, P=0.017). In all these studies, very weak responses were induced when mice were immunized with the E7 protein alone.
LPD/E7 protein induced anti-E7 immune responses. Mice (n=4–5) were immunized with E7 protein alone (20 μg/mouse), LPD/E7 protein, or E7 protein adjuvanted with Alum (15 μg/mouse) (Alum/E7) on days 0 and 14. On day 28, they were bled via tail vein. Also, Spleens from mice in the same group were pooled, and splenocytes were prepared. All formulations were in 5% sterile dextrose. As a control, one group of mice was left untreated. a CTL response. Asterisk indicate that the values from every treatment are different from each other. Shown are mean ± S.D (n=3). The CTL result is a representative from three independent experiments. b Cytokine released from splenocytes after stimulation with E7 protein (10 μg/ml). Shown are concentrations averaged from six different readings (±S.D.). Double asterisk indicates the INF-γ from LPD/E7 immunized mice is significantly higher than that from the others. c Specific total IgG level in serum after diluted by 1,000-fold. A ANOVA analysis on the three treatments showed a P value of 0.001. Triple asterisk indicates that the value from LPD/E7 is significantly different from that of the others
Treatment with LPD/E7 led to complete regressions of tumors in mice
Because the LPD/E7 protein induced strong CTL and T helper cell responses (Fig. 1a, b), we expected the immune responses have anti-tumor activity. To test this, TC-1 tumor cells were subcutaneously seeded into mice, 4 days later, the mice were treated with the LPD/E7 protein. As shown in Fig. 2, treatment of tumor-bearing mice with the LPD/E7 caused complete regression of the tumors. In contrast, E7 protein alone or E7 protein admixed with Alum did not induce inhibitory effects on tumor growth. On day 25, the size of tumors in E7/Alum or mice treated with E7 alone were similar to that of the untreated mice (P=0.26).
Treatment with the LPD/E7 protein caused complete tumor regressions. Mice (n=5) were subcutaneously injected with TC-1 cells (5×105 /mouse) on day 0. On day 4, they were treated with E7 protein alone (20 μg/mouse), LPD/E7 protein, and E7 protein adjuvanted with Alum (15 μg/mouse) (Alum/E7). Shown is the tumor growth kinetics. On day 25, the tumor sizes in the LPD/E7 treated mice are significantly smaller than that from other treatments (P<<0.05). Standard deviations are only showed for day 25 for easy viewing. Only one representative of three independent experiments is shown. Filled triangle indicates the treatment time point
Construction of E7 mutant
Point mutations D21 to G21 and C94 to G94 were introduced into the E7 protein using overlapping PCR. DNA sequencing confirmed the mutations. It has been shown that replacing amino acid D21 on HPV 16 E7 gene protein by G21 deletes the cell transformation ability of the E7 protein [25, 72]. Also, disruption of the zinc finger structure in the C terminal of E7 protein by deleting one of the CXXC motifs significantly damages the oncogenic activity of E7 [73, 74]. Therefore, only an indirect method was used to confirm that the mutated E7 protein is unable to activate E2F-driven genes [24]. The wild type E7 protein can bind to pRB, causing the activation of E2F; whereas the mutant E7 protein created should not be able to do the same. When 293 cells were co-transfected with a luciferase gene driven by an E2F responsive element (cdc25A Sac I-luc) and an E7 protein encoding plasmid (pCDNA-E7), significantly higher luciferase expression was observed as compared with cdc25A Sac I-luc co-transfected with an empty plasmid (pCDNA3) (P=0.02) (Fig. 3). However, when pCDNA-E7m was co-transfected with cdc25A Sac I-luc, the resulting luciferase level was comparable to that of cdc25A Sac I-luc co-transfected with pCDNA3 (P=0.19). Taken together, the data were consistent with the notion that the mutations on E7 have removed its ability to bind to pRB and thus its oncogenic activity.
Relative luciferase unit (RLU) in 293 cells transfected with a CMV driven β-galactosidase gene containing plasmid, cdc25A Sac I-luc, and pCDNA3(+) with or without E7/E7m gene (see Materials and Methods for details). Asterisk indicates that the value for pCDNA-E7 is different from that of the others (P=0.002). Also, the value for pCDNA3 is not different from that for pCDNA-E7m (P=0.19). Data reported are mean ± S.D. (n=6). Experiment was repeated three times. Shown is one representative
LPD incorporated with the mutant E7 protein induced immune responses comparable to that induced by LPD incorporated with the wild-type E7 protein
To investigate whether the mutations introduced into the E7 protein affect its ability to induce anti-tumor and antibody responses, both recombinant E7 and E7m proteins were purified, incorporated into LPD, and used to immunize mice. The resulting specific antibody level and tumor therapy activity were compared. Shown in Fig. 4 are the specific IgG levels in serum on day 28 and day 60. Both LPD/E7 and LPD/E7m induced significantly higher IgG levels than E7 and E7m alone without LPD. Interestingly, on day 28, the IgG level from LPD/E7 was higher than that from LPD/E7m (P=0.019); whereas on day 60, the IgG level from LPD/E7 was comparable to that from LPD/E7m (P=0.53). This is due to the significantly decreased IgG level in LPD/E7 immunized mice on day 60 (P=0.004). It is possible that the antibody response from the mutated E7 protein lasted longer than that from the wild type E7 protein. The above data are the antibody levels when measured against the E7 protein. Similar results were obtained when they were measured against the E7m protein (data not shown).
Specific total IgG levels in mice immunized with E7m, LPD/E7m, E7, and LPD/E7. Mice (n=5–6) were immunized on days 0 and 14. Shown are IgG levels in serum on day 28 (open circle) and day 60 (open square). The IgG levels from E7 or E7m alone immunized mice were significantly lower than those from LPD/E7 or LPD/E7m immunized mice, respectively. On day 28, the value for LPD/E7m was lower than that for LPD/E7 (P = 0.02); on day 60, the values from these two treatments were similar (P=0.53). For LPD/E7m, the value from day 28 was similar to that for day 60 (P=0.81); for LPD/E7, these two values are different (P=0.004). The dark lines are the means (n=5–6).
Treatment of tumor bearing mice with LPD/E7m is as effective as with LPD/E7 in causing tumor regressions (Fig. 5). In addition, the LPD particles as an antigen carrier or adjuvant are more effective than the Montanide ISA-51 in treating tumors (Fig. 6). LPD/E7m treatment (once, 6 days after tumor inoculation) caused complete tumor regressions, whereas Montanide ISA-51/E7m did not induce significant anti-tumor activity (Fig. 6).
LPD/E7m and LPD/E7 are equally effective in treating tumor. Mice (n=5 or 10, 10 for LPD/E7 and LPD/E7m) were injected with TC-1 cells (5×105 /mouse) on day 0. On days 4 and 10, they were treated with E7 or E7m alone, LPD/E7 or LPD/E7m. The protein dose was 20 μg/mouse. Tumor sizes were reported as a function of time. Statistical analysis showed that the values for LPD/E7m and LPD/E7 are not different (Prism). Error bars are standard deviation. One representative of two independent experiments is shown. Filled triangles indicate the treatment time points
LPD/E7m induced stronger anti-tumor response than E7m incorporated into Montanide ISA-51. Mice (n=7) were injected with TC-1 cells (5×105 /mouse) on day 0. On day 6, they were treated with LPD/E7m or E7m incorporated into Montanide ISA-51. The protein dose was 20 μg/mouse. Tumor sizes were reported as a function of time. Error bars are standard deviation. Shown is one representative of two independent experiments. The filled triangle indicates the treatment time point
Discussion
We have shown that LPD as a protein antigen carrier and adjuvant induced strong and robust immune responses to eradicate established tumors in a mouse model. In fact, the anti-tumor activity from LPD as an antigen carrier and adjuvant is even stronger than that from the Montanide ISA-51, one of the Montanide series that have been used in many previous clinical trials as a vaccine adjuvant [52–64]. Considering the good toxicity profile of LPD in previous clinical trials [76], LPD has a great potential as a vaccine carrier and adjuvant. The HPV 16 E7 protein was used as an antigen to test the adjuvanticity of LPD. Although antibody response and Th2 cytokine release, such as IL-4, may not be required for the killing of cervical cancer cells, we still measured these aspects of immune responses to thoroughly understand the resulting immune response. To our surprise, both strong CTL and potent antibody responses have been induced. Thus, LPD may be readily used to prepare vaccines against HIV or malaria, for which both neutralizing antibody and CTL responses are required.
Another objective of the present study is to test the feasibility of using the HPV 16 E7 protein-incorporated LPD (LPD/E7 protein) as a therapeutic vaccine to treat cervical cancer. In three different dosing schedules [day 4 only (Fig. 2), days 4 and 10 (Fig. 5), and day 6 only (Fig. 6)], treatment with LPDs incorporated with either the wild-type or the mutant E7 protein always led to complete tumor regression in the end. Thus, we believe that our LPD particles incorporated with cervical cancer specific antigens (E6 and E7 from the “high risk” HPV types) could be a potent vaccine for cervical cancer therapy.
Only second to breast cancer, cervical cancer is prevalent among women worldwide. Evidence clearly points to ‘high risk’ HPV viruses as the causal agent of cervical cancer. In the U.S., the widespread use of the ‘Pap’ smear screening has resulted in a 70% decline in mortality from cervical cancers in the last five decades [77]. Unfortunately, it was estimated that 50% of cervical cancer in the US occurred in previously screened patients. Also, women in developing countries do not have easy access to this screening program [78]. Therefore, vaccination seems to be the most promising approach. Due to the almost universal presence of E6 and E7 proteins in cervical cancer cells, successful immune responses raised against E6 and/or E7 protein should theoretically kill the cervical cancer cells. In fact, many vaccines have been constructed based on partial or full length E6 and/or E7 in the form of protein, peptide, or DNA [79]. Our LPD particles, incorporated with the E7 protein, induced very strong CTL and anti-tumor responses. The Th1 response as indicated by the high IFN-γproduction may also be helpful. It is believed that the CD4+ T cell response is not required for tumor killing, but still beneficial [80]. In fact, our previous tumor prevention study showed that, after immunization with the LPD/E7 protein, about 40% of CD4+ cell-depleted mice developed tumors when challenged with TC-1 cells, in comparison to the fact that all the LPD/E7 protein immunized normal mice were tumor free (unpublished data). Montanide series are a group of oil/surfactant based adjuvants in which different surfactants are combined with either a non-metabolizable mineral oil, a metabolizable oil, or a mixture of the two [81]. The various Montanide ISA adjuvants are water-in-oil emulsions, oil-in-water emulsions, or water-in-oil-in-water emulsions. Different adjuvants accommodate different aqueous phase/oil phase ratios because of the variety of surfactant and oil combinations. The manufacturer mentioned that the performance of these adjuvants is similar to the incomplete Freund’s adjuvant (IFA) for antibody production; however the inflammatory response is usually less. ISA-51 is a W/O emulsion based on mineral oil and designed to enhance immune responses. It has already been assessed in various clinical trials (I/II/III) [81]. The data from the current study (Fig. 6) clearly demonstrated that our LPD particles induced a much stronger anti-tumor response than the ISA-51 did. In another study using Montanide ISA-51, we found that treatment of tumor-bearing mice with antigen-incorporated ISA-51 failed to induce a detectable CTL response (unpublished data). This may explain why treatment with the ISA-51/E7 protein failed to cause tumor regression in the present study. In our study, when the E7 solution and ISA-51 were mixed in a 1:2 ratio (v/v), a very viscous whitish suspension was formed, making it extremely difficult to inject. The suspension formed a solid mass in the injection site, which took many days to diffuse. We are not sure whether an alternative and improved E7 protein and ISA-51 combination will lead to improved performance.
In general, a protein alone as an antigen does not induce (or only weakly induces) an immune response. Therefore, an effective adjuvant is necessary. Unfortunately, upto the present, Alum still represents the only approved vaccine adjuvant for humans in the U.S. Alum is a weak adjuvant for inducing antibody response, and is even worse as a cell-mediated immune (CMI) response adjuvant. The strong antibody and CMI including CTL responses against E7 protein, when the E7 was dosed as a LPD/E7 protein, demonstrated the potential of LPD as a vaccine carrier and adjuvant. Previous data showed that as high as 17% of DCs in the popliteal lymph nodes picked up LPD particles when the LPDs were subcutaneously injected into mouse footpad [69]. LPD nanoparticles enter DCs via endocytosis (unpublished data). A protein as an antigen usually does not induce CTL response because it is taken up via the endosome/lysosome path, degraded inside them, and then presented to the MHC II molecules. Recent studies have shown that carrying a protein in certain particulates allows it to enter the cytoplasma directly. The protein will be processed by the proteosome, presented to the MHC I molecules, then induce a CTL response [82, 83]. The fact that the E7 protein incorporated into LPD was able to induce a CTL response might be explained similarly. For those E7 proteins that were delivered to DCs directly, some may be delivered into the cytoplasm, presented ‘endogenously’, and induce a CTL response; some may stay in the endosome and lysosome and induce antibody response [84]. As to the mechanism of immune induction by LPD as an adjuvant, our previous studies have shown that the empty plasmid DNA incorporated inside the liposomes and the cationic lipids (or liposomes) are both responsible and required for its full activity [85]. It is known that the bacterial plasmid DNA is a potent vaccine adjuvant because of its unmethylated CpG motifs [86]. Studies by us and others have also shown that certain cationic lipids, such as the DOTAP used to prepare liposomes in our studies, are immunostimulatory [87]. Treatment of DCs with DOTAP induced both CD80/CD86 expression on DCs surface and the release of proinflammatory cytokines such as TNF-α by DCs [85, 87]. LPD as a vaccine carrier and adjuvant has many advantages. (1) Incorporation of antigen in the aqueous core of liposomes prevents the antigen from enzymatic degradation; (2) Two components of the LPD, the plasmid DNA and the cationic liposomes, are both immunostimulatory; (3) The immune response from LPD is balanced, both humoral and cellular responses are induced; (4) The LPD is not complicated to prepare because the incorporation of protamine-condensed DNA into liposomes is a spontaneous process; (5) The safety profile of LPD has been established in a recent Phase I clinical trial [76].
It is known that the HPV 16 E7 protein is tumorigenic. However, the risk from E7 in protein form as a vaccine is much lower than that when the E7 is coded in plasmid DNA for immunization. More toxicity studies are needed to determine whether these mutations are needed for an E7 protein-based vaccine. If a mutated version of the E7 protein is proven to be necessary in the future, our LPD particles should also be effective in delivering the mutated proteins as long as the MHC I-restricted epitope(s) are not altered or deleted. As shown in present studies, when incorporated with the mutated E7 protein, LPD particles are still effective in inducing anti-TC-1 immune responses.
In summary, we report that LPD as a protein-based antigen carrier and adjuvant induces a very potent and robust immune response, including CTL and antibody responses. It may be used to treat diseases such as cervical cancer, when specific antigens such as E7 protein is incorporated inside. We are currently confirming the anti-tumor efficacy of the LPD/E7m in humanized mice.
References
Blattman JN, Greenberg PD (2004) Cancer immunotherapy: a treatment for the masses. Science 305:200–205
Hoerr I, Obst R, Rammensee HG, Jung G (2000) In vivo application of RNA leads to induction of specific cytotoxic T lymphocytes and antibodies. Eur J Immunol 30:1–7
Carralot JP, Probst J, Hoerr I, Scheel B, Teufel R, Jung G, Rammensee HG, Pascolo S (2004) Polarization of immunity induced by direct injection of naked sequence-stabilized mRNA vaccines. Cell Mol Life Sci 61:2418–2424
Berzofsky JA, Terabe M, Oh S, Belyakov IM, Ahlers JD, Janik JE, Morris JC (2004) Progress on new vaccine strategies for the immunotherapy and prevention of cancer. J Clin Invest 113:1515–1525
Renkvist N, Castelli C, Robbins PF, Parmiani G (2001) A listing of human tumor antigens recognized by T cells. Cancer Immunol Immunother 50:3–15
Novellino L, Castelli C, Parmiani G (2005) A listing of human tumor antigens recognized by T cells: March 2004 update. Cancer Immunol Immunother 54:187–207
Matsuda K, Tsunoda T, Tanaka H, Umano Y, Tanimura H, Nukaya I, Takesako K, Yamaue H (2004) Enhancement of cytotoxic T-lymphocyte responses in patients with gastrointestinal malignancies following vaccination with CEA peptide-pulsed dendritic cells. Cancer Immunol Immunother 53:609–616
Mayordomo JI, Loftus DJ, Sakamoto H, CM De Cesare, Appasamy PM, Lotze MT, Storkus WJ, Appella E, DeLeo AB (1996) Therapy of murine tumors with p53 wild-type and mutant sequence peptide-based vaccines. J Exp Med 183:1357–1365
Nestle FO, Alijagic S, Gilliet M, Sun Y, Grabbe S, Dummer R, Burg G, Schadendorf D (1998) Vaccination of melanoma patients with peptide- or tumor lysate-pulsed dendritic cells. Nat Med 4:328–332
Butch AW, Kelly KA, Munshi NC (2001) Dendritic cells derived from multiple myeloma patients efficiently internalize different classes of myeloma protein. Exp Hematol 29:85–92
Davis CB, Dikic I, Unutmaz D, Hill CM, Arthos J, Siani MA, Thompson DA, Schlessinger J, Littman DR (1997) Signal transduction due to HIV-1 envelope interactions with chemokine receptors CXCR4 or CCR5. J Exp Med 186:1793–1798
Goldman F, Crabtree J, Hollenback C, Koretzky G (1997) Sequestration of p56(lck) by gp120, a model for TCR desensitization. J Immunol 158:2017–2024
Brown K, Gao W, Alber S, Trichel A, M Murphey-Corb, Watkins SC, Gambotto A, Barratt-Boyes SM (2003) Adenovirus-transduced dendritic cells injected into skin or lymph node prime potent simian immunodeficiency virus-specific T cell immunity in monkeys. J Immunol 171:6875–6882
Granelli-Piperno A, Zhong L, Haslett P, Jacobson J, Steinman RM (2000) Dendritic cells, infected with vesicular stomatitis virus-pseudotyped HIV-1, present viral antigens to CD4+ and CD8+ T cells from HIV-1-infected individuals. J Immunol 165:6620–6626
Humrich J, Jenne L (2003) Viral vectors for dendritic cell-based immunotherapy. Curr Top Microbiol Immunol 276:241–259
Manickan E, Kanangat S, Rouse RJ, Yu Z, Rouse BT (1997) Enhancement of immune response to naked DNA vaccine by immunization with transfected dendritic cells. J Leukoc Biol 61:125–132
Sharma S, Miller PW, Stolina M, Zhu L, Huang M, Paul RW, Dubinett SM (1997) Multicomponent gene therapy vaccines for lung cancer: effective eradication of established murine tumors in vivo with interleukin-7/herpes simplex thymidine kinase-transduced autologous tumor and ex vivo activated dendritic cells. Gene Ther 4:1361–1370
Smith SG, Patel PM, Porte J, Selby PJ, Jackson AM (2001) Human dendritic cells genetically engineered to express a melanoma polyepitope DNA vaccine induce multiple cytotoxic T-cell responses. Clin Cancer Res 7:4253–4261
Franco EL, Schlecht NF, Saslow D (2003) The epidemiology of cervical cancer. Cancer J 9:348–359
de Villiers EM (1994) Human pathogenic papillomavirus types: an update. Curr Top Microbiol Immunol 186:1–12
Munger K, Howley PM (2002) Human papillomavirus immortalization and transformation functions. Virus Res 89:213–228
Villa LL (1997) Human papillomaviruses and cervical cancer. Adv Cancer Res 71:321–341
Scheffner M, Huibregtse JM, Vierstra RD, Howley PM (1993) The HPV-16 E6 and E6-AP complex functions as a ubiquitin-protein ligase in the ubiquitination of p53. Cell 75:495–505
Borysiewicz LK, Fiander A, Nimako M, Man S, Wilkinson GW, Westmoreland D, Evans AS, Adams M, Stacey SN, Boursnell ME et al (1996) A recombinant vaccinia virus encoding human papillomavirus types 16 and 18, E6 and E7 proteins as immunotherapy for cervical cancer. Lancet 347:1523–1527
Munger K, Phelps WC (1993) The human papillomavirus E7 protein as a transforming and transactivating factor. Biochim Biophys Acta 1155:111–123
Schiller JT, Lowy DR (2001) Papillomavirus-like particle based vaccines: cervical cancer and beyond. Expert Opin Biol Ther 1:571–581
Tobery TW, Smith JF, Kuklin N, Skulsky D, Ackerson C, Huang L, Chen L, Cook JC, McClements WL, Jansen KU (2003) Effect of vaccine delivery system on the induction of HPV16L1-specific humoral and cell-mediated immune responses in immunized rhesus macaques. Vaccine 21:1539–1547
Zhang LF, Zhou J, Chen S, Cai LL, Bao QY, Zheng FY, Lu JQ, Padmanabha J, Hengst K, Malcolm K et al (2000) HPV6b virus like particles are potent immunogens without adjuvant in man. Vaccine 18:1051–1058
Hagensee ME, Olson NH, Baker TS, Galloway DA (1994) Three-dimensional structure of vaccinia virus-produced human papillomavirus type 1 capsids. J Virol 68:4503–4505
Chen CH, Wang TL, Hung CF, Pardoll DM, Wu TC (2000) Boosting with recombinant vaccinia increases HPV-16 E7-specific T cell precursor frequencies of HPV-16 E7-expressing DNA vaccines. Vaccine 18:2015–2022
Chen LP, Thomas EK, Hu SL, Hellstrom I, Hellstrom KE (1991) Human papillomavirus type 16 nucleoprotein E7 is a tumor rejection antigen. Proc Natl Acad Sci U S A 88:110–114
Cassetti MC, McElhiney SP, Shahabi V, Pullen JK, IC Le Poole, Eiben GL, Smith LR, Kast WM (2004) Antitumor efficacy of Venezuelan equine encephalitis virus replicon particles encoding mutated HPV16 E6 and E7 genes. Vaccine 22:520–527
Chu NR, Wu HB, Wu T, Boux LJ, Siegel MI, Mizzen LA (2000) Immunotherapy of a human papillomavirus (HPV) type 16 E7-expressing tumour by administration of fusion protein comprising Mycobacterium bovis bacille Calmette-Guerin (BCG) hsp65 and HPV16 E7. Clin Exp Immunol 121:216–225
Daemen T, Regts J, Holtrop M, Wilschut J (2002) Immunization strategy against cervical cancer involving an alphavirus vector expressing high levels of a stable fusion protein of human papillomavirus 16 E6 and E7. Gene Ther 9:85–94
De Marco F, Hallez S, Brulet JM, Gesche F, Marzano P, Flamini S, Marcante ML, Venuti A (2003) DNA vaccines against HPV-16 E7-expressing tumour cells. Anticancer Res 23:1449–1454
Franconi R, Di Bonito P, Dibello F, Accardi L, Muller A, Cirilli A, Simeone P, Dona MG, Venuti A, Giorgi C (2002) Plant-derived human papillomavirus 16 E7 oncoprotein induces immune response and specific tumor protection. Cancer Res 62:3654–3658
Herd KA, Harvey T, Khromykh AA, Tindle RW (2004) Recombinant Kunjin virus replicon vaccines induce protective T-cell immunity against human papillomavirus 16 E7-expressing tumour. Virology 319:237–248
Kaufmann AM, Nieland J, Schinz M, Nonn M, Gabelsberger J, Meissner H, Muller RT, Jochmus I, Gissmann L, Schneider A et al (2001) HPV16 L1E7 chimeric virus-like particles induce specific HLA-restricted T cells in humans after in vitro vaccination. Int J Cancer 92:285–293
Lamikanra A, Pan ZK, Isaacs SN, Wu TC, Paterson Y (2001) Regression of established human papillomavirus type 16 (HPV-16) immortalized tumors in vivo by vaccinia viruses expressing different forms of HPV-16 E7 correlates with enhanced CD8(+) T-cell responses that home to the tumor site. J Virol 75:9654–9664
Li J, Sun Y, Garen A (2002) Immunization and immunotherapy for cancers involving infection by a human papillomavirus in a mouse model Epub 2002 Nov 21. Proc Natl Acad Sci U S A 99:16232–16236
Lin CW, Lee JY, Tsao YP, Shen CP, Lai HC, Chen SL (2002) Oral vaccination with recombinant Listeria monocytogenes expressing human papillomavirus type 16 E7 can cause tumor growth in mice to regress. Int J Cancer 102:629–637
Nonn M, Schinz M, Zumbach K, Pawlita M, Schneider A, Durst M, Kaufmann AM (2003) Dendritic cell-based tumor vaccine for cervical cancer I: in vitro stimulation with recombinant protein-pulsed dendritic cells induces specific T cells to HPV16 E7 or HPV18 E7 Epub 2003 Aug 2. J Cancer Res Clin Oncol 129:511–520
Osen W, Peiler T, Ohlschlager P, Caldeira S, Faath S, Michel N, Muller M, Tommasino M, Jochmus I, Gissmann L (2001) A DNA vaccine based on a shuffled E7 oncogene of the human papillomavirus type 16 (HPV 16) induces E7-specific cytotoxic T cells but lacks transforming activity. Vaccine 19:4276–4286
Ressing ME, Sette A, Brandt RM, Ruppert J, Wentworth PA, Hartman M, Oseroff C, Grey HM, Melief CJ, Kast WM (1995) Human CTL epitopes encoded by human papillomavirus type 16 E6 and E7 identified through in vivo and in vitro immunogenicity studies of HLA-A*0201-binding peptides. J Immunol 154:5934–5943
Tillman BW, Hayes TL, DeGruijl TD, Douglas JT, Curiel DT (2000) Adenoviral vectors targeted to CD40 enhance the efficacy of dendritic cell-based vaccination against human papillomavirus 16-induced tumor cells in a murine model. Cancer Res 60:5456–5463
Wu L, Goodwin EC, Naeger LK, Vigo E, Galaktionov K, Helin K, DiMaio D (2000) E2F-Rb complexes assemble and inhibit cdc25A transcription in cervical carcinoma cells following repression of human papillomavirus oncogene expression. Mol Cell Biol 20:7059–7067
Zhi H, Han L, Ren J, Tian H, Luo W, Liang Y, Ruan L (2002) [Construction of recombinant vaccinia virus co-expressing mutant E6 plus E7 proteins and detection of its immunogenicity and antitumor response]. Zhonghua Shi Yan He Lin Chuang Bing Du Xue Za Zhi 16:341–344
Ferrara A, Nonn M, Sehr P, Schreckenberger C, Pawlita M, Durst M, Schneider A, Kaufmann AM (2003) Dendritic cell-based tumor vaccine for cervical cancer II: results of a clinical pilot study in 15 individual patients. J Cancer Res Clin Oncol 129:521–530
Kaufmann AM, Stern PL, Rankin EM, Sommer H, Nuessler V, Schneider A, Adams M, Onon TS, Bauknecht T, Wagner U et al (2002) Safety and immunogenicity of TA-HPV, a recombinant vaccinia virus expressing modified human papillomavirus (HPV)-16 and HPV-18 E6 and E7 genes, in women with progressive cervical cancer. Clin Cancer Res 8:3676–3685
Muderspach L, Wilczynski S, Roman L, Bade L, Felix J, Small LA, Kast WM, Fascio G, Marty V, Weber J (2002) A phase I trial of a human papillomavirus (HPV) peptide vaccine for women with high-grade cervical and vulvar intraepithelial neoplasia who are HPV 16 positive. Clin Cancer Res 6:3406–3416
Steller MA, Gurski KJ, Murakami M, Daniel RW, Shah KV, Celis E, Sette A, Trimble EL, Park RC, Marincola FM (1998) Cell-mediated immunological responses in cervical and vaginal cancer patients immunized with a lipidated epitope of human papillomavirus type 16 E7. Clin Cancer Res 4:2103–2109
WJ van Driel, Ressing ME, Kenter GG, Brandt RM, Krul EJ, van Rossum AB, Schuuring E, Offringa R, Bauknecht T, A Tamm-Hermelink, et al (1999) Vaccination with HPV16 peptides of patients with advanced cervical carcinoma: clinical evaluation of a phase I-II trial. Eur J Cancer 35:946–952
Hersey P, Menzies SW, Coventry B, Nguyen T, Farrelly M, Collins S, Hirst D, Johnson H (2005) Phase I/II study of immunotherapy with T-cell peptide epitopes in patients with stage IV melanoma. Cancer Immunol Immunother 54:208–218
Garcia de la Fuente JN, Gutierrez-Martin CB, Ortega N, Rodriguez-Ferri EF, del Rio ML, Gonzalez OR, Salinas J (2004) Efficacy of different commercial and new inactivated vaccines against ovine enzootic abortion. Vet Microbiol 100:65–76
Kumar S, Jones TR, Oakley MS, Zheng H, Kuppusamy SP, Taye A, Krieg AM, Stowers AW, Kaslow DC, Hoffman SL (2004) CpG oligodeoxynucleotide and Montanide ISA 51 adjuvant combination enhanced the protective efficacy of a subunit malaria vaccine. Infect Immun 72:949–957
Slingluff CL Jr, Petroni GR, Yamshchikov GV, Barnd DL, Eastham S, Galavotti H, Patterson JW, Deacon DH, Hibbitts S, Teates D et al (2003) Clinical and immunologic results of a randomized phase II trial of vaccination using four melanoma peptides either administered in granulocyte-macrophage colony-stimulating factor in adjuvant or pulsed on dendritic cells. J Clin Oncol 21:4016–4026
Carr A, Rodriguez E, Mdel CA, Camacho R, Osorio M, Gabri M, Carrillo G, Valdes Z, Bebelagua Y, Perez R et al (2003) Immunotherapy of advanced breast cancer with a heterophilic ganglioside (NeuGcGM3) cancer vaccine. J Clin Oncol 21:1015–1021
Gonzalez G, Crombet T, Torres F, Catala M, Alfonso L, Osorio M, Neninger E, Garcia B, Mulet A, Perez R et al (2003) Epidermal growth factor-based cancer vaccine for non-small-cell lung cancer therapy. Ann Oncol 14:461–466
Patil PK, Bayry J, Ramakrishna C, Hugar B, Misra LD, Natarajan C (2002) Immune responses of goats against foot-and-mouth disease quadrivalent vaccine: comparison of double oil emulsion and aluminium hydroxide gel vaccines in eliciting immunity. Vaccine 20:2781–2789
Slingluff CL, Jr., Yamshchikov G, Neese P, Galavotti H, Eastham S, Engelhard VH, Kittlesen D, Deacon D, Hibbitts S, Grosh WW et al (2001) Phase I trial of a melanoma vaccine with gp100(280–288) peptide and tetanus helper peptide in adjuvant: immunologic and clinical outcomes. Clin Cancer Res 7:3012–3024
Toledo H, Baly A, Castro O, Resik S, Laferte J, Rolo F, Navea L, Lobaina L, Cruz O, Miguez J et al (2001) A phase I clinical trial of a multi-epitope polypeptide TAB9 combined with Montanide ISA 720 adjuvant in non-HIV-1 infected human volunteers. Vaccine 19:4328–4336
Yamshchikov GV, Barnd DL, Eastham S, Galavotti H, Patterson JW, Deacon DH, Teates D, Neese P, Grosh WW, Petroni G, et al (2001) Evaluation of peptide vaccine immunogenicity in draining lymph nodes and peripheral blood of melanoma patients. Int J Cancer 92:703–711
Pye D, Vandenberg KL, Dyer SL, Irving DO, Goss NH, Woodrow GC, Saul A, Alving CR, Richards RL, Ballou WR, et al (1997) Selection of an adjuvant for vaccination with the malaria antigen, MSA-2. Vaccine 15:1017–1023
Elliott SL, Pye S, Le T, Mateo L, Cox J, Macdonald L, Scalzo AA, Forbes CA, Suhrbier A (1999) Peptide based cytotoxic T-cell vaccines; delivery of multiple epitopes, help, memory and problems. Vaccine 17:2009–2019
Lee RJ, Huang L (1996) Folate-targeted, anionic liposome-entrapped polylysine-condensed DNA for tumor cell-specific gene transfer. J Biol Chem 271:8481–8487
Li S, Rizzo MA, Bhattacharya S, Huang L (1998) Characterization of cationic lipid-protamine-DNA (LPD) complexes for intravenous gene delivery. Gene Ther 5:930–937
Whitmore MM, Li S, Falo L Jr, Huang L (2001) Systemic administration of LPD prepared with CpG oligonucleotides inhibits the growth of established pulmonary metastases by stimulating innate and acquired antitumor immune responses. Cancer Immunol Immunother 50:503–514
Whitmore M, Li S, Huang L (1999) LPD lipopolyplex initiates a potent cytokine response and inhibits tumor growth. Gene Ther 6:1867–1875
Dileo J, Banerjee R, Whitmore M, Nayak JV, Falo LD Jr, Huang L (2003) Lipid-protamine-DNA-mediated antigen delivery to antigen-presenting cells results in enhanced anti-tumor immune responses. Mol Ther 7:640–648
Paschen A, Eichmuller S, Schadendorf D (2004) Identification of tumor antigens and T-cell epitopes, and its clinical application. Cancer Immunol Immunother 53:196–203
Heck DV, Yee CL, Howley PM, Munger K (1992) Efficiency of binding the retinoblastoma protein correlates with the transforming capacity of the E7 oncoproteins of the human papillomaviruses. Proc Natl Acad Sci U S A 89:4442–4446
Sang BC, Barbosa MS (1992) Single amino acid substitutions in “low-risk” human papillomavirus (HPV) type 6 E7 protein enhance features characteristic of the “high-risk” HPV E7 oncoproteins. Proc Natl Acad Sci U S A 89:8063–8067
Jewers RJ, Hildebrandt P, Ludlow JW, Kell B, McCance DJ (1992) Regions of human papillomavirus type 16 E7 oncoprotein required for immortalization of human keratinocytes. J Virol 66:1329–1335
Shi W, Bu P, Liu J, Polack A, Fisher S, Qiao L (1999) Human papillomavirus type 16 E7 DNA vaccine: mutation in the open reading frame of E7 enhances specific cytotoxic T-lymphocyte induction and antitumor activity. J Virol 73:7877–7881
Kim TY, Myoung HJ, Kim JH, Moon IS, Kim TG, Ahn WS, Sin JI (2002) Both E7 and CpG-oligodeoxynucleotide are required for protective immunity against challenge with human papillomavirus 16 (E6/E7) immortalized tumor cells: involvement of CD4+ and CD8+ T cells in protection. Cancer Res 62:7234–7240
Leone P, Janson CG, Bilaniuk L, Wang Z, Sorgi F, Huang L, Matalon R, Kaul R, Zeng Z, Freese A et al (2000) Aspartoacylase gene transfer to the mammalian central nervous system with therapeutic implications for Canavan disease. Ann Neurol 48:27–38
Kurman RJ, Henson DE, Herbst AL, Noller KL, Schiffman MH (1994) Interim guidelines for management of abnormal cervical cytology The 1992 National Cancer Institute Workshop. Jama 271:1866–1869
Crum CP (2002) The beginning of the end for cervical cancer? N Engl J Med 347:1703–1705
Eiben GL, da Silva DM, Fausch SC, Le Poole IC, Nishimura MI, Kast WM (2003) Cervical cancer vaccines: recent advances in HPV research. Viral Immunol 16:111–121
Hahn S, Gehri R, Erb P (1995) Mechanism and biological significance of CD4-mediated cytotoxicity. Immunol Rev 146:57–79
Aucouturier J, Dupuis L, Deville S, Ascarateil S, Ganne V (2002) Montanide ISA 720 and 51: a new generation of water in oil emulsions as adjuvants for human vaccines. Expert Rev Vaccines 1:111–118
Falo LD Jr, Kovacsovics-Bankowski M, Thompson K, Rock KL (1995) Targeting antigen into the phagocytic pathway in vivo induces protective tumour immunity. Nat Med 1:649–653
York IA, Rock KL (1996) Antigen processing and presentation by the class I major histocompatibility complex. Annu Rev Immunol 14:369–396
Blum JS, Ma C, Kovats S (1997) Antigen-presenting cells and the selection of immunodominant epitopes. Crit Rev Immunol 17:411–417
Cui Z, Han S-J, Vangasseri DP, Huang L (2005) Immnuostimulation mechanism of LPD nanoparticles as a vaccine carrier. Mol Pharmaceutics 2:22–28
Bauer S, Kirschning CJ, Hacker H, Redecke V, Hausmann S, Akira S, Wagner H, Lipford GB (2001) Human TLR9 confers responsiveness to bacterial DNA via species-specific CpG motif recognition. Proc Natl Acad Sci U S A 98:9237–9242
Heil F, Hemmi H, Hochrein H, Ampenberger F, Kirschning C, Akira S, Lipford G, Wagner H, Bauer S (2004) Species-specific recognition of single-stranded RNA via toll-like receptor 7 and 8. Science 303:1526–1529
Acknowledgment
This work was supported in part by NIH grants CA74918 and AI48851 to LH. The authors would like to thank Dr. Jeong-Im Sin from the Catholic University of Korea (Seoul, Korea) for the pET-E7 plasmid. ZRC would like to thank Jiang Li and Bin Sun for their help in plasmid molecular manipulation.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Cui, Z., Huang, L. Liposome-polycation-DNA (LPD) particle as a carrier and adjuvant for protein-based vaccines: Therapeutic effect against cervical cancer. Cancer Immunol Immunother 54, 1180–1190 (2005). https://doi.org/10.1007/s00262-005-0685-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-005-0685-2