Abstract
Purpose: In addition to its use as a blood marker for many carcinomas, elevated expression of carcinoembryonic antigen (CEA, CD66e, CEACAM5) has been implicated in various biological aspects of neoplasia, especially tumor cell adhesion, metastasis, the blocking of cellular immune mechanisms, and having antiapoptosis functions. However, it is not known if treatment with anti-CEA antibodies can affect tumor metastasis or alter the effects of cytotoxic drugs. Methods: In vitro, human colon cancer cell lines were treated with anti-CEA MAb IgG1, hMN-14 (labetuzumab), to assess direct effects on proliferation, as well as antibody-dependent cellular cytotoxicity (ADCC), and complement-dependent cytotoxicity (CDC). In vivo studies were undertaken in nude mice bearing s.c. (local growth) or i.v. (metastatic model) GW-39 and LS174T human colon cancer grafts, to evaluate the MAb alone and in combination with either CPT-11 or 5-fluorouracil (5FU). Results: In vitro, labetuzumab did not induce apoptosis, nor did it affect tumor cell proliferation directly or by CDC, but it did inhibit tumor cell proliferation by ADCC. In vivo, labetuzumab did not increase median survival in the GW-39 metastatic model unless the mice were pretreated with GM-CSF to increase their peripheral WBC counts; GM-CSF alone was ineffective. Also, if GW-39 tumors were pretreated with IFN-γ to up-regulate CEA expression threefold prior to i.v. injection, labetuzumab significantly increased median survival of the mice. When nude mice received labetuzumab with CPT-11 or 5FU, median survival increased significantly as compared to the drug or antibody alone. Conclusions: Labetuzumab, a CEA-specific MAb, induces effector-cell function in vitro against CEA-positive colonic tumor cells, and also inhibits growth of lung metastasis when CEA expression is up-regulated or if peripheral WBCs are increased. The MAb also shows chemosensitizing properties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several antibodies have emerged as effective cancer therapeutics, either by affecting the signaling function of their receptor targets, inducing apoptosis or cell-cycle phase disruption, evoking host immune responses, enhancing chemosensitivity or radiosensitivity, or a combination of these factors. Examples include antibodies to CD20 in non-Hodgkin’s lymphoma [18, 65], and to GA733-2 or EpCAM [2, 75], EGFR [52, 72], and HER-2/neu [61, 94] in certain solid tumors. The introduction and acceptance of such biological therapies has stimulated an intensive search for other suitable targets for antibody-mediated cancer therapy.
One such candidate target is carcinoembryonic antigen, or CEA (also known as CD66e or CEACAM5) [6, 34], which was first described in 1965 as a gastrointestinal oncofetal antigen [22], but is now known to be overexpressed in a majority of carcinomas, including those of the gastrointestinal tract, the respiratory and genitourinary systems, and of the breast [23, 27, 33, 93, 101].
The CEA gene family is present in two defined clusters on chromosome 19, between 19q13.1 and 19q13.3, represented by 29 gene-like sequences, and is considered to be a subset of the immunoglobulin gene superfamily, with analogous variable and constant regions [34, 78]. CEA is anchored in the cell membrane via a glycosyl phosphatidyl inositol moiety [38], showing temperature- and Ca2+-independence typical of classical intercellular adhesion receptors. Further, CEA has been shown to be involved in both homophilic (CEA to CEA) and heterophilic (CEA binding to non-CEA molecules) binding [7, 79, 97], suggesting to some that it is an intercellular adhesion molecule involved in cancer invasion and metastasis [47, 110].
Alternatively, it has been proposed that CEA acts as a signal-transducing protein that repulses cellular contact and increases tumor cell mobility, thus inducing cell migration and metastasis [31, 105]. Supporting this notion is the finding that after transplantation of colorectal tumors into nude mice, the number of liver metastases increased from 2% to 48% following injection of CEA to the mice [41]; however, others have disputed the role of blood CEA in this setting [60]. It has also been reported that CEA overexpression can protect tumor cells from undergoing anoikis, or apoptosis from loss of cell contact with the extracellular matrix [80]. Still other studies have shown that CEA affects expression of various groups of cancer-related genes, especially cell cycle and apoptotic genes, protecting colonic tumor cells from various apoptotic stimuli, such as treatment with 5-fluorouracil (5FU) [95]. Therefore, CEA expression may be a means for cancer cells to overcome apoptosis-inducing therapies. Conversely, inhibition of, or binding to, CEA may result in antitumor effects or even enhance other apoptosis-mediated therapeutic interventions, such as with typical anticancer drugs, or the activation of proapoptotic pathways, as has been proposed for epidermal growth factor receptor (EGFR) antagonists [72]. Thus, after almost 4 decades of research involving CEA, its biological function is still the subject of considerable investigation and debate. In this article, we demonstrate for the first time that CEA-binding antibodies exert antimetastatic effects in vivo in appropriate settings of CEA expression, and also have chemosensitizing properties.
Materials and methods
Antibody
The MN-14 antibody is a second-generation murine MAb with tenfold higher affinity than the first generation NP-4 antibody [35], directed against a CEA-specific (CEACAM5 or CD66e), class III epitope according to Primus et al. [83], and shown subsequently [64] to bind to the A3B3 domain of Gold epitope group 3 of CEA [8]. The CDR-grafted (humanized) MN-14 anti-CEA IgG1, hMN-14 or labetuzumab [89], along with the murine MN-14 MAb [35], both supplied by Immunomedics (Morris Plains, NJ, USA), were purified by protein A and ion-exchange chromatography (Q-Sepharose; Pharmacia, Piscataway, NJ, USA). Purity was tested by immunoelectrophoresis, polyacrylamide gel electrophoresis using reducing and nonreducing conditions and size-exclusion high-pressure liquid chromatography. Previous studies have shown that the biodistribution, tumor targeting and pharmacokinetic behavior of labetuzumab was similar to that of murine MN-14 in nude mice [88, 89]. The F(ab)2 fragment was prepared by pepsin digestion of the intact IgG, followed by passage over a protein A column. The control hA20 anti-CD20 humanized IgG1 MAb [98] was provided by Immunomedics.
CEA expression in cell lines
Expression of CEA was assayed in a labetuzumab cell-binding ELISA assay. One hundred thousand cells were added in growth media to wells of a 96-well microtiter plate. Labetuzumab and an isotype-matched negative control, anti-CD20 humanized MAb [98], were diluted in growth media and added to the cells in triplicate at a final concentration of either 1 or 5 μg/ml. After incubation for 1 h the cells were washed by centrifugation of plates. Secondary antibody, HRP-goat antihuman IgG, Fc-specific, was added, and plates were incubated for 1 h at either 4°C or room temperature. The plates were washed as before, with a final wash in PBS. Bound antibody was detected with a luminescent HRP substrate (LumiGlo; KPL, Gaithersburg, MD, USA). The plates were read in an EnVision plate reader (PerkinElmer, Boston, MA, USA), using a luminescence protocol. Cell lines which gave values that were three times the negative controls were considered to be positive.
Peripheral WBC determination
In some studies, mice were given 1 μg/day × 4 days i.p. of recombinant murine granulocyte-macrophage colony-stimulating growth factor (GM-CSF) (Immunex, Seattle, WA, USA). Immediately after the last treatment with GM-CSF and prior to initiation of labetuzumab therapy, 50 μl of heparinized blood was collected retro-orbitally. Red blood cells were lysed and white blood cells were counted on a Becton Dickinson FACScan as described previously [11].
CEA immunohistochemistry
GW-39sc tumors were removed from nude mice and fixed with buffered formalin. Paraffin-embedded tumor samples were cut into 5.0-μm sections. Tumor sections were deparaffinized, rehydrated, blocked, and exposed to 10 μg/ml of murine anti-CEA MAb or an irrelevant control murine antibody (Ag-8, raised against murine myelogranulocytic leukemia) as previously described [10]. After incubation for 45 min, slides were washed in PBS, and biotinylated goat antimouse secondary antibody applied for 30 min, using the Vectastain ABC Kit (Vector Labs, Burlingame, CA, USA). Endogenous peroxidase was destroyed by flooding the slides with 0.3% H2O2 in methanol. Slides were then incubated with 25 μl of avidin–horseradish peroxidase (HRP) conjugate (ABC) under humid conditions for 45 min. Excess ABC was washed off, and the sections were finally covered with 100 μl of HRP substrate, 3,3′-diaminobenzidine tetrahydrochloride solution (Sigma; 100 μg/ml diaminobenzidine in 0.1 M sodium acetate buffer, pH 6.0, with 0.01% [v/v] H2O2 for 15 min). Slides were then counterstained briefly with hematoxylin.
Antibody-dependent cellular cytotoxicity (ADCC) assay
The ADCC activity was determined by an LDH release assay. Tumor cell lines were obtained from the American Type Culture Collection (Rockville, MD, USA). Effector cells were PBMCs obtained from a healthy donor on the day of the experiment, using Lymphoprep lymphocyte separation medium (Accurate Chemical Co., Westbury, NY, USA). Effector cells were resuspended in assay medium (RPMI 1640 medium, 1% fetal bovine serum, penicillin [100 U/ml], streptomycin [100 μg/ml]). Target cells were detached from flasks by trypsin-EDTA, washed with assay media, and incubated with antibodies at 1 μg/ml for 40 min at 37°C in 96-well microtiter plates. Effector cells were added to the wells, and after 4 h, LDH release was assayed according to the manufacturer’s protocol (CytoTox One Homogeneous membrane integrity assay; Promega, Madison, WI, USA). The average absorbance of triplicate determinations was used to calculate the percentage cytotoxicity, calculated as:
% cytotoxicity = (experimental-targetspontaneous − effectorspontaneous) / (target maximum − targetspontaneous). All statistical analyses were done by Student’s t test.
Complement-dependent cytotoxicity (CDC) assay
The CDC assay was performed using CEA-positive (LS-174T, LoVo, CaPan-1) and CEA-negative cell lines (HT-29, MCF 7, Calu3, Daudi), and human complement (Quidel, San Diego, CA, USA). Antibodies were diluted in the assay medium (RPMI 1640, 0.1% BSA, penicillin [100 U/ml], streptomycin [100 μg/ml]) to 1 μg/ml final concentration. Cells were resuspended in media and added to 96-well microtiter plates, and antibodies and complement were added and incubated for 2 h. Cell viability was assayed by the addition of C12-resazurin (Molecular Probes, Eugene, OR, USA) to 5 μM. After 5 h, the plates were read in an EnVision plate reader (PerkinElmer) at Ex544 and Em590. Dose–response curves were generated from the mean of triplicate determinations, and statistical analyses were performed by Student’s t test.
CD55 and CD59 expression in cell lines
Expression of CD55 and CD59 was measured in a cell-binding ELISA assay. The assay was similar to that described for CEA expression with the following modifications. Phycoerythrin-labeled anti-CD55, anti-CD59 (BD Biosciences, Pharmingen, San Diego, CA, USA), or an isotype-matched negative control, murine IgG (Immunotech, Marseilles, France), were used at a final concentration of 5 μg/ml. The cells were incubated on ice for 1 h and washed. Bound antibody was detected by reading in an EnVision fluorescence plate reader at Ex480 nm and Em570 nm. Cell lines giving values that were three times the negative control were considered to be positive.
Proliferation assay
Cells were plated into 96-well microtiter plates at 10,000 cells per well, containing RPMI 1640 medium with 10% fetal bovine serum, penicillin (100 U/ml) and streptomycin (100 μg/ml). After 24 h, serial dilutions of antibodies (0.039–10 μg/ml) in complete growth media were added. A crosslinking antibody, goat antihuman IgG, Fc-specific (Jackson Immunoresearch, West Grove, PA, USA) was added at 20 μg/ml. After 4 days, proliferation was assessed in a multiplex metabolic assay (CellTiter Aqueous96; Promega, USA) and a DNA synthesis assay (BRDU ELISA; Roche Applied Sciences, Indianapolis, IN, USA), according to the manufacturers’ protocols. Dose–response curves were generated from the mean of triplicate determinations, and statistics performed by Student’s t test.
In vivo therapy studies
Female athymic nude mice (6–8 weeks old) were purchased from Taconic (Germantown, NY, USA). Survival therapy studies were performed using our CEA-positive GW-39 intrapulmonary micrometastasis model (GW-39iv; [9, 26, 89]). The GW-39 tumor has been maintained as a serially transplanted signet-ring cell human colon carcinoma line since 1966 [26], and expresses ~160 μg CEA/g tissue [25]. Subcutaneous GW-39 human colorectal tumors grown in nude mice were used to prepare a 10% or 5% cell suspension. Cells (30 μl) were injected i.v. into the caudal vein of 5- to 6-week-old female nude mice (Taconic). This model results in approximately 50–100 nodules developing in the lungs with resulting median survival of 7–9 weeks [9, 87]. For studies to assess the effect of higher neutrophil counts on anti-CEA Ab therapy effects, GM-CSF (1 μg/day × 4 days) was given i.p. to mice on days −4 through −1. GW-39 cells (30 μl of a 5% suspension) were introduced i.v., and hMN-14 treatments were initiated the same day (100 μg/day × 14 days and twice weekly for the duration of the study). Labetuzumab was initiated on either day 0 or day 3 after cell implantation, and administered once daily for 14 days and twice weekly thereafter for the duration of the study at a dose of 100 μg/day. CPT-11 (Camptosar, Florida Infusion, Palm Harbor, FL, USA) was administered i.p. at a dose of 80–160 μg daily for 5 days (10–20% of the MTD based on established doses in the literature [59]), starting on day 0 or day 3 after cell implantation. 5-Fluorouracil (5-FU; Sigma, St Louis, MO, USA) was given at an i.p. dose of 0.4 mg/day × 5 days (100% of the MTD). For some studies, the GW-39 tumor used for the transplant inoculum came from mice that received 100,000 U of IFN-γ (Florida Infusion) twice daily for 4 days to up-regulate CEA expression, as described earlier [30]. Body weight was monitored weekly and animal survival recorded. Results were analyzed by the Kaplan-Meier estimated survival curves, and significance was determined with the log-rank comparison of survival curves. Median survival time for each treatment group was also determined. For bulky disease studies, GW-39sc (10% tumor cell suspension in 200 μl derived from GW-39 tumors) or LS174Tsc (1e7 cells) was implanted s.c. in nude mice. After 2.5 weeks, when tumor size reached ~0.3 cm3, treatment was initiated. Tumor size was determined weekly by the product of 3 diameters determined by caliper measurements, and change in tumor size was calculated. The percentage growth inhibition (%GI) at 21 days posttreatment was determined: % GI = [(tumor size of untreated group − tumor size of treated group) / (tumor size of untreated tumor group)]×100%. All studies utilized ten mice per treatment group. Animal studies were performed under protocols approved by the Institutional Animal Care and Use Committee.
Results
CEA expression in cell lines
The CEA expression in cell lines was determined in a labetuzumab cell-binding ELISA. The colon cancer cell lines, LS-174T and LoVo, were positive, as was the pancreatic cancer cell line, CaPan-1. HT-29 was classified as CEA-negative in this assay, since binding with labetuzumab was not observed under the conditions tested.
ADCC activity of labetuzumab
Labetuzumab’s potential to mediate killing of tumor cell lines was investigated using PMBCs as effector cells. Labetuzumab was able to induce ADCC activity in both CEA-expressing colon cancer cell lines, LS174T and LoVo, and a CEA-expressing pancreatic tumor cell line, CaPan-1 (Fig. 1). The percentage lysis was significantly different from an isotype-matched negative control, anti-CD20 MAb, hA20 [37]. No ADCC activity was observed on CEA-negative tumor cell lines, HT-29, Calu3, SKOV4, MCF-7, and Daudi, to which labetuzumab failed to bind.
ADCC on CEA-positive tumor cell lines. Cells were incubated with labetuzumab (hMN-14) and hA20 (control anti-CD20 humanized MAb) in the presence of human peripheral blood mononuclear cells. The cells were incubated for 4 h at 37°C. After 4 h, LDH release was assayed by a homogeneous fluorometric assay. Error bars represent standard deviations. P values were determined by Student’s t test
CDC activity of labetuzumab
The ability of labetuzumab to mediate complement-dependent lysis was investigated in vitro using human complement. A panel of cell lines was tested, including both CEA-positive and CEA-negative cell lines. No CDC activity induced by labetuzumab was found in any cell lines tested, LS-174T, LoVo, and CaPan-1, but in a positive control, CDC activity was confirmed by treating CD20-positive lymphoma cells with anti-CD20 IgG1 MAb [98]. The expression of the complement inhibitory receptors CD55 and CD59 was assayed on the tumor cell lines used in the CDC assay. All CEA-positive tumor cell lines expressed high levels of CD55 and CD59 compared with the low levels of CD55 and CD59 of the CDC-sensitive Daudi lymphoma cell line (Fig. 2).
Direct effects of labetuzumab on tumor cell growth
No induction of apoptosis was effected by labetuzumab in the absence of effector cells in a 4-h ADCC assay. The direct effect of labetuzumab on tumor cell line growth was investigated in a proliferation assay. Proliferation was assessed both by a metabolic assay, which is proportional to the number of viable cells, and by a BrdU-incorporation assay, which measures cellular DNA synthesis. CEA-positive (LS-174T) and CEA-negative (HT-29) colon cancer cell lines were incubated with labetuzumab in the presence or absence of a cross-linking antibody, goat antihuman IgG, Fc-specific, for 4 days. An isotype-matched negative control antibody, hA20, also was included. There was no difference in the proliferation of any of the cell lines in the presence of labetuzumab, with or without a cross-linking antibody, compared with the negative control antibody (data not shown).
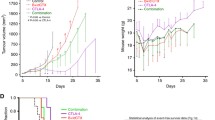
Effects of labetuzumab alone or in GM-CSF–pretreated mice
The ability of labetuzumab to increase survival of GW-39iv mice under baseline conditions and with increased numbers of effector cells was also evaluated. A 4-day pretreatment of nude mice with rM-GM-CSF (1 μg/day) resulted in 4.5- to 5.0-fold increases in total pWBCs (P<0.001; Fig. 3, top panel). A comparison of therapeutic effects of labetuzumab in mice with baseline pWBCs versus mice with GM-CSF–up-regulated pWBC levels is shown in Fig. 3 (bottom panel). GM-CSF treatment alone did not affect survival, nor did repeated dosing with labetuzumab. However, the median survival in the labetuzumab-treated group (7.5 weeks) was increased by 42.7–10.7 weeks in those mice with higher pWBC counts resulting from GM-CSF treatment (T=9.858, P<0.005).
Effects of GM-CSF on labetuzumab (hMN-14) therapy in the GW-39 intrapulmonary micrometastasis model. GM-CSF (1 μg/day × 4 days) was given i.p. to mice on days −4 through −1, blood was collected on day 0 of the study, and pWBCs were enumerated by flow cytometry. The mean ± SD of each treatment (N=10) was recorded. GW-39 cells (30 μl of a 5% suspension) were introduced i.v., and hMN-14 treatments were initiated the same day (100 μg/day × 14 days and twice weekly for the duration of the study. Survival of mice was monitored
Role of CEA expression on the therapeutic effects of labetuzumab
We postulated that the amount of tumor CEA expressed might influence the ability of naked anti-CEA antibody therapy. Stock tumors derived from the s.c. models and then used to establish the GW-39iv model have a heterogeneous CEA expression (160 μg CEA/g tumor by ELISA; [39]), while s.c. tumors derived from mice given a 4-day treatment with IFN-γ have much higher and more homogeneous CEA expression (Fig. 4, top panels) that remains ~3-fold elevated for 10–13 days after the 4-day dosing regimen with IFN-γ (data not shown). When low CEA–expressing tumors were used to establish the GW-39iv model, labetuzumab did not affect group survival (T=0.417; P<0.9; Fig. 4, lower left panel). In contrast, when IFN-γ–treated tumors with up-regulated CEA expression were used to establish the same model, labetuzumab did improve median survival of mice bearing GW-39iv lung nodules from 10 to 12 weeks (T=5.598; P<0.025; Fig. 4, lower right panel). In contrast, IFN-γ–pretreated tumors without antibody treatment did not show in vivo survival extensions comparable to those subsequently given labetuzumab, indicating that interferon alone does not account for the antimetastatic effects observed with labetuzumab therapy. From the outcome of these two studies, we conclude that although labetuzumab has limited activity in this relatively low CEA–expressing tumor model, it becomes effective when either the number of effector cells or the amount of target antigen in the tumor is increased.
Up-regulation of GW-39 CEA expression and therapeutic effects of labetuzumab. Mice bearing stock GW-39 tumors were either left untreated or treated with IFN-γ (100,000 IU 2×/day × 4 days). Tumor was removed and an aliquot was placed into formalin for immunohistochemistry to measure CEA expression. The remainder was used to prepare a 5% cell suspension that was introduced i.v. into mice. Treatment with labetuzumab (hMN-14) was initiated the same day and survival of mice was monitored in each treatment group (N=10)
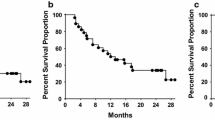
In vivo chemosensitization by labetuzumab
In addition to direct antitumor effects, labetuzumab was found to augment the antigrowth activity of two anticancer drugs applied in these models. Figure 5 shows survival curves for the GW-39iv model left untreated, treated with labetuzumab alone, CPT-11 alone, or the combination of antibody and drug, both initiated on the same day. Under baseline conditions (normal pWBC counts and low CEA expression), labetuzumab did not alter animal survival. Low-dose CPT-11 (10% MTD) increased median survival by 1.4 weeks from 6.8 to 8.2 weeks (P<0.05), whereas CPT-11 + labetuzumab extended median survival to 10.4 weeks (T=8.02; P<0.005 compared with CPT-11 group; and T=9.879; P<0.005 compared with untreated mice).
Therapeutic effects of labetuzumab (hMN-14) together with CPT-11 in the GW-39 lung micrometastasis model. The tumor model was initiated with 30 μl of a 10% GW-39 cell suspension. Groups of ten mice were either left untreated, treated with labetuzumab (hMN-14 IgG;100 μg/day × 14 days and twice weekly thereafter starting on day 1), CPT-11 (10% of the MTD or 80 μg/day × 5 days on days 1–5), or the combination of labetuzumab + CPT-11. Survival was monitored weekly
Since maximal antibody accretion occurs 3 days post injection, we questioned whether initiating labetuzumab treatments 3 days before CPT-11 dosing would further enhance the therapeutic effect of the combined modality treatment by allowing high antibody uptake and chemosensitization in vivo. Figure 6 demonstrates that the 3-day pretreatment with labetuzumab followed by CPT-11 increased median survival by 51.1–14.2 weeks (T=12.22; P<0.001 compared with labetuzumab + CPT-11 initiated together or CPT-11 initiated on day 0 and labetuzumab initiated on day 3, both with a median survival of 9.4 weeks).
Comparison of survival of mice bearing the GW-39 lung micrometastasis model (10% suspension) left untreated, or given labetuzumab (hMN-14) and CPT-11 (5 days schedule at 10% of the MTD) when both are started on day 0, or CPT-11 is started on day 0 and labetuzumab is started on day 3, or when labetuzumab is started on day 0 and CPT-11 is started on day 3
The chemosensitizing effect of hMN-14 IgG was not observed in the absence of the Fc portion of the antibody, if the labetuzumab bivalent F(ab)2 fragment was used in combination with CPT-11 (Fig. 7). Median survival of CPT-11–treated mice in this study was 11.0 weeks; labetuzumab + CPT-11, 13.5 weeks; and labetuzumab F(ab)2 + CPT-11, 9.3 weeks. The drug-augmenting effect was also absent if a nonspecific intact IgG (Ag8) was used in combination with CPT-11 (data not shown).
Survival curves for mice bearing GW-39 intrapulmonary micrometastases and left untreated or treated with labetuzumab (hMN-14) alone or labetuzumab F(ab)2 alone (100 μg/day × 14 days and twice weekly for the duration of the study), a 20% MTD of CPT-11 (160 μg/day × 5 days) alone, the IgG and CPT-11, or the F(ab)2 and CPT-11 together. Antibody treatment was initiated the day of cell implantation (30 μl of a 10% cell suspension) and CPT-11 was started on day 3
5-Fluorouracil, another commonly used chemotherapeutic in the management of colorectal cancer, also was evaluated in combination with labetuzumab. In the GW-39 xenograft model, this drug is much less efficacious than CPT-11, as evidenced by the need to use a 100% MTD of 5FU to observe any effect on survival, compared with the 10% MTD of CPT-11 which typically resulted in a 20% increase in survival. Labetuzumab was able to increase the efficacy of 5FU (T=4.376; P<0.05; Fig. 8), improving median survival from 7.4 weeks in the 5FU-treated group to 9 weeks in the 5FU + labetuzumab–treated group.
Survival of mice with GW-39 intrapulmonary micrometastases left untreated or treated with labetuzumab (hMN-14; 100 μg/day × 14 days and twice weekly for the duration of the study), or drug alone (5FU; 100% of the MTD or 400 μg/day × 5 days) or a combination of labetuzumab starting on day 0 and drug starting on day 3. Each treatment group started with ten mice
In the final experiments, we evaluated whether labetuzumab could also enhance the effect of CPT-11 in bulky s.c. GW-39 xenografts, as it does for micrometastatic disease in the GW-39iv model, and in a second human colonic s.c. xenograft using LS174T tumors. Figure 9 (upper panel) demonstrates that the percentage growth inhibition (%GI) of labetuzumab + CPT-11 was 51.8% on day 21 post treatment, compared with CPT-11–treated mice (29.7%) or labetuzumab-treated mice (0%). Similarly, the results with the LS174T model (Fig. 9, lower panel) shows that %GI for labetuzumab + CPT-11 was 67.2% on day 28 post treatment, compared with CPT-11–treated mice (28.9%) or labetuzumab-treated mice (0%). Thus, the chemosensitizing effect of labetuzumab occurs for both minimal, disseminated disease and larger, established, s.c. tumor models.
Growth curves for GW-39 tumors (upper panel) and LS-174T tumors (lower panel) grown s.c. in nude mice. Mice were left untreated, or treated with labetuzumab (hMN-14), CPT-11 (20% MTD), or the combination with antibody initiated 3 days before the 5-day course of CPT-11. Initial tumor size was ~0.3 cm3 at the time treatment began. The mean ± SD of the change in tumor size from day 0 in each treatment group (N=10) is shown
Discussion
These investigations contribute several new findings regarding CEA function and the possible role of CEA antibodies in the control of cancer dissemination and the enhancement of chemotherapy. The observation that a specific CEA antibody, targeting the A3B3 (CD66e) epitope [64] that is not shared with other CEA-family members [6, 34], inhibits human colonic cancer spread to the lungs and mortality in nude mice is the first direct support of earlier in vitro studies suggesting a role of CEA in cancer spread and metastasis by pretreating of CEA-expressing metastatic colonic cancer cells with anti-CEA antibody in vitro and then showing a reduction of metastasis in vivo [53]. However, our findings appear to contradict recent experiments on adhesion and differentiation-inhibitory activities of CEA, which indicated that monovalent Fab fragments could reverse tumorigenic effects whereas divalent antibodies, as used in our studies, would be expected to increase the tumorigenic effects of CEA [99].
The alteration of CEA-expressing colonic cancer spread and lethality in a xenograft model by a CEA-specific antibody is supportive of the general view of the role of CEA in tumor biology, despite the mechanisms related thereto still being in dispute. Studies with in vitro and in vivo cell lines, as well as clinical observations, support the view that high CEA production is directly related to malignancy, particularly enhanced metastasis [28, 41, 42, 46–50, 54, 73, 74, 100, 102, 106, 107, 110]. CEA was found to function as an intercellular adhesion molecule promoting cell aggregation by homotypic interactions, because cells transfected with cDNA for CEA formed aggregates, and this aggregation was completely inhibited by CEA antibody treatment of the cells in vitro [7, 79]. The transfectants could have their ability to form liver metastases after splenic injection inhibited by in vitro treatment with CEA antibody [36, 37]. In another line of experimentation, CEA has been found to block cellular differentiation [16], it had tumorigenic effects alone and in combination with other oncogenes [85], and deregulated CEA expression in human colonocyte lines disrupted cell polarization, tissue architecture, and increased tumorigenicity [43].
These past observations on the various mechanisms of CEA are supported by the finding that anti-CEA antibody treatment of CEA-expressing tumor cells can inhibit the homotypic binding in vitro and also the size and number of hepatic metastases [110]. Further, this group found that anti-CEA antibody did not influence tumor cell growth in vitro or the incidence of hepatic metastases or splenic weight, which suggested to them that complement-mediated or antibody-dependent cell-mediated cytotoxicity was not involved by pretreatment of the cells with anti-CEA antibody in vitro, and concluded that the increased metastatic potential to the liver is related to the increased homotypic binding through CEA [110]. However, some CEA MAbs have been reported to have complement-mediated cytotoxicity against tumor cells in vitro [45], contrary to our own experience herein with the GW-39 tumor model, and supported by the high levels measured for the complement regulatory factors, CD55 and CD59, which are known to inhibit complement-mediated cytotoxicity [21, 40]. These authors also found that their fully human CEA MAb inhibited colon tumor growth in vivo [45], thus agreeing with the results reported here. Using effusion samples from patients with colorectal cancer, it has also been demonstrated that degree of aggregation correlated with CEA expression, and that in vitro, aggregation was completely inhibited by anti-CEA antibody, supporting the notion that CEA on the tumor cell surface mediated this aggregation [55]. Further, since it was shown that the ability to accrete CEA is restricted to Kupffer cells [4] and alveolar macrophages [103], thus being tissue-specific, we speculate that these mechanisms may also explain why CEA antibodies, as shown in our studies, control metastasis to the lungs of mice injected i.v. with human colonic tumor cells.
A raised serum CEA level also has been associated with poor cell-mediated immunity and poor survival [54], which is consistent with other evidence that CEA affects lymphocyte function [15, 32, 51, 70, 71, 84] and can interfere with NK and LAK cell activity [81, 82, 86]. These results suggest that CEA may represent an escape mechanism protecting cancer cells from cellular immune attack [70]. In fact, in one study, combining a chimeric mouse–human anti-CEA antibody with LAK cells and IL-2 showed evidence of antitumor activity in vitro and in vivo [86]. However, these authors failed to report any study of the naked antibody without the use of LAK cells and IL-2, but they did demonstrate that the chimeric antibody mediated ADCC in vitro, which is in agreement with the findings reported here as well as other reports that CEA antibodies induce ADCC in cell cultures of colorectal cancer [13, 44, 45, 57, 91, 111]. Finally, our observation that treating mice with GM-CSF enhances the antitumor effects of labetuzumab is consistent with the known effects of this and other cytokines in enhancing antigen expression [20] and ADCC [19].
The in vivo studies showing that the humanized anti-CEA antibody, labetuzumab, can enhance the therapeutic effects of two cytotoxic drugs used frequently in colorectal cancer therapy—5-fluorouracil and CPT-11—in both s.c. and metastatic human colonic tumor cells propagated in nude mice, are the first to suggest such a role for CEA antibodies, and provoke speculation as to how CEA expression on tumor cells may affect the tumor’s sensitivity to such drugs. One explanation may involve a role in blocking cell aggregation, such as by interfering with CEA’s adhesion function [111]. The formation of multicellular aggregates of tumor cells has been shown to increase their resistance to chemotherapy agents, so that disruption of tumor spheroids results in increased growth formation and increased chemosensitivity of tumors in vitro or in vivo [29, 56, 96]. Thus, antibodies that disrupt cell–cell adhesion and prevent the formation of spheroids could increase tumor sensitivity to drugs, as has been shown for the GA733-2 antigen (EpCAM) targeted by the 17.1A antibody, edrecolomab [5]. GA733-2 is, like CEA, a homophilic adhesion receptor that can alter growth, invasion, and metastasis of a colorectal cancer cell line [63].
Another explanation for the chemosensitizing role of CEA antibody may be that inhibition of CEA affects apoptotic stimuli, including the effects of cytotoxic drugs. Using a CEA-targeted ribozyme in human colon cancer cells to regulate CEA levels, it has been reported that CEA does not affect cell cycle or proliferation, but does protect the cells from undergoing apoptosis under various conditions, including confluent growth, UV light, interferon therapy, and treatment with 5FU [95]. Also, transfection of human colon cancer cells with a CEA antisense-expressing vector resulted in a decrease in CEA expression and low tumorigenicity, but such effects involved primary and not metastatic tumors in mice [3]. It seems likely, therefore, that reducing or blocking CEA by administering antibodies against this receptor may overcome this CEA protection in tumor to apoptotic stimuli, as experienced with antisense oligonucleotides [3]. Thus, certain anticancer drugs could have their apoptotic effects enhanced by blocking CEA production and/or expression.
Both the ADCC and chemosensitization effects observed with labetuzumab are similar to those reported for two other antireceptor antibodies of clinical interest—trastuzumab and cetuximab—and indeed their clinical applications appear to be most effective when combined with anticancer drugs [52, 61, 72, 94]. Common mechanisms of action among these antibodies given with drugs include cell-cycle arrest, potentiation of apoptosis, and inhibition of angiogenesis, resulting in augmentation of the antitumor effects of chemotherapy and, in some cases, of radiation therapy [72]. In the case of CEA antibodies, such as the CEACAM5 MAb studied here, a contribution in terms of apoptosis enhancement needs to be considered because of the observation that inhibition of endogenous CEA can achieve this when CEA is overexpressed [80, 108], despite our failure to show direct apoptotic effects by labetuzumab in the tumors tested.
These initial observations of the in vivo antiproliferative and antimetastatic effects of a humanized CEA MAb, labetuzumab, and its potentiation of two common drugs used in colorectal cancer therapy, need to be confirmed and expanded in other tumor models having various levels of CEA expression and with anticancer drugs having diverse mechanisms of action, and eventually in patients. In a high CEA-expressing human medullary thyroid cancer xenograft, we also have shown that this CEA antibody can inhibit tumor cell growth and also augment the effects of dacarbazine, which is active in this cancer type (Stein et al., Mol Cancer Ther, in press).
In addition to its well-known role as a serum marker for a number of CEA-expressing malignancies [23, 27, 33], CEA also has gained attention as a target for radiolabeled antibodies [24], drug and toxin immunoconjugates [1, 17, 66, 67, 90, 92], photodynamic immunotherapy [12], cytokine immunoconjugates [62, 109], vaccines [39, 68, 69, 76], and diverse gene therapy strategies [14, 58, 64, 77, 104]. The studies reported here now suggest that CEACAM5-binding antibodies also have antitumor and chemosensitizing functions. Hence, these various lines of investigation attest that after 4 decades [22], CEA continues to be of major interest and focus in oncology.
Abbreviations
- ADCC:
-
Antibody-dependent cellular cytotoxicity
- CDC:
-
Complement-dependent cytotoxicity
- BrdU:
-
Bromodeoxyuridine
- CDR:
-
Complementarity-determining region
- CEA:
-
Carcinoembryonic antigen
- EDTA:
-
Ethylenediaminetetraacetic acid
- EGFR:
-
Epidermal growth factor receptor
- ELISA:
-
Enzyme-linked immunosorbent assay
- 5FU:
-
5-Fluorouracil
- GM-CSF or rM-GM-CSF:
-
Recombinant murine granulocyte-macrophage colony-stimulating factor
- HRP:
-
Horseradish peroxidase
- IFN-γ:
-
Gamma interferon
- LAK cells:
-
Lymphokine-activated killer cells
- LDH:
-
Lactate dehydrogenase
- MAb:
-
Monoclonal antibody
- MTD:
-
Maximum tolerated dose
- NK cells:
-
Natural killer cells
- PBMC:
-
Peripheral blood mononuclear cell
- pWBC:
-
Peripheral white blood cell
References
Akamatsu Y, Murphy JC, Nolan KF, Thomas P, Kreitman RJ, Leung SO, Junghans RP (1998) A single-chain immunotoxin against carcinoembryonic antigen that suppresses growth of colorectal carcinoma cells. Clin Cancer Res 4:2825–2832
Armstrong A, Eck SL (2003) EpCAM: a new therapeutic target for an old cancer antigen. Cancer Biol Ther 2:320–326
Baczynska D, Wietrzyk J, Madej J, Krop-Watorek A, Dabrowska A, Widerak K, Opolski A, Ugorski M (2003) The tumorigenic potential of human CX-1 colon adenocarcinoma cells depends on carcinoembryonic antigen (CEACAM5) expression. Cell Mol Biol Lett 8:471–486
Bajenova OV, Zimmer R, Stolper E, Salisbury-Rowswell J, Nanji A, Thomas P (2001) Heterogeneous RNA-binding protein M4 is a receptor for carcinoembryonic antigen in Kupffer cells. J Biol Chem 276:31067–31073
Basak S, Speicher D, Eck S, Wunner W, Maul G, Simmons MS, Herlyn D (1998) Colorectal carcinoma invasion inhibition by CO17-1A/GA 733 antigen and its murine homologue. J Natl Cancer Inst 90:691–697
Beauchemin N, Draber P, Dveksler G, Gold P, Gray-Owen S, Grunert F, Hammerstrom S, Holmes KV, Karlsson A, Kuroki M, Lin SH, Lucka L, Najjar SM, Neumaier M, Obrink B, Shively JE, Skubitz KM, Stanners CP, Thomas P, Thompson JA, Virji M, von Kleist S, Wagener C, Watt S, Zimmermann W (1999) Redefined nomenclature for members of the carcinoembryonic antigen family. Exp Cell Res 252:243–249
Benchimol S, Fuks A, Jothy S, Beauchemin N, Shirota K, Stanners CP (1989) Carcinoembryonic antigen, a human tumor marker, functions as a intercellular adhesion molecule. Cell 57:327–334
Bjerner J, Lebedin Y, Bellanger L, Kuroki M, Shively JE, Varaas T, Nustad K, Hammarstrom S, Bormer OP (2002) Protein epitopes in carcinoembryonic antigen. Tumor Biol 23:249–262
Blumenthal RD, Sharkey RM, Haywood L, Natale AM, Wong GY, Siegel JA, Kennel SJ, Goldenberg DM (1992) Targeted therapy of athymic mice bearing GW-39 human colonic cancer micrometastases with 131I-labeled monoclonal antibodies. Cancer Res 52:6036–6044
Blumenthal RD, Sharkey RM, Kashi R, Natale AM, Goldenberg DM (1992) Physiological factors influencing radioantibody uptake: a study of four human colonic carcinomas. Int J Cancer 51:935–941
Blumenthal RD, Alisauskas R, Lew W, Sharkey RM, Goldenberg DM (1998) Myelosuppressive changes from single or repeated doses of radioantibody therapy: effect of bone marrow transplantation, cytokines, and hematopoietic suppression. Exp Hematol 26:859–868
Carcenac M, Larrouque C, Langlois R, van Lier JE, Artus JC, Pelegrin A (1999) Preparation, phototoxicity, and biodistribution studies of anti-carcinoembryonic antigen monoclonal antibody-phthalocyanine conjugates. Photochem Photobiol 70:930–936
Carrel S, Delisle MC, Mach JP (1978) Antiserums against carcinoembryonic antigen (CEA) can induce a specific lysis of colon carcinoma cells by normal lymphocytes. Schweiz Med Wochenschr 108:954–958
Chowdhury S, Chester KA, Bruidgewater J, Collins MK, Martin F (2004) Efficient retroviral vector targeting of carcinoembryonic antigen-positive tumors. Mol Ther 9:85–92
Clark DA, McCulloch PB, Liao SK, Dent PB, Fuks A (1984) Sensitivity of human carcinoma lines to lysis by blood natural killer cells correlating with surface expression of carcinoembryonic antigen. J Natl Cancer Inst 72:505–512
Eidelman FJ, Fuks A, DeMarte L, Taheri M, Stanners CP (1993) Human carcinoembryonic antigen, an intercellular adhesion molecule, blocks fusion and differentiation of rat myoblasts. J Cell Biol 123:467–475
Embleton MJ, Charleston A, Robins RA, Pimm MV, Baldwin RW (1991) Recombinant ricin toxin A chain cytotoxicity against carcinoembryonic antigen expressing tumor cells mediated by bispecific monoclonal antibody and its potentiation by ricin toxin B chain. Br J Cancer 63:670–674
Emmanouilides C, Jazirehi AR, Bonavida B (2002) Rituximab-mediated sensitization of B-non-Hodgkin’s lymphoma (NHL) to cytotoxicity induced by paclitaxel, gemcitabine, and vinorelbine. Cancer Biother Radiopharm 17:621–630
Flieger D, Spengler U, Beier I, Sauerbruch T, Schmidt-Wolf IG (2000) Prestimulation of monocytes by the cytokines GM-CSF or IL-2 enhances the antibody dependent cellular cytotoxicity of monoclonal antibody 17–1A. J Gastroenterol 38:615–622
Flieger D, Hoff AS, Sauerbruch T, Schmidt-Wolf IG (2001) Influence of cytokines, monoclonal antibodies, and chemotherapeutic drugs on epithelial cell adhesion molecule (EpCAM) and LewisY antigen expression. Clin Exp Immunol 123:9–14
Gelderman KA, Kuppen PJ, Bruin W, Fleuren GJ, Gorter A (2002) Enhancement of the complement activating capacity of 17-1A mAb to overcome the effect of membrane-bound complement regulatory proteins on colorectal carcinoma. Eur J Immunol 32:128–135
Gold P, Freedman SO (1965) Specific carcinoembryonic antigens of the human digestive system. J Exp Med 122:467–481
Gold P, Goldenberg NA (1997) The carcinoembryonic antigen (CEA): past, present, and future. McGill J Med 3:46–66
Goldenberg DM (1995) Carcinoembryonic antigen as a target cancer antigen for radiolabeled antibodies: prospects for cancer imaging and therapy. Tumour Biol 16:62–73
Goldenberg DM, Hansen HJ (1972) Carcinoembryonic antigen present in human colonic neoplasms serially propagated in hamsters. Science 175:1117–1118
Goldenberg D, Witte S, Elster K (1966) GW-39: a new human tumor serially transplantable in the golden hamster. Transplantation 4:760–764
Goldenberg DM, Sharkey RM, Primus FJ (1976) Carcinoembryonic antigen in histopathology: immunoperoxidase staining of conventional tissue sections. J Natl Cancer Inst 57:11–22
Goslin R, Steele G Jr, MacIntyre J, Mayer R, Sugarbaker P, Cleghorn K, Wilson R, Zamcheck N (1980) The use of preoperative plasma CEA levels for the stratification of patients after curative resection of colorectal cancer. Ann Surg 192:747–751
Green SK, Francia G, Isidoro C, Kerbel RS (2004) Antiadhesive antibodies targeting E-cadherin sensitizes multicellular tumor spheroids to chemotherapy in vitro. Mol Cancer Ther 3:149–159
Greiner JW, Guadagni F, Roselli M, Nieroda CA (1996) Novel approaches to tumor detection and therapy using a combination of monoclonal antibody and cytokine. Anticancer Res 16:2129–2133
Grimm T, Riethmuller G, Johnson JP (1994) Characteristics of carcinoembryonic antigen (CEA) expressed in different cell types: evidence that CEA can function as an adhesion molecule and as a repulsion molecule. Biochem Biophys Res Commun 204:1225–1234
Hakim A (1984) Carcinoembryonic antigen, a tumor associated glycoprotein, induces defective lymphocyte function. Neoplasma 31:385–397
Hammarstrom S (1999) The carcinoembryonic antigen (CEA) family: structures, suggested functions and expression in normal and malignant tissues. Semin Cancer Biol 9:67–81
Hammarstrom S, Olsen A, Teglund S, Baranov V (1998) The nature and expression of the human CEA family. In: Stanners CP (ed) Cell adhesion and communications mediated by the CEA family basic and clinical perspectives, vol 5. Harwood Academic, Amsterdam, pp 1–30
Hansen HJ, Goldenberg DM, Neman ES, Grebenau R, Sharkey RM (1993) Characterization of second-generation monoclonal antibodies against carcinembryonic antigen. Cancer 71:3478–3485
Hashino J, Fukuda Y, Oikawa S, Nakazato H, Nakanishi T (1994) Metastatic potential in nude mice of Chinese hamster ovary cells expressing human carcinoembryonic antigen. Biochem Biophys Res Commun 200:1748–1753
Hashino J, Fukuda Y, Oikawa S, Nakazato H, Nakanishi T (1994) Metastatic potential of human colorectal carcinoma SW1222 cells transfected with cDNA encoding carcinoembryonic antigen. Clin Exp Metastasis 12:324–328
Hefta SA, Hefta LJ, Lee TD, Paxton RJ, Shively JE (1988) Carcinoembryonic antigen is anchored to membranes by covalent attachment to a glycosylphosphatidylinositol moiety: identification of the ethanolamine linkage site. Proc Natl Acad Sci U S A 85:4648–4652
Horig H, Medina FA, Conkright WA, Kaufman HL (2000) Strategies for cancer therapy using carcinoembryonic antigen vaccines. Expert Rev Mol Med 19:1–24
Hosch SB, Scheunemann P, Luth M, Inndorf S, Stoecklein NH, Erbersdobler A, Rehders A, Gundlach M, Knoefel WT, Izbicki JR (2001) Expression of 17-1A antigen and complement resistance factors CD55 and CD59 on liver metastasis in colorectal cancer. J Gastrointest Surg 5:673–679
Hostetter RB, Augustus LB, Mankarious R, Chi K, Fan D, Toth C, Thomas P, Jessup JM (1990) Carcinoembryonic antigen as a selective enhancer of colorectal cancer metastasis. J Natl Cancer Inst 82:380–385
Hostetter RB, Campbell DE, Chi KF, Kerckhoff S, Cleary KR, Ullrich S, Thomas P, Jessup JM (1990) Carcinoembryonic antigen enhances metastatic potential of human colorectal carcinoma. Arch Surg 125:300–304
Ilantzis C, DeMarte L, Screaton RA, Stanners CP (2002) Deregulated expression of the human marker CEA and CEA family member CEACAM6 disrupts tissue architecture and blocks coloncyte differentiation. Neoplasia 4:151–163
Imai K, Sasanami T, Fujita H, Moriya Y, Tsujisaki M, Kawaharada M, Ferrone S, Yachi A (1983) Antibody-dependent cell-mediated cytotoxicity using monoclonal antibodies reacting with CEA. Ann N Y Acad Sci 417:443–451
Imakiire T, Kuroki M, Shibaguchi H, Abe H, Yamauchi Y, Ueno A, Hirose Y, Yamada H, Yamashita Y, Shirakusa T, Ishida I, Kuroki M (2004) Generation, immunologic characterization and antitumor effects of human monoclonal antibodies for carcinoembryonic antigen. Int J Cancer 108:564–570
Jessup JM, Thomas P (1989) Carcinoembryonic antigen: function in metastasis by human colorectal carcinoma. Cancer Metastasis Rev 8:263–280
Jessup JM, Thomas P (1998) CEA and metastasis: a facilitator of site-specific metastasis. In: Stanners CP (ed) Cell adhesion and communication by the CEA family, vol 5. Harwood Academic, Amsterdam, pp 195–222
Jessup JM, Giavazzi R, Campbell D, Cleary K, Morikawa K, Fidler IJ (1988) Growth potential of human colorectal carcinomas in nude mice: association with the preoperative serum concentration of carcinoembryonic antigen in patients. Cancer Res 48:1689–1692
Jessup JM, Giavazzi R, Campbell D, Cleary KR, Morikawa K, Hostetter R, Atkinson EN, Fidler IJ (1989) Metastatic potential of human colorectal carcinomas implanted into nude mice: prediction of clinical outcome in patients operated upon for cure. Cancer Res 49:6906–6910
Jessup JM, Ishii S, Mitzoi T, Edmiston KH, Shoji Y (1999) Carcinoembryonic antigen facilitates experimental metastases through a mechanism that does not involve adhesion to liver cells. Clin Exp Metastasis 17:481–488
Kammerer R, von Kleist S (1996) The carcinoembryonic antigen (CEA) modulates effector-target cell interaction by binding to activated lymphocytes. Int J Cancer 68:457–463
Kim ES, Khuri FR, Herbst R (2001) Epidermal growth factor receptor biology (IMC-C225). Curr Opin Oncol 13:506–513
Kim JC, Roh SA, Park KC (1997) Adhesive function of carcinoembryonic antigen in the liver metastasis of KM-12c colon carcinoma cell line. Dis Colon Rectum 40:946–953
King J, Caplehorn JR, Ross WB, Morris DL (1997) High serum carcinoembryonic antigen concentration in patients with colorectal liver metastasis is associated with poor cell-mediated immunity, which is predictive of survival. Br J Surg 84:1382–1385
Kitsuki H, Katano M, Morisaki T, Torisu M (1995) CEA-mediated homotypic aggregation of human colorectal carcinoma cells in a malignant effusion. Cancer Lett 88:7–13
Kobayashi H, Man S, Graham CH, Kapitain SJ, Teicher BA, Kerbel RS (1993) Acquired multicellular-mediated resistance to alkylating agents in cancer. Proc Natl Acad Sci U S A 90:3294–3298
Koga H, Kanda H, Nakashima M, Watanabe Y, Endo K, Watanabe T (1990) Mouse–human chimeric monoclonal antibody to carcinoembryonic antigen (CEA): in vitro and in vivo activities. Hybridoma 9:43–56
Kuroki M, Arakawa F, Khare PD, Kuroki M, Liao S, Matsumoto H, Abe H, Imakiire T (2000) Specific targeting strategies of cancer gene therapy using a single-chain variable fragment (scFv) with a high affinity for CEA. Anticancer Res 20:4067–4071
Lavelle F, Bissery MC, Andre S, Roquet F, Riou JF (1996) Preclinical evaluation of CPT-11 and its active metabolite SN-38. Semin Oncol 23:11–20
Leconte A, Garambois V, Ychou M, Robert B, Purquier D, Tereskikh A, Mach JP, Pelegrin A (1999) Involvement of circulating CEA in liver metastases from colorectal cancers re-examined in a new experimental model. Br J Cancer 80:1373–1379
Lee S, Yang W, Lan KH, Sellappan S, Klos K, Hortobagyi G, Hung MC, Yu D (2002) Enhanced sensitization to taxol-induced apoptosis by herceptin pretreatment in ErbB2-overexpressing breast cancer cells. Cancer Res 62:5703–5710
Liao S, Khare PD, Arakawa F, Kuroki M, Hirose Y, Fijimura S, Tomita Y, Kuroki M (2001) Targeting of LAK activity to CEA-expressing tumor cells with an anti-CEA scFv/IL-2 fusion protein. Anticancer Res 21:1673–1680
Litvinov M, Velders MP, Bakker HA, Fleuren GJ, Warnaar SO (1994) Ep-CAM: a human epithelial antigen is a homophilic cell-cell adhesion molecule. J Cell Biol 125:437–446
Ma Q, DeMarte L, Wang Y, Stanners CP, Junghans RP (2004) Carcinoembryonic antigen-immunoglobulin Fc fusion protein (CEA-Fc) for identification and activation of anti-CEA immunoglobulin-T-cell-modified T cells, representative of a new class of IgG fusion proteins. Cancer Gene Ther Adv Online 11:297–306
Maloney DG, Smith B, Rose A (2002) Rituximab: mechanism of action and resistance. Semin Oncol 29:2–9
Manosroi J, von Kleist S, Manosroi A, Grunert F (1992) Thermo-stability ond antitumor activity on colon cancer cell lines of monoclonal anti-CEA antibody-sporin immunotoxin. J Korean Med Sci 7:128–135
Mao W, Luis E, Ross S, Silva J, Tan C, Crowley C, Chui C, Franz G, Senter P, Koeppen H, Polakis P (2004) EphB2 as a therapeutic antibody drug target for the treatment of colorectal cancer. Cancer Res 64:781–788
Marshall J (2003) Carcinoembryonic antigen-based vaccines. Semin Oncol 30:30–36
Marshall JL, Hoyer RJ, Toomey MA, Faraguna K, Chang P, Richmond E, Pedicano JE, Gehan E, Peck RA, Arlen P, Tsang KY, Schlom J (2000) Phase I study in cancer patients of a diversified prime and boost vaccination protocol using recombinant vaccinia virus and recombinant nonreplicating avipox virus to elicit anti-carcinoembryonic antigen immune responses. J Clin Oncol 18:3964–3973
Medoff JR, Jegasothy BV, Roche K (1984) Carcinoembryonic antigen-induced release of a suppressor factor from normal human lymphocytes in vitro. Cancer Res 44:5822–5827
Medoff JR, Clack VD, Roche JK (1986) Characterization of an immunosuppressive factor from malignant ascites that resembles a factor induced in vitro by carcinoembryonic antigen. J Immunol 137:2057–2064
Mendelsohn J, Baselga J (2003) Status of epidermal growth factor antagonists in the biology and treatment of cancer. J Clin Oncol 21:2787–2799
Minami S, Furui J, Kanematsu T (2001) Role of carcinoembryonic antigen in the progression of colon cancer cells that express carbohydrate antigen. Cancer Res 61:2732–2735
Nakamura T, Tabuchi Y, Nakae S, Ohno M, Saitoh Y (1996) Serum carcinoembryonic antigen levels and proliferating cell nuclear antigen labeling index for patients with colorectal carcinoma: correlation with tumor progression and survival. Cancer 77:1741–1746
Naundorf S, Preithneg S, Mayer P, Lippold S, Wolf A, Hanakam F, Fichtner I, Kufer P, Raum T, Riethmuller G, Baeuerle PA, Dreier T (2002) In vitro and in vivo activity of MT201, a fully human monoclonal antibody for pancarcinoma treatment. Int J Cancer 100:101–110
Niethammer AG, Primus FJ, Xiang R, Dolman CS, Ruehlmann JM, Ba Y, Gillies SD, Reisfeld RA (2001) An oral DNA vaccine against human carcinoembryonic antigen prevents growth and dissemination of Lewis lung carcinoma in CEA transgenic mice. Vaccine 20:421–429
Nolan KF, Yun CO, Akamatsu Y, Murphy JC, Leung SO, Beecham EJ, Junghans RP (1999) Bypassing immunization: optimized design of “designer T cells” against carcinoembryonic antigen (CEA)-expressing tumors, and lack of suppression by soluble CEA. Clin Cancer Res 5:3928–3941
Oikawa S, Imajo S, Noguchi T, Kosaki G, Nakazato H (1987) The carcinoembryonic antigen (CEA) contains multiple immunoglobulin-like domains. Biochem Biophys Res Commun 144:634–642
Oikawa S, Inuzuka C, Kuroki M, Matsuoka Y, Kosaki G, Nakazato H (1989) Cell adhesion activity of non-specific cross-reacting antigen (NCA) and carcinoembryonic antigen (CEA) expressed on CHO cell surface: homophilic and heterophilic adhesion. Biochem Biophys Res Commun 164:39–45
Ordonez C, Screaton RA, Ilantzis C, Stanners CP (2000) Human carcinoembryonic antigen functions as a general inhibitor of anoikis. Cancer Res 60:3419–3424
Pellegrini P, Berghella AM, Del Beato T, Maccarone D, Cencioni S, Adorno D, Casciani CU (1997) The sCEA molecule suppresive role in NK and TH1 cell functions in colorectal cancer. Cancer Biother Radiopharm 12:257–264
Prado IB, Laudanna AA, Carneiro CR (1995) Susceptibility of colorectal-carcinoma cells to natural-killer-mediated lysis: relationship to CEA expression and degree of differentiation. Int J Cancer 61:854–860
Primus FJ, Newell KD, Blue A, Goldenberg DM (1983) Immunological heterogeneity of carcinoembryonic antigen: antigenic determinants on carcinoembryonic antigen distinguished by monoclonal antibodies. Cancer Res 43:686–692
Rivoltini L, Cattoretti G, Arienti F, Mastroianni A, Parmiani G (1992) CEA and NCA expressed by colon carcinoma cells affect their interaction with and lysability by activated lymphocytes. Int J Biol Markers 7:143–147
Screaton RA, Penn LZ, Stanners CP (1997) Carcinoembryonic antigen, a human tumor marker, cooperates with Myc and Bcl-2 in cellular transformation. J Cell Biol 137:939–952
Senba T, Kuroki M, Arakawa F, Yamamoto T, Kuwahara M, Haruno M, Ikeda S, Matsuoka Y (1998) Tumor growth suppression by a mouse/human chimeric anti-CEA antibody and lymphokine-activated killer cells in vitro and in SCID mouse xenograft model. Anticancer Res 18:17–24
Sharkey RM, Weadock KS, Natale A, Haywood L, Aninipot R, Blumenthal RD, Goldenberg DM (1991) Successful radioimmunotherapy for lung metastasis of human colonic cancer in nude mice. J Natl Cancer Inst 83:627–632
Sharkey RM, Goldenberg DM, Murthy S, Pinsky H, Vagg R, Pawlyk D, Siegel JA, Wong GY, Gascon P, Izon DO, Verra M, Burger K, Swayne LC, Pinsky CM, Hansen HJ (1993) Clinical evaluation of tumor targeting with a high-affinity anti-carcinoembryonic-antigen-specific murine monoclonal antibody, MN-14. Cancer 71:2082–2096
Sharkey RM, Juweid M, Shevitz J, Behr T, Dunn R, Swayne LC, Wong GY, Blumenthal RD, Griffiths GL, Siegel JA, Leung S, Hansen HJ, Goldenberg DM (1995) Evaluation of a complementarity-determining region-grafted (humanized) anti-carcinoembryonic antigen monoclonal antibody in preclinical and clinical studies. Cancer Res 55:5935–5945
Sharma SK, Boden JA, Springer CJ, Burke PJ, Bagshawe KD (1994) Antibody-directed enzyme prodrug therapy (ADEPT): a three-phase study in ovarian tumor xenografts. Cell Biophys 24–25:219–228
Shibaguchi H, Arakawa F, Imakiire T, Kuroki M, Kuroki M (2003) cDNA cloning and sequencing of a novel monoclonal antibody to carcinoembryonic antigen and construction of a mouse/human chimeric antibody. Anticancer Res 23:4383–4388
Shih LB, Goldenberg DM, Xuan H, Lu H, Sharkey RM, Hall TC (1991) Anthracycline immunoconjugates prepared by a site-specific linkage via an amino-dextran intermediate carrier. Cancer Res 51:4192–4198
Shively JE, Beatty JD (1985) CEA-related antigens: molecular biology and clinical significance. Crit Rev Oncol Hematol 2:355–399
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M, Baslga J, Norton L (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344:783–792
Soeth E, Wirth T, List HJ, Kumbhani S, Petersen A, Neumaier M, Czubayko F, Juhl H (2001) Controlled ribozyme targeting demonstrates an antiapoptotic effect of carcinoembryonic antigen in HT-29 colon cancer cells. Clin Cancer Res 7:2022–2030
St Croix B, Kerbel RS (1997) Cell adhesion and drug resistance in cancer. Curr Opin Oncol 9:549–556
Stanners CP, Fuks A (1998) Properties of adhesion mediated by the human CEA family. In: Stanners CP (ed) Cell adhesion and communication by the CEA family, vol 5. Harwood Academic, Amsterdam, pp 57–72
Stein R, Qu Z, Chen S, Rosario A, Shi V, Hayes M, Horak ID, Hansen HJ, Goldenberg DM (2004) Characterization of a new humanized anti-CD20 monoclonal antibody, IMMU-106, and its use in combination with the humanized anti-CD22 antibody, epratuzumab, for the therapy of non-Hodgkin’s lymphoma. Clin Cancer Res 10:2868–2878
Taheri M, Saragovi HU, Stanners CP (2003) The adhesive and differentiation-inhibitory activities of the immunoglobulin superfamily member, carcinoembryonic antigen, can be independently blocked. J Biol Chem 278:14632–14639
Thomas P, Gangopadhyay A, Steele GJ, Andrews C, Nakazoto H, Oikawa S, Jessup JM (1995) The effect of transfection of the CEA gene on the metastatic behavior of the human colorectal cancer cell line MIP-101. Cancer Lett 92:59–66
Thompson JA, Grunert F, Zimmermann W (1991) Carcinoembryonic antigen gene family: molecular biology and clinical perspectives. J Clin Lab Anal 5:344–366
Tibbetts LM, Doremus CM, Tzanakakis GN, Vezeridis MP (1993) Liver metastases with 10 human colon carcinoma cell lines in nude mice and association with carcinoembryonic antigen production. Cancer 71:315–321
Toth CA, Rapoza A, Zamcheck N, Steele GJ, Thomas P (1989) Receptor-mediated endocytosis of carcinoembryonic antigen by rat alveolar macrophages in vitro. J Leukoc Biol 45:370–376
Ueda K, Iwahashi M, Nakamori M, Nakamura M, Matsuura I, Ojima T, Yamaue H (2003) Improvement of carcinoembryonic antigen-specific prodrug gene therapy for experimental colon cancer. Surgery 133:309–317
von Kleist S, Migule I, Halla B (1995) Possible function of CEA as cell-contact inhibitory molecule. Anticancer Res 15:1889–1894
Wagner HE, Toth CA, Steele GDJ, Thomas P (1992) Metastatic potential of human colon cancer cell lines: relationship to cellular differentiation and carcinoembryonic antigen production. Clin Exp Metastasis 10:25–31
Wanebo H, Rao B, Pinsky CM, Hoffman RG, Stearns M, Schwartz MK, Oettgen HF (1978) Preoperative carcinoembryonic antigen level as a prognostic indicator in colorectal cancer. N Engl J Med 299:448–451
Wirth T, Soeth E, Czubayko F, Juhl H (2002) Inhibition of endogenous carcinoembryonic antigen (CEA) increases the apoptotic rate of colon cancer cells and inhibits metastatic tumor growth. Clin Exp Metastasis 19:155–160
Xu X, Clarke P, Szalai G, Shively JE, Williams LE, Shyr Y, Shi E, Primus FJ (2000) Targeting and therapy of carcinoembryonic antigen-expressing tumors in transgenic mice with an antibody-interleukin-2 fusion protein. Cancer Res 60:4475–4484
Yoshioka T, Masuko T, Kotanagi H, Aizawa O, Saito Y, Nakazato H, Koyama K, Hashimoto Y (1998) Homotypic adhesion through carcinoembryonic antigen plays a role in hepatic metastasis development. Jpn J Cancer Res 89:177–185
Zhou H, Stanners CP, Fuks A (1993) Specificity of anti-carcinoembryonic antigen monoclonal antibodies and their effects on CEA-mediated adhesion. Cancer Res 53:3817–3822
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Blumenthal, R.D., Osorio, L., Hayes, M.K. et al. Carcinoembryonic antigen antibody inhibits lung metastasis and augments chemotherapy in a human colonic carcinoma xenograft. Cancer Immunol Immunother 54, 315–327 (2005). https://doi.org/10.1007/s00262-004-0597-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-004-0597-6