Abstract
Expression of the cancer-testis antigen Taxol resistance–associated gene-3 (TRAG-3) protein is associated with acquired paclitaxel (Taxol) resistance, and is expressed in various cancer types; e.g., breast cancer, leukemia, and melanoma. Thus, TRAG-3 represents an attractive target for immunotherapy of cancer. To identify HLA-A*02.01–restricted epitopes from TRAG-3, we screened cancer patients for spontaneous cytotoxic T-cell responses against TRAG-3–derived peptides. The TRAG-3 protein sequence was screened for 9mer and 10mer peptides possessing HLA-A*02.01–binding motifs. Of 12 potential binders, 9 peptides were indeed capable of binding to the HLA-A*02.01 molecule, with binding affinities ranging from strong to weak binders. Subsequently, lymphocytes from cancer patients (9 breast cancer patients, 12 melanoma patients, and 13 patients with hematopoietic malignancies) were analyzed for spontaneous reactivity against the panel of peptides by ELISpot assay. Spontaneous immune responses were detected against 8 epitope candidates in 7 of 9 breast cancer patients, 7 of 12 melanoma patients, and 5 of 13 patients with hematopoietic malignancies. In several cases, TRAG-3–specific CTL responses were scattered over several epitopes. Hence, no immunodominance of any single peptide was observed. Furthermore, single-peptide responses were detected in 2 of 12 healthy HLA-A2+ donors, but no responses were detectable in 9 HLA-A2− healthy donors or 4 HLA-A2− melanoma patients. The identified HLA-A*02.01–restricted TRAG-3–derived epitopes are targets for spontaneous immune responses in breast cancer, hematopoietic cancer, and melanoma patients. Hence, these epitopes represent potential target structures for future therapeutic vaccinations against cancer, possibly appropriate for strategies that combine vaccination and chemotherapy; i.e., paclitaxel treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The major component of antitumor immune responses, the cytotoxic T cell (CTL), is capable of direct lysis of tumor cells, in addition to secretion of cytokines with secondary antitumor effects, such as IL-2, TNF-α, GM-CSF, and IFN-γ [31]. Hence, treatment of cancers by induction of specific antitumor CTLs represents an appealing therapeutic concept; especially since conventional treatment of metastatic disease rarely produces durable responses [52]. Moreover, the last decade has revealed considerable advances in understanding of the molecular and cellular mechanisms involved in initiating and sustaining of cellular immune responses [45]. This implies that immunotherapeutic intervention of cancer is now manageable through the specific targeting of peptides expressed by cancer cells in the context of HLA molecules. Although several hurdles need to be overcome, this strategy holds promise for improving the clinical outcome for cancer patients [32]. Compared with more nonspecific modulators of cellular immune responses—e.g., administration of cytokines—the specific targeting of tumor-associated antigens (TAAs) necessitates the identification and characterization of antigenic peptides from those TAAs [51].
Cancer-testis (CT) antigens are a group of proteins expressed in male germline cells and certain tumor types, but not, or at least 1,000-fold less, in other healthy tissues [22, 43]. Because of the blood-testis barrier and the immune-privileged status of germline cells, these antigens can be considered functionally tumor-specific, and hence, represent attractive targets for immunotherapy [51, 55]. The main additional characteristics of this group are mapping to the X chromosome, the presence of multigene families, and immunogenicity in cancer patients [11]. Subsequent studies have identified additional characteristics, like heterogeneous antigen expression in cancer, and association with tumor progression and the metastatic potential of cancer cells, but also exceptions to all of these characteristics [6, 42, 51]. The function of the CT antigens is not fully known, and so far the cellular role has only been elucidated for a few of these proteins [42].
Identification of CT antigens has been achieved in several ways [55]. The Taxol resistance–associated gene-3 (TRAG-3) was identified by comparing mRNA expression profiles of the Taxol-sensitive ovarian cancer line SKOV3, to a Taxol-resistant daughter line [14, 16]. Thus, TRAG-3 was identified as a transcript associated with paclitaxel (Taxol) resistance in cancer. Although there is no evidence for a direct role in the acquisition of paclitaxel resistance, TRAG-3 and the splice variant TRAG-3L are expressed in cancers of the colon, CNS, ovary, kidney, prostate, and breast, as well as non–small cell lung cancers, melanomas, and leukemias, but not in normal, nontestis tissue [9, 14, 16]. The broad expression among tumors suggests that exposure to paclitaxel is not a requisite for TRAG-3 expression, but probably that the expression frequencies increase with tumor progression as observed with other CT antigens [7].
Numerous TAAs have been characterized, and T-cell peptide epitopes identified [36]. Some of these peptides have been used in peptide-based vaccination trials, in particular peptides derived from melanocyte differentiation antigens in vaccinations against melanoma, in some cases demonstrating remarkable response rates [30, 40]. However, these antigens are not broadly applicable in cancer immunotherapy. CT antigens are more broadly expressed among cancers, and therapeutic vaccination against cancer with CT-derived peptides have been shown to induce clinically relevant antitumor responses [18, 23, 28, 29, 37]. Hence, immunization with T-cell epitopes from the TRAG-3 protein might be beneficial, and could potentially be successfully combined with chemotherapy, i.e., paclitaxel treatment.
The first human tumor antigen recognized by CTLs, the MAGE-3/HLA-A1 peptide, was discovered by cloning the epitope recognized by autologous CTLs [50]. A different approach was recently undertaken in the study of Zhu et al. [56] describing the characterization of a TRAG-3–derived peptide by means of establishing specific CTLs by repeated in vitro peptide stimulation.
In the present study, we used the principles of reverse immunology [46] for an extensive study of the immunogenicity of the TRAG-3 protein. We present data demonstrating spontaneous CTL responses against eight HLA-A*0201–restricted TRAG-3–derived peptides in cancer patients. Spontaneous responses were detected in patients with breast cancer, melanoma, as well as hematopoietic malignancies. Our data suggests that TRAG-3–derived peptides are widely applicable in therapeutic vaccinations against cancer.
Materials and methods
Patients
Blood and tumor biopsies from melanoma and breast cancer patients as well as from patients with hematopoietic malignancies were included. The Danish Ethical Committee approved the protocol, and all patients provided informed consent to participate and donate blood and biopsy material. Serological HLA typing revealed that 9 breast cancer patients, 13 melanoma patients, and 12 patients with hematopoietic malignancies were HLA-A2-positive and these were included in the present study. None of the patients received immunotherapy prior to sampling of blood and/or biopsies.
As negative controls, 12 healthy HLA-A2-positive donors, 9 healthy HLA-A2-negative donors, and 4 HLA-A2-negative melanoma patients were included in the study.
Peptides and cell lines
Twelve synthetic 9mer and 10mer peptides were produced by Invitrogen, Taastrup, Denmark. Two of the peptides addressed the insert region in the splice variant TRAG-3L [16], either completely (T_L95) or partially (T_L102). The peptide denoted T_4 along with the three control peptides (EBV BMLF1259-267, Flu Matrix58-66, and HIV-1 pol476-484) were dissolved in DMSO (final concentration 10 mg/ml); all other peptides were dissolved in distilled water (final concentration 2 mg/ml). The transporter associated with antigen processing (TAP) deficient cell line (T2 cells) used in this study is derived from a hybrid of the B-LCL.174 and T.LCL CEM (116) cell lines, and hence is a hybrid of a B-cell line and a T-cell line with immortal properties. The T2 cell line was maintained in RPMI 1640 (GibcoBRL, Life Technologies, Roskilde, Denmark) with 10% FCS.
MHC class I peptide–binding assay
TAP-deficient T2 cells (5×106 cells/sample) were incubated 45 min at 37°C, 5% CO2 in methionine-free RPMI 1640 (GibcoBRL) with 10% FCS. Subsequently, cells were labeled by addition of 50 μCi35 S-methionine per sample. After a 30-min incubation step, cells were lysed in 500 μl ice-cold lysis buffer in the presence of protease inhibitors and peptide in varying concentrations (20–0.02 μM). Cell nuclei were pelleted by ultracentrifugation, and the samples were precleared by addition of Pansorbin (Calbiochem, Nottingham, UK), and left on rotation overnight. After centrifugation, the supernatant was isolated, and antibody (W6/32) for immunoprecipitation of the HLA-peptide complex was added. A-Sepharose beads were added to collect the folded MHC complexes attached by the antibodies, and subsequently, the beads were washed four times in lysis buffer, pelleted, and run on iso-electric focusing (IEF) gels. After electrophoresis, gels were exposed to PhosphorImager screens, and peptide binding was quantitated using the Imagequant PhosphorImager program (Molecular Dynamics, Sunnyvale, Calif., USA).
Antigen stimulation of peripheral blood lymphocytes (PBLs)
To extend the sensitivity of the ELISpot assay, PBLs were stimulated once in vitro prior to analysis [33, 34]. At day 0, PBLs or biopsy samples were thawed and plated in 2 ml/well at a concentration of 2×106 cells in 24-well plates (Nunc, Denmark) in X-Vivo medium (BioWhittaker, Walkersville, Md., USA), 5% heat-inactivated human serum in the presence of 10 μM of peptide. Two days later, 20 IU/ml recombinant interleukin 2 (IL-2) (Chiron, Ratingen, Germany) was added to the cultures. The cultured cells were tested for reactivity by ELISpot on day 10.
ELISpot assay
Ninety-six-well nitrocellulose plates (Multiscreen MAIP N45; Millipore, Hedehusene, Denmark) were coated with 7.5 μg/ml mouse anti-IFN-γ monoclonal antibody (1-D1k; Mabtech, Nacka, Sweden) in 75 μl PBS overnight at room temperature. After washing several times and blocking with 200 μl X-Vivo media (BioWhittaker, Walkersville, Md., USA), 104 T2 cells (unpulsed or pulsed with 1 μg peptide) and lymphocytes in three different concentrations (105, 3×104, and 104 cells per well) were added to each well. After incubation overnight, the plates were washed 6 times, and biotinylated secondary anti-IFN-γ antibody (7-B6-Biotin; Mabtech) was added. After a 2-h incubation step, the plates were washed 6 times and avidin-enzyme conjugate (Life Technologies) was added to each well. After 1 h incubation at RT, the plates were washed 6 times, and enzyme substrate (DAKOcytomation; DAKO, Carpinteria, Calif., USA) was added to each well, and incubated for 5–10 min at RT. When dark purple spots emerged, the reaction was terminated by washing with tap water. Spots were quantitated using a computerized ELISpot counter (Immunospot; CTL, Calif., USA). Responses were defined as average number of antigen-specific spots ± 1/2 standard deviation >25 per 105 lymphocytes.
Results
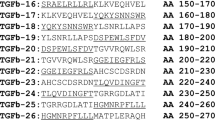
Binding of TRAG-3–derived peptides to HLA-A2
The amino acid sequences of the TRAG-3 and the splice variant TRAG-3L proteins were screened for the most probable HLA-A*02.01 9mer and 10mer peptide epitopes, using the main HLA–specific anchor residues [2, 35]. Ten TRAG-3 and two TRAG-3L deduced peptides were synthesized and examined for binding to HLA-A*02.01 by comparison with the high-affinity positive control epitope from HIV-1 pol476-484 (ILKEPVHGV) in the assembly assay. This assay measures the ability of any given peptide to bind to the MHC molecule, taking advantage of metabolically labeled 35S-methionine, enabling a measure of increased stability of MHC class I molecules upon binding of a peptide. In short, TAP-deficient cell line T2 was loaded with peptide, whereupon correctly folded, stable MHC heavy chains were immunoprecipitated using a conformation-dependent antibody [3]. After separation by IEF electrophoresis, gels where exposed, and correctly folded MHC molecules were quantitated. The extent of stabilization of class I MHC molecules is directly related to the binding affinity of the added peptide. The peptide concentration required for half maximal recovery of class I MHC molecules (C50 value) was 0.2 μM for the HIV-1 pol476-484 (Table 1). Three TRAG peptides bound with high affinity similar to the positive control: T_4, T_45, and T_58 (C50=0.3, 0.7, and 0.7 μM, respectively). The peptides T_57.10, T_59, and T_L102 bound with intermediate affinity (C50=35, 5, and 16 μM, respectively), and T_29, T_37.9, and T_57.9 bound only weakly to HLA-A2 (C50>100 μM). The remaining three peptides had HLA-A*0201 affinities below the detection limit of the assay (not binding, NB).
Identification of spontaneous CTL responses in cancer patients
We analyzed the T-cell responses in 9 breast cancer patients, 12 melanoma patients, and 13 patients with hematopoietic malignancies, against the panel of TRAG-3–derived peptides capable of binding to the HLA-A*0201 molecule (Fig. 1). This was carried out using the ELISpot assay [4].
Overview of ELISpot results. PBLs from 12 healthy HLA-A*02.01-positive donors (a), 9 healthy HLA-A*02.01-negative donors (b), 4 HLA-A*02.01-negative melanoma patients (c), 9 HLA-A*02.01-positive breast cancer patients (d), 13 HLA-A*02.01-positive patients with hematopoietic malignancies (e), and 12 HLA-A*02.01-positive melanoma patients (f) were tested for spontaneous immune responses against the panel of TRAG-3–derived peptides capable of binding to HLA-A*02.01 molecules
In PBLs from breast cancer patients, spontaneous immune responses were detected against one or several peptides in seven of nine patients (78%) (Fig. 2). In this group, the majority of responses were directed against T_37.9, T_4, and T_57.10. However, single immune responses were detected against T_29, T_45, T_58, and T_L102, the last overlapping the insert region of the splice variant TRAG-3L. Furthermore, the PBLs from this group were tested against the irrelevant peptide HIV-1 pol476-484. Data from these experiments showed highly comparable results when testing unpulsed T2 cells versus T2 cells pulsed with HIV-1 pol476-484, even after a 10-day stimulation of the PBLs with the HIV-1 pol476-484 peptide (data not shown).
Spontaneous immune responses against TRAG-3–derived peptides in HLA-A2-positive breast cancer patients. Responses were detected by ELISpot, measuring IFN-γ secretion by T cells. Peptide-specific spontaneous responses were measured twice in triplicates. Columns represent the number of antigen-specific spots formed per 105 T cells; bars indicate SD. Dark columns indicate spontaneous responses (defined as antigen-specific spots ± 1/2 SD >25 spots per 105 cells)
In patients with various hematopoietic malignancies, immune responses against TRAG-3–derived peptides were detected in 5 of the 13 patients examined (38%) (Fig. 3). In this group, immune responses against T_4 and T_58 tended to be slightly dominating, with dispersed responses against T_29, T_37.9, T_57.9, T_57.10, and T_L102. Notably, no responses against the strong binder T_45 were observed in this group. The lymphocytes in this group originated from blood samples from patients with chronic lymphatic leukemia (CLL), lymphoma (LYM), or multiple myeloma (MM). The responding samples originated from one CLL, two LYM, and two MM patients. The nonresponding lymphocytes originated from two CLL, three LYM, and three MM patients. Due to limited patient material available from the melanoma patients and those suffering from hematological malignancies, it was not possible to analyze for reactivity against the full panel of HLA-A*02.01–binding peptides in these patients.
Spontaneous immune responses against TRAG-3–derived peptides in HLA-A2-positive hematopoietic patients. Responses were detected by ELISpot, measuring IFN-γ secretion by T cells. Due to limited patient material, it was not possible to analyze for reactivity against the full panel of peptides in all patients. Columns represent the number of antigen specific spots formed per 105 T cells. Dark columns indicate spontaneous responses (defined as antigen specific spots ± 1/2 SD >25 spots per 105 cells); bars indicate SD. CLL chronic lymphatic leukemia, MM multiple myeloma, LYM lymphoma
In melanoma patients, TRAG-3–specific immune responses were detected in 7 of 12 patients (58%) (Fig. 4). The immune responses against the strong binders T_4 and T_45 were prominent in this group, with dispersed responses against T_29, T_37.9, T_57.9, T_57.10, and T_L102. The responding melanoma patient material originated from tumor-infiltration lymphocytes (TILs) from one subcutaneous metastasis and one lymph node metastasis, in addition to PBLs. The nonresponding lymphocytes were TILs from two lymph node metastases, a subcutaneous metastasis, and a primary tumor, in addition to PBLs from a blood sample.
Spontaneous immune responses against TRAG-3–derived peptides in HLA-A2-positive melanoma patients. Responses were detected by ELISpot, measuring IFN-γ secreted by T cells upon TCR stimulation. Due to limited patient material, it was not possible to analyze for reactivity against the full panel of peptides in all patients. Columns represent the number of antigen specific spots formed per 105 T cells. Dark columns indicate spontaneous responses (defined as antigen specific spots ± 1/2 SD >25 spots per 105 cells). Bars indicate SD. Lymphocytes of responding patients originated from infiltrated lymph nodes (LN), metastases (ME), or blood samples (PBL)
Identification of spontaneous CTL responses in control samples
To verify that the observed spontaneous TRAG-3–specific responses found in cancer patients were related to tumorigenesis and expression of HLA-A2 molecules, we included lymphocytes from healthy donors and HLA-A2-negative cancer patients. Thus, PBLs from 12 HLA-A2-positive healthy donors, 9 healthy HLA-A2-negative donors, and 4 HLA-A2-negative melanoma patients were tested using ELISpot, for spontaneous TRAG-3 reactivity against the full panel of HLA-A2–binding peptides, under the same conditions as described above. Neither the HLA-A2-negative healthy donor PBLs nor the HLA-A2-negative melanoma patient PBLs elicited any measurable TRAG-3 reactivity. However, 2 of 12 donors (17%) in the group of HLA-A2-positive healthy donors displayed TRAG-3–specific responses against T_45 (38 ± 7 specific spots per 105 cells; calculated as in Figs. 2, 3, and 4) and T_57.10 (94 ± 13 specific spots per 105 cells), respectively.
Furthermore, the HLA-A2-positive healthy donors were used as positive controls for the ELISpot assay by testing PBMCs stimulated with the EBV BMLF1259-267 and the Flu Matrix58-66 peptides. This resulted in strong, highly significant responses for all donors against the EBV BMLF1259-267 peptide in addition to similar responses for the majority of the donors against the Flu Matrix58-66 peptide (data not shown).
Discussion
Since the first human T-cell epitope derived from a TAA was described in melanoma more than a decade ago [50], numerous antigens expressed by melanoma cells have been identified and molecularly characterized [36]. Moreover, during the past few years T-cell antigens have been characterized in several other neoplasms, leading to the notion that host T cells in general have the capacity to recognize cancer cells [1, 19]. Together with advances in the identification and characterization of the cells and molecules involved in the initiation and sustaining of cellular immune responses [17], this has provided scientists and clinicians with sophisticated tools for immunological targeting of cancer cells.
Characterization of TAA-derived CTL epitopes is essential to allow active specific immunization of cancer patients. In the absence of well-defined tumor-reactive T-cell clones, reverse immunology has been used by many investigators to identify novel tumor-associated antigens [38, 46, 51]. In the present study, we employed this technique to identify TRAG-3–derived CTL epitopes capable of binding to the HLA-A*02.01, leading to the characterization of nine such peptides binding with variable affinities to the class I molecule.
Several methods are available for monitoring of antitumor CTL responses, however, due to its high throughput and sensitivity, the ELISpot assay represents the method of choice in many laboratories [54]. Using this approach, responses were detected against eight of the nine peptides capable of binding to the HLA molecule. Considering compiled reactivity among the included patient groups, responses were detected in approximately 50% of the patients, and no responses were detected in HLA-A2-negative controls. In view of the high response frequency, it could be speculated that lack of responses could be due to lack of antigen expression, and that the response rates analyzed in cancer patients having TRAG-3–expressing tumors therefore in reality might be even higher. In this respect, however, data from melanoma samples suggests that the majority of melanomas express TRAG-3 [16]. Unfortunately, biopsies were not available from the breast cancer patients included in the present study; however, Wu and colleagues recently reported expression of TRAG-3 in 23 of 34 mainly invasive breast carcinomas [53]. Summing up, the highest response rates were detected in breast cancer patients (78%). It could be speculated that the high response rate in these samples is related to expression of TRAG-3 in response to treatment, since these patients received systemic administration of chemotherapy in the treatment of their disease; however, this is true for the patients suffering from hematopoietic malignancies as well. Still, the response rates are surprisingly high, in particular since spontaneous CTL responses against CT antigens are not frequent [27]. Exceptions to this are the MAGE-10254-262 HLA-A*02.01–restricted peptide inducing spontaneous CTL responses in two thirds of melanoma patients [49], and the NY-ESO-1 protein similarly eliciting spontaneous CTL reactivity in melanoma patients [48]. Although the biological significance of cross-priming is a matter of debate [57], it seems likely that such spontaneously elicited CTL responses are induced through host APC cross-priming [8].
Interestingly, CTL responses against the MAGE-10254-262 HLA-A*02.01–restricted peptide are not only detectable in PBLs from cancer patients, but also in PBLs from healthy HLA-A2-positive donors. In our analyses of PBLs from 12 HLA-A2-positive healthy donors, TRAG-3 specific responses were detected in 2: against the strong binder T_45 and the intermediate binder T_57.10. The biological significance of these responses remains unresolved. CTL responses against the melanoma differentiation antigen MART-1 are similarly detectable in normal healthy donors as well as melanoma patients; however, MART-1–specific CTLs in healthy donors are characterized by naïve cell surface phenotype and incapacity to secrete INF-γ [39]. To our knowledge, no data is available on the phenotype of CTLs specific for CT antigens—either in cancer patients or healthy individuals—due to the low pre-cursor frequency in unstimulated PBLs.
Paclitaxel (Taxol) is a natural product derived from the bark of Taxus brevifolia, and taxanes represent one of the most important antitumor agents introduced in cancer chemotherapy over the past decade [52]. Taxanes inhibit microtubule depolymerization and demonstrate a broad spectrum of antitumor activity in various cancers, including cancers of the breast, ovary, and lung [21, 26, 47]. However, despite effective initial responses for these malignancies, paclitaxel treatment is rarely curative for the treatment of metastatic disease due to the development of paclitaxel resistance [41]. In fact, drug resistance represents a general characteristic observed in virtually every type of tumor (with few exceptions), with every known type of anticancer chemotherapeutic drug [25]. Several lines of evidence suggest that the development of drug resistance is associated with the expression of proteins not expressed in sensitive cells, underlining the potential of immunological targeting of proteins associated with drug resistance [15]. Evidence for a direct role of the TRAG-3 protein in paclitaxel resistance has not been provided, but in general, expression of CT antigens is up-regulated by demethylation [12], and alterations in the methylation status are a general characteristic of cancer cells in turn setting the stage for selection during chemotherapy [5]. Moreover, for other CT antigens (MAGE-1, MAGE-2, MAGE-3, and MAGE-4), and therefore possibly also TRAG-3, there is more frequent expression in metastatic lesions [7]. In this respect, all breast cancer patients included were late-stage patients, whereas some of the melanoma samples were from newly diagnosed patients. It could therefore be speculated that lesions from the breast cancer patients were more likely to be TRAG-3-positive compared with the melanoma lesions.
A recent study suggested that the induction of CTL responses correlates with binding; i.e., high-affinity peptides are more frequently recognized by host T cells [24]. In the present study, responses against the high-affinity binding peptide T_4 were detected in samples from seven patients, however, responses against the intermediately binding peptide T_57.10 were almost as frequent (Fig. 1). Surprisingly, the high-affinity peptides T_45, and T_58 were only recognized in three and four patients, respectively. These data indicate that other factors than binding affinity influence the specificity of the T-cell response. In this respect, it was recently shown that higher peptide binding affinity for HLA molecules does not necessarily equate with functional activity of the responding T cell [13, 20].
Detection of spontaneous TRAG-3–specific CTL responses in cancer patients clearly does not provide evidence that TRAG-3–derived peptides are processed and presented by cancer cells. Such evidence may be provided by elution of peptides from the surface of cancer cells [10]; however, in most cases the use of CTL clone cytoxicity assays is considered sufficient evidence for the presentation of the peptide in question [36]. In spite of the fact that in most cases production of INF-γ corresponds to cytotoxic potential, we attempted to expand TRAG-3–specific CTLs in sufficient numbers for cytotoxicity assays. However, these experiments were not successful. A recent study characterized the T_58 peptide, also described in the present study, and demonstrated that CTLs specific for this peptide were cytolytic against HLA-matched tumor targets expressing the TRAG-3 protein [56]. Clearly, these data support the notion of TRAG-3–derived peptides as targets for cytolytic T cells—a notion strengthened and extended in the present study. Moreover, our data suggest that the T_58 peptide is not the prominent natural target for anti-TRAG-3 CTL responses, although it could be speculated that the CTLs recognizing one of the peptides T_57.9, T_59.10, and T_58 may in fact react against all three peptides. In some patients, responses were detected against two or all three of these peptides, supporting this notion (Fig. 3, patients H2-MM, H3-LYM, and H5-LYM; and Fig. 4, patients M3-PBL and M5-PBL). However, in other patients, responses were detected against one of the peptides only, suggesting that some T cells (in some patients) cross-react, whereas others do not. Clearly, isolation and comparison of the clonotypic composition of cells responding against the respective peptides could provide the means to resolve this question [44].
In conclusion, our data demonstrate that several peptides from the TRAG-3 protein are targets for spontaneous T-cell responses in cancer patients. These peptides may be suited for future therapeutic vaccinations against cancer.
References
Andersen MH, thor Straten P (2002) Survivin—a universal tumor antigen. Pathol Histopathol 17(2):669–675
Andersen MH, Tan L, Sondergaard I, Zeuthen J, Elliott T, Haurum JS (2000) Poor correspondence between predicted and experimental binding of peptides to class I MHC molecules. Tissue Antigens 55(6):519–531
Andersen MH, Ostergaard Pedersen L, Becker JC, thor Straten P (2001) Identification of a cytotoxic T lymphocyte response to the apoptose inhibitor protein Survivin in cancer patients. Cancer Res 61:869–872
Anthony DD, Lehmann PV (2003) T-cell epitope mapping using the ELISPOT approach. Methods 29(3):260–269
Baylin SB, Herman JG, Graff JR, Vertino PM, Issa JP (1998) Alterations in DNA methylation: a fundamental aspect of neoplasia. Adv Cancer Res 72:141–196
Bilsborough J, Panichelli C, Duffour MT, Warnier G, Lurquin C, Schultz ES, Thielemans K, Corthals J, Boon T, van Der BP (2002) A MAGE-3 peptide presented by HLA-B44 is also recognized by cytolytic T lymphocytes on HLA-B18. Tissue Antigens 60(1):16–24
Brasseur F, Rimoldi D, Lienard D, Lethe B, Carrel S, Arienti F, Suter L, Vanwijck R, Bourlond A, Humblet Y et al (1995) Expression of MAGE genes in primary and metastatic cutaneous melanoma. Int J Cancer 63:375–380
Chen W, Masterman KA, Basta S, Mansour Haeryfar SM, Dimopoulos N, Knowles B, Bennink JR, Yewdell JW (2004) Cross-priming of CD8+ T cells by viral and tumor antigens is a robust phenomenon. Eur J Immunol 34(1):194–199
Chen Z, Zhu B, Wu Y (2002) Expression of TRAG-3 antigen in non-small-cell lung carcinomas. Lung Cancer 38(1):101–102
Clark RE, Dodi IA, Hill SC, Lill JR, Aubert G, Macintyre AR, Rojas J, Bourdon A, Bonner PL, Wang L, Christmas SE, Travers PJ, Creaser CS, Rees RC, Madrigal JA (2001) Direct evidence that leukemic cells present HLA-associated immunogenic peptides derived from the BCR-ABL b3a2 fusion protein. Blood 98(10):2887–2893
Coulie PG (2002) Cancer immunotherapy with MAGE antigens. Suppl Tumori 1(4):S63–S65
De Smet C, De Backer O, Faraoni I, Lurquin C, Brasseur F, Boon T (1996) The activation of human gene MAGE-1 in tumor cells is correlated with genome-wide demethylation. Proc Natl Acad Sci U S A 93(14):7149–7153
Dionne SO, Smith MH, Marincola FM, Lake DF (2003) Functional characterization of CTL against gp100 altered peptide ligands. Cancer Immunol Immunother 52(4):199–206
Duan Z, Feller AJ, Toh HC, Makastorsis T, Seiden MV (1999) TRAG-3, a novel gene, isolated from a taxol-resistant ovarian carcinoma cell line. Gene 229(1–2):75–81
Duan Z, Duan Y, Lamendola DE, Yusuf RZ, Naeem R, Penson RT, Seiden MV (2003) Overexpression of MAGE/GAGE genes in paclitaxel/doxorubicin-resistant human cancer cell lines. Clin Cancer Res 9(7):2778–2785
Feller AJ, Duan Z, Penson R, Toh HC, Seiden MV (2000) TRAG-3, a novel cancer/testis antigen, is overexpressed in the majority of melanoma cell lines and malignant melanoma. Anticancer Res 20(6B):4147–4151
Gabrilovich DI (2002) Dendritic cell vaccines for cancer treatment. Curr Opin Mol Ther 4(5):452–458
Godelaine D, Carrasco J, Lucas S, Karanikas V, Schuler-Thurner B, Coulie PG, Schuler G, Boon T, Van Pel A (2003) Polyclonal CTL responses observed in melanoma patients vaccinated with dendritic cells pulsed with a MAGE-3.A1 peptide. J Immunol 171(9):4893–4897
Gordan JD, Vonderheide RH (2002) Universal tumor antigens as targets for immunotherapy. Cytotherapy 4(4):317–327
Gross DA, Graff-Dubois S, Opolon P, Cornet S, Alves P, Bennaceur-Griscelli A, Faure O, Guillaume P, Firat H, Chouaib S, Lemonnier FA, Davoust J, Miconnet I, Vonderheide RH, Kosmatopoulos K (2004) High vaccination efficiency of low-affinity epitopes in antitumor immunotherapy. J Clin Invest 113(3):425–433
Hudis C (2002) Adjuvant use of taxanes for patients with breast cancer: we see the tip of the iceberg. Clin Breast Cancer 3(5):326–332
Juretic A, Spagnoli GC, Schultz-Thater E, Sarcevic B (2003) Cancer/testis tumour-associated antigens: immunohistochemical detection with monoclonal antibodies. Lancet Oncol 4(2):104–109
Karanikas V, Lurquin C, Colau D, van Baren N, De Smet C, Lethe B, Connerotte T, Corbiere V, Demoitie MA, Lienard D, Dreno B, Velu T, Boon T, Coulie PG (2003) Monoclonal anti-MAGE-3 CTL responses in melanoma patients displaying tumor regression after vaccination with a recombinant canarypox virus. J Immunol 171(9):4898–4904
Keogh E, Fikes J, Southwood S, Celis E, Chesnut R, Sette A (2001) Identification of new epitopes from four different tumor-associated antigens: recognition of naturally processed epitopes correlates with HLA-A*0201-binding affinity. J Immunol 167(2):787–796
Kerbel RS (2001) Molecular and physiologic mechanisms of drug resistance in cancer: an overview. Cancer Metastasis Rev 20(1–2):1–2
Khayat D, Antoine EC, Coeffic D (2000) Taxol in the management of cancers of the breast and the ovary. Cancer Invest 18(3):242–260
Marchand M, Weynants P, Rankin E, Arienti F, Belli F, Parmiani G, Cascelli N, Bourlond A, Vanwijck R, Humblet Y, Canon JL, Laurent C, Naeyaert JM, Plangne R, Deraemaeker R, Knuth A, Jäger E, Brasseur F, Herman J, Coulie PG, Boon T (1995) Tumor regression responses in melanoma patients treated with a peptide encoded by gene MAGE-3. Int J Cancer 63:883–885
Marchand M, van Baren N, Weynants P, Brichard V, Dreno B, Tessier MH, Rankin E, Parmiani G, Arienti F, Humblet Y, Bourlond A, Vanwijck R, Lienard D, Beauduin M, Dietrich PY, Russo V, Kerger J, Masucci G, Jager E, De Greve J, Atzpodien J, Brasseur F, Coulie PG, van der Bruggen P, Boon T (1999) Tumor regressions observed in patients with metastatic melanoma treated with an antigenic peptide encoded by gene MAGE-3 and presented by HLA-A1. Int J Cancer 80(2):219–230
Marchand M, Weynants P, Rankin E, Arienti F, Belli F, Parmiani G, Cascinelli N, Bourlond A, Vanwijck R, Humblet Y (1995) Tumor regression responses in melanoma patients treated with a peptide encoded by gene MAGE-3 (letter). Int J Cancer 63(6):883–885
Nestle FO, Alijagic S, Gilliet M, Sun Y, Grabbe S, Dummer R, Burg G, Schadendorf D (1998) Vaccination of melanoma patients with peptide- or tumor lysate-pulsed dendritic cells. Nat Med 4(3):328–332
Parmiani G, Rivoltini L, Andreola G, Carrabba M (2000) Cytokines in cancer therapy. Immunol Lett 74(1):41–44
Parmiani G, Castelli C, Dalerba P, Mortarini R, Rivoltini L, Marincola FM, Anichini A (2002) Cancer immunotherapy with peptide-based vaccines: what have we achieved? Where are we going? J Natl Cancer Inst 94(11):805–818
Pass HA, Schwarz SL, Wunderlich JR, Rosenberg SA (1998) Immunization of patients with melanoma peptide vaccines: immunologic assessment using the ELISPOT assay. Cancer J Sci Am 4(5):316–323
Rabinowich H, Banks M, Reichert TE, Logan TF, Kirkwood JM, Whiteside TL (1996) Expression and activity of signaling molecules in T lymphocytes obtained from patients with metastatic melanoma before and after interleukin 2 therapy. Clin Cancer Res 2(8):1263–1274
Rammensee HG, Weinschenk T, Gouttefangeas C, Stevanovi ES (2002) Towards patient-specific tumor antigen selection for vaccination. Immunol Rev 188(1):164–176
Renkvist N, Castelli C, Robbins PF, Parmiani G (2001) A listing of human tumor antigens recognized by T cells. Cancer Immunol Immunother 50(1):3–15
Reynolds SR, Zeleniuch-Jacquotte A, Shapiro RL, Roses DF, Harris MN, Johnston D, Bystryn JC (2003) Vaccine-induced CD8+ T-cell responses to MAGE-3 correlate with clinical outcome in patients with melanoma. Clin Cancer Res 9(2):657–662
Riley JP, Rosenberg SA, Parkhurst MR (2003) Stimulation of tumor-reactive T lymphocytes using mixtures of synthetic peptides derived from tumor-associated antigens with diverse MHC binding affinities. J Immunol Methods 276(1–2):103–119
Romero P, Valmori D, Pittet MJ, Zippelius A, Rimoldi D, Levy F, Dutoit V, Ayyoub M, Rubio-Godoy V, Michielin O, Guillaume P, Batard P, Luescher IF, Lejeune F, Lienard D, Rufer N, Dietrich PY, Speiser DE, Cerottini JC (2002) Antigenicity and immunogenicity of Melan-A/MART-1 derived peptides as targets for tumor reactive CTL in human melanoma. Immunol Rev 188(1):81–96
Rosenberg SA, Yang JC, Schwartzentruber DJ, Hwu P, Marincola FM, Topalian SL, Restifo NP, Dudley ME, Schwarz SL, Spiess PJ, Wunderlich JR, Parkhurst MR, Kawakami Y, Seipp CA, Einhorn JH, White DE (1998) Immunologic and therapeutic evaluation of a synthetic peptide vaccine for the treatment of patients with metastatic melanoma. Nat Med 4(3):321–327
Sangrajrang S, Fellous A (2000) Taxol resistance. Chemotherapy 46(5):327–334
Scanlan MJ, Gure AO, Jungbluth AA, Old LJ, Chen YT (2002) Cancer/testis antigens: an expanding family of targets for cancer immunotherapy. Immunol Rev 188(1):22–32
Scanlan MJ, Simpson AJ, Old LJ (2004) The cancer/testis genes: review, standardization, and commentary. Cancer Immun 4:1
Schrama D, Andersen MH, Terheyden P, Schrøder L, Ostergaard Pedersen L, thor Straten P, Becker JC (2001) Oligoclonal TCR usage of melanocyte differentiation antigen-reactive T cells. Cancer Res 61:493–496
Schuler G, Schuler-Thurner B, Steinman RM (2003) The use of dendritic cells in cancer immunotherapy. Curr Opin Immunol 15(2):138–147
Schultze JL, Vonderheide RH (2001) From cancer genomics to cancer immunotherapy: toward second-generation tumor antigens. Trends Immunol 22(9):516–523
Simon GR, Bunn PA, Jr (2003) Taxanes in the treatment of advanced (stage III and IV) non-small cell lung cancer (NSCLC): recent developments. Cancer Invest 21(1):87–104
Valmori D, Dutoit V, Lienard D, Rimoldi D, Pittet MJ, Champagne P, Ellefsen K, Sahin U, Speiser D, Lejeune F, Cerottini JC, Romero P (2000) Naturally occurring human lymphocyte antigen-A2 restricted CD8+ T-cell response to the cancer testis antigen NY-ESO-1 in melanoma patients. Cancer Res 60(16):4499–4506
Valmori D, Dutoit V, Rubio-Godoy V, Chambaz C, Lienard D, Guillaume P, Romero P, Cerottini JC, Rimoldi D (2001) Frequent cytolytic T-cell responses to peptide MAGE-A10(254–262) in melanoma. Cancer Res 61(2):509–512
van der Bruggen P, Traversari C, Chomez P, Lurquin C, De Plaen E, Van den Eynde B, Knuth A, Boon T (1991) A gene encoding an antigen recognized by cytolytic T lymphocytes on a human melanoma. Science 254:1643–1647
van der Bruggen P, Zhang Y, Chaux P, Stroobant V, Panichelli C, Schultz ES, Chapiro J, Van den Eynde BJ, Brasseur F, Boon T (2002) Tumor-specific shared antigenic peptides recognized by human T cells. Immunol Rev 188(1):51–64
Wolff AC (2001) Systemic therapy. Curr Opin Oncol 13(6):436–449
Wu YZ, Zhao TT, Ni B, Zou LY, Liu HL, Zhu B (2003) Expression of TRAG-3 in breast cancer. Int J Cancer 107(1):167–168
Yee C, Greenberg PD (2002) Modulating T-cell immunity to tumours: new strategies for monitoring T-cell responses. Nat Rev Cancer 2(6):409–419
Zendman AJ, Ruiter DJ, van Muijen GN (2003) Cancer/testis-associated genes: identification, expression profile, and putative function. J Cell Physiol 194(3):272–288
Zhu B, Chen Z, Cheng X, Lin Z, Guo J, Jia Z, Zou L, Wang Z, Hu Y, Wang D, Wu Y (2003) Identification of HLA-A*0201-restricted cytotoxic T lymphocyte epitope from TRAG-3 antigen. Clin Cancer Res 9(5):1850–1857
Zinkernagel RM (2002) On cross-priming of MHC class I-specific CTL: rule or exception? Eur J Immunol 32(9):2385–2392
Acknowledgements
This work was supported by the EU project “European Searchable Tumour Cell line Database” (ESTDAB), (QLRI-CT-2001-01325), and by grants from The Novo Nordisk Foundation, The Danish Cancer Society, The Danish Research Council, Danish Foundation for Cancer Research, and the Julie von Müllens fund. We thank Professor A. Svejgaard and Ms Bodil K. Jakobsen, Department of Clinical Immunology, University Hospital, Copenhagen, for HLA-typing of patient blood samples.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meier, A., Reker, S., Svane, I.M. et al. Spontaneous T-cell responses against peptides derived from the Taxol resistance–associated gene-3 (TRAG-3) protein in cancer patients. Cancer Immunol Immunother 54, 219–228 (2005). https://doi.org/10.1007/s00262-004-0578-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-004-0578-9