Abstract
This study prospectively correlated the level of expression of CD55 on tumours with 7-year survival in 136 colorectal cancer patients. Patients with tumours expressing high levels of CD55 had a significantly worse survival (24%) than patients with low CD55 levels (50%, p<0.02). A similar difference was seen for patients (Duke's B or C) with a high risk of recurrence (29% vs 58%, p<0.05). Furthermore, there was a progressive deterioration in prognosis with increasing antigen expression (p=0.01). It remains unclear if CD55 is overexpressed by tumours to protect them from complement or if it is related to the recent observation that CD55 is a ligand for the T-cell activation antigen CD97. However, it is a marker of aggression, as colorectal cancer patients whose tumours overexpress CD55 have a significantly reduced 7-year survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although colorectal cancer incidence and mortality rates have declined over the past decade these changes are not universal [4], and it is the second or third commonest cause of cancer death in most developed countries. A large proportion of colorectal cancer patients will develop metastases after attempted curative surgery. Those at significant risk of recurrence are those with tumours extending beyond the muscularis propria (the majority of colorectal cancers) and subdivision of this large group is principally dependent on the presence of lymph node involvement (Duke's B or C lesions). However, there is still considerable uncertainty in outcome within these stages as some stage B patients do poorly whereas some stage C patients do very well. A prognostic marker used in conjunction with Duke's staging may more accurately predict the outcome and need for adjuvant therapy, as in breast cancer where the combination of lymph node status and oestrogen receptor measurement is used to guide adjuvant therapy.
Recently a human anti-idiotypic antibody 105AD7, which mimics the tumour-associated antigen 791Tgp72, has been used as a vaccine in colorectal cancer patients. In a neoadjuvant setting, increased infiltration of CD4 cells expressing the activation receptor CD25 [11] and NK cells [6] was observed in 105AD7 immunised as compared with unimmunised patients. Furthermore, there was a three-fold increase in tumour cell apoptosis in the immunised patients [1]. 791Tgp72 is an integral membrane glycoprotein, and flow cytometric studies have shown that it is expressed by a high proportion of tumour cells from primary colorectal cancers [7]. By extensive clinical localisation studies, this expression has been shown to be functionally selective with the monoclonal antibody 791T/36 [2]. 791Tgp72 antigen has recently been cloned and was shown to be identical to CD55 [15]. CD55 is a complement regulatory protein that binds to C3 convertases of both the classical and alternative complement pathways and protects cells against bystander attack from complement. It is composed of four external small consensus repeats and is GPI-anchored to the cell membrane. The level of expression of CD55 varies widely on colorectal tumours, with at least 75% of tumour showing enhanced levels compared with normal cells [9]. The level of CD55 expression on colorectal tumour cells was, therefore, quantified using the monoclonal antibody 791T/36, which binds to SCR1 and 2 of CD55. Expression was then correlated prospectively with 7-year survival to determine if CD55 could confer a selective advantage for tumour growth and be used to identify patients at risk of recurrence.
Materials and methods
Cells
Fresh tumour specimens were obtained at the time of colorectal cancer resection from 136 patients. Specimens were finely minced and disaggregated with 0.05% collagenase (Type IV, Boehringer Mannheim, Lewes, UK) for 20 min at 37°C. The tumour cell suspension was removed and washed three times in Hanks balanced salt solution (Gibco BRL, Paisley, UK). Fresh collagenase was added to the remaining tissue and it was reincubated for a further 20 min. This procedure was repeated twice before combining cells from all dissociations and resuspending them in Dulbecco's medium containing 20% fetal calf serum (Gibco). Previous studies on 791T cells that express CD55 and on purified CD55 have shown that this antigen is not cleaved by collagenase (unpublished results).
Normal mucosa was obtained at the margin of the resected bowel. Mucosa was stripped from the underlying mucosa layer and disaggregated in 0.05% collagenase for 20 min at 37°C.
CD55 immunofluorescence
Tumour cells were incubated for 1 hr at 4°C with 791T/36 mouse monoclonal antibody. Cells were washed twice and incubated for a further hour with fluorescein isothiocyanate conjugated rabbit antimouse immunoglobulin (Dako, Bucks., UK). Normal mouse immunoglobulin was used as a negative control and this fluorescence was subtracted from the fluorescence obtained with 791T/36. The cells were washed three times prior to analysis on a FACS IV (Becton Dickinson, Sunnyvale, CA) as previously described. Results are expressed as mean linear fluorescence (MLF) as the results were measured with linear amplification. The flow cytometer was always precalibrated with florescent heads. An MLF of 100 indicated 2×103 molecules of antigen [7].
Disaggregation of solid tumours yields a mixed population of cells including red blood cells, lymphocytes, stromal cells, macrophages, and endothelial cells. The percentage of epithelial cells as measured by staining of cytokeratin monoclonal antibody Cam 5.2 was only 22±13% (range 10–60). However, following forward angle light scatter gating to selectively analyse cells in the malignant cell size range, 79±4% (range 69–86) of the cells analysed were epithelial. Furthermore, the variation between tumours was considerably reduced.
The percentage of leukocytes as measured by staining with the anti-CD45 monoclonal antibody F-10–89 in the total nucleate population was 74±16 (range 40–90). This was considerably reduced to 5.5±5% (range 1–20) following FACS IV gating for malignant size. The percentage of stromal cells in the population of cells analysed in the malignant size range was 3.5±3% (range 1–13).
Follow-up
The patients in this study had colorectal cancer resections performed by the department of surgery, University Hospital Nottingham. At operation, the tumour site, the surgeon's estimate of curability, pathological stage, and grade were all entered prospectively into a computerised database. Patients were followed up every 3–6 months in a dedicated colorectal clinic for a minimum of 7 years. None of the patients received any further therapy for their colorectal tumours. Only two patients were lost to follow-up and both were censored in their third year. Those alive at the time of the analysis had a median follow-up of 89 months. Survival was taken as the time from operation to colorectal cancer–related death. Patients known to have died from other causes were censored at the time of death. Patients dying in the immediate postoperative period (<30 days) were excluded, as these deaths were related to postoperative complication and are unlikely to be influenced by CD55 expression on the resected tumour. These tumours had a similar distribution of CD55 expression to the other tumours in the study.
Statistics
Statistical analysis was performed using Kaplan-Meier survival curves using a log rank test to test for survival difference. A linear association between survival and antigen expression was analysed by a Mantel-Haenszel test.
Results
Tumours were obtained from 136 consecutive patients in a single colorectal cancer centre. There was a 3:2 ratio of male to female with a median age of 68 (range 47–87). The number of rectal, caecal, and sigmoid cancers were comparable. The majority of cancers were of moderate differentiation and 12% were Duke's A, 41% Duke's B, 21% Duke's C, and 26% modified Duke's D. There were slightly higher number of Duke's B than in a normal population as this centre is a referral centre for population screening for colorectal cancer.
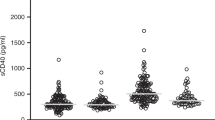
The level of CD55 expression was quantified on the cell surface of freshly disaggregated colorectal tumour cells by immunofluorescence staining and flow cytometric analysis. Although there was intertumour variation in the number of cells stained with 791T/36, an average of 67±17% of cells within the malignant gate were stained. There was wide intratumour variation in staining of colorectal tumours with histograms showing a broad normally distributed peak. The results were therefore summarised as a mean for the 10,000 cells analysed. There was also a wide range in the levels of CD55 expressed between tumours (Fig. 1a). Five percent of tumours failed to express any CD55, and 12% had levels similar to normal mucosa. Twenty-five percent of patients had a modest (2–3-fold) increase in CD55 expression as compared with normal mucosa, whereas a further 25% had a 3–9-fold increase. The remaining patients had large and variable increases in CD55 expression (10–67 fold). The mean level of expression for all patients was 233 (range 0–2,020). Interestingly, there was no correlation between CD55 expression and tumour stage (Fig. 1b) with mean level of expression for Duke's A–D being 151, 261, 198, and 230, respectively. There was also no correlation with tumour site or differentiation (results not shown).
a Freshly isolated tumours and normal mucosa from the resection were disaggregated by collagenase treatment, stained by indirect immunofluorescence with 791T/36 monoclonal antibody, and analysed by flow cytometry. b Freshly isolated tumours were disaggregated by collagenase treatment, stained by indirect immunofluorescence with 791T/36 monoclonal antibody, and analysed by flow cytometry. Modified Duke's staging where D denotes patients with distant metastases
One hundred thirty-six patients were entered into the study and followed up in dedicated clinics for 7 years. Fifteen patients were lost to follow-up and 16 died of either non-colorectal cancer–related deaths or due to postoperative complications. The remaining 105 patients were studied. Seven-year survival for all patients with different Duke's stages is shown in Table 1. The overall 7-year survival for all patients was 41%. However, patients whose tumours expressed CD55 at levels greater than the mean (233) had significantly worse (p<0.02) survival (24%) when compared with patients whose tumours expressed less than the mean levels (50%). More importantly there was significantly poorer survival for patients overexpressing CD55 (MLF>233, p=0.05) even in patients at increased risk of recurrence (Duke's B and C). Kaplan-Meier plots clearly show a significantly (log rank p=0.001) poorer survival rate at all time points for patients whose tumours overexpress CD55 (Fig. 2). To further investigate the correlation between CD55 expression on tumours and patient survival, patients were divided into quartile ranges for increasing expression of CD55 (Table 2). Patients whose tumours lacked or had similar levels of CD55 to normal mucosa had a high survival rate of 58%. Patients whose tumours had a modest 2–3-fold increase in CD55 had a survival rate of 50%, patients with a 3–9-fold increase had a survival rate of 38%, and those with a 10–65-fold increase had a poor survival rate of 26%. There was, therefore, a progressive and significant deterioration in prognosis with increasing CD55 expression when analysed by a Mantel-Haenszel test for linear association (p=0.01).
Discussion
There is accumulating evidence that adjuvant chemotherapy may improve survival in selected colorectal cancer patients with a poor prognosis [12]. Similarly many new biological and immunotherapies are being developed to prevent recurrence following surgery. However, it remains unclear as to which patients would benefit from further therapy. It is current practice to offer chemotherapy to all Duke's C patients. Although the majority of Duke's A and B patients will be cured by surgery, there are some patients that would benefit from further therapy. Similarly, at least one third of Duke's C patients are cured by surgery and, therefore, undergo unnecessary and potentially dehabilitating further treatments. If additional markers could be added to Duke's staging, such as oestrogen receptor status in breast cancer, it may be possible to select patients for aggressive adjuvant therapy.
Other colorectal tumour markers have been studied in an attempt to predict survival. The pattern of p53 and 5T4 tumour staining has been used with varying results [3, 16]. Similarly the degree and type of lymphocytic infiltration has been characterised. Although overt skeletal metastases are uncommon in colorectal cancer, it has recently been shown that the presence of tumour cells in the bone marrow is an independent prognostic indicator of a shorter disease-free survival [10]. All these studies currently depend upon immunohistochemical staining, and slides have to be interpreted by a skilled pathologist. These methods are at best semiquantitative and may suffer from intraobserver variation. The use of FACS assays in this study has allowed the objective quantification of CD55 expression. In addition, the technique should have less sampling error as one third of the tumour is disaggregated and a representative sample of 105 cells stained and analysed. This is very important, as intratumour variation in antigen expression is common in colorectal cancer.
CD55 is a complement regulatory protein that is expressed by a wide variety of cells that are exposed to bystander complement attack [14]. These cells include blood cells, endothelial cells, and surface epithelial cells. It is, therefore, not surprising that colorectal adenocarcinomas of epithelial origin also express CD55. What was surprising, however, was the large variation in levels of expression of CD55 on tumours. Some tumours failed to express any CD55, as assessed by binding to the monoclonal antibody 791T/36, whereas some expressed a 65-fold increase over the levels on normal cells. It was of further interest that the tumours expressing high levels were apparently more aggressive as patients with tumours expressing these levels had a significantly reduced 7-year survival (26%) compared with those with tumours expressing either normal levels (50%) or failing to express CD55 (58%).
It may have been predicted that loss of CD55 may have made tumours more susceptible to complement-mediated lysis and that overexpression would protect cells. In contrast, tumours with low expression are less aggressive than tumours that overexpress CD55. This may be related to the observation that CD55 on T cells results in enhanced proliferation [5]. Perhaps signalling via CD55 on tumours also results in enhanced proliferation? Alternatively, it may be related to the observation that CD55 is a ligand for CD97, a protein expressed by activated leukocytes [8]. Overexpression of CD55 may make tumours susceptible to T-cell attack. However, we have shown that strong cell surface expression of CD55 on colorectal tumours is associated with high levels of CD55 deposited within tumour stroma [9]. We have shown that CD55 within extracellular matrix is functional and can be released in a soluble form by MMP-7 [13]. Perhaps extracellular CD55 acts as a dereceptor and inhibits both complement activation and interaction with CD97. In this context we have recently shown that soluble CD55 can inhibit cytokine secretion by a T-cell clone and this inhibition can be reversed with antibodies which block CD55/CD97 interaction (unpublished results).
Whatever the reason for CD55 overexpression by tumours, its level may act as an independent prognostic indicator allowing a further classification of Duke's B and C patients who may benefit from further therapy.
References
Amin S, Robins RA, Maxwell-Armstrong C, Scholefield J, Durrant LG (2000) Vaccine induced apoptosis: a novel clinical trial endpoint? Cancer Res 60(12):3132–3136
Armitage NC, Perkins AC, Pimm MV, Farrands PA, Baldwin RW, Hardcastle JD (1984) Localization of an anti-tumour monoclonal antibody (791T/36) in gastrointestinal tumors. Br J Surg 71(6):407–412
Bosari S, Viale G, Bossi P, Maggioni M, Coggi G, Murray JJ, Lee AK (1994) Cytoplasmic accumulation of p53 protein: an independent prognostic indicator in colorectal carcinomas. J Natl Cancer Inst 86:681–687
Chu KC, Tarone RE, Chow W et al (1994) Temporal patterns in colorectal cancer incidence, survival and mortality from 1950 through 1990. J Natl Cancer Inst 86:997–1006
Davis LS, Patel SS, Atkinson JP, Lipsky PE (1988) Decay accelerating factor functions as a signal transducing molecule for human T cells. J Immunol 141:2246–2252
Durrant LG, Armstrong CM, Buckley D, Amin S, Robins RA, Carmichael JC et al (2000) A neoadjuvant clinical trial in colorectal cancer patients of the human anti-idiotypic antibody 105AD7, which mimics CD55. Clin Cancer Res 62(2):422–430
Durrant LG, Robins RA, Baldwin RW (1989) Flow cytometric screening of monoclonal antibodies for drug or toxin targeting to human cancer. J Natl Cancer Inst 81:688–695
Hamann J, Vogel B, Vanschijndel GMW, Vanlier RAW (1996) The 7-span transmembrane receptor CD97 has a cellular ligand (CD55, DAF) J Exp Med 184(3):1185–1189
Li L, Spendlove I, Morgan J, Durrant LG (2000) CD55 is overexpressed in the tumour environment. Br J Cancer 84(1):80–86
Lindemann F, Schlimok G, Dirschedl P et al (1992) Prognostic significance of micrometastatic tumour cells in the bone marrow of colorectal cancer patients. Lancet 340:685–689
Maxwell-Armstrong CA, Durrant LG, Robins RA, Galvin AM, Scholefield JH, Hardcastle JD (1999) Increased activation of lymphocytes infiltrating primary colorectal cancers following immunisation with the anti-idiotype monoclonal antibody 105AD7. Gut 45:593–598
Moertel CG, Fleming TR, Macdonald JS et al (1990) Levamisole and fluorouracil for adjuvant therapy of resected colon cariconmas. N Engl J Med 322:352–358
Morgan J, Spendlove I, Durrant LG (2002) The role of CD55 in protecting the tumour environment from complement attack. Tissue Antigens 60(3):213–223
Nicholson-Weller A, Wang C (1994) Structure and function of decay-accelerating factor CD55. J Lab Clin Med 123(4):485–491
Spendlove I, Li L, Carmichael J, Durrant LG (1999) Decay accelerating factor (CD55): a target for cancer vaccines? Cancer Res 59(10):2282–2286
Starzynska T, Marsh PJ, Scholfield PF et al (1994) Prognostic significance of 5T4 oncofetal antigen expression in colorectal adenocarcinomas. Br J Cancer 69:899–902
Acknowledgements
This work was supported by the Cancer Research Campaign, UK, with a programme grant, no. SP2220/0501.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Durrant, L.G., Chapman, M.A., Buckley, D.J. et al. Enhanced expression of the complement regulatory protein CD55 predicts a poor prognosis in colorectal cancer patients. Cancer Immunol Immunother 52, 638–642 (2003). https://doi.org/10.1007/s00262-003-0402-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-003-0402-y