Abstract
We have previously reported that Fms-like tyrosine kinase-3 ligand (flt3-L) induced tumor stabilization and regression of palpable ectopic prostate tumors (TRAMP-C1). Although some mice remained "tumor free" for several months following termination of therapy, tumors invariably reappeared and grew progressively in all animals. The lack of a curative response suggests that TRAMP-C1 tumors may inhibit the development of a flt3-L-induced anti-tumor immune response. Consistent with this view, we demonstrate herein that TRAMP-C1 tumors isolated from flt3-L treated animals contained a marked dendritic cell (DC) infiltrate that was temporally correlated with tumor regression. However, tumor-associated DCs, especially in a flt3-L setting, progressively lost MHC class II antigen expression during tumor growth. Treatment with the DC maturation factor trimeric CD40 ligand (CD40-L) either alone or in combination with fl3-L neither prevented loss of DC class II antigens nor disease relapse. Because loss of class II antigens would prevent CD4+ helper T (Th) cell development, we treated tumor-bearing mice with agonistic anti-4-1BB antibody (Ab), which can promote cytotoxic T lymphocyte (CTL) development independent of Th cell function. However, anti-4-1BB Ab alone did not alter TRAMP-C1 growth kinetics, and, when used in combination, was no more effective than flt3-L alone. The inability of the 4-1BB co-stimulatory signal to promote tumor regression may have been related to two additional features of TRAMP-C1 tumors. First, tumor-associated T cells, but not splenic T cells from tumor-bearing animals, were profoundly deficient in expression of CD3-epsilon (CD3ε) and T cell receptor-beta chain (TCRβ). Second, CTLs required 24 h to efficiently kill TRAMP-C1 target cells even after up-regulation of MHC class I antigens by interferon-γ. This rate of tumor cell destruction by CTLs may not be sufficient to prevent tumor progression. Taken together, these data reveal several important immunosuppressive characteristics of the prostate tumor microenvironment (TME) that immunotherapeutic interventions must first overcome to achieve long-term cures. These data also highlight the importance of utilizing treatment versus vaccination models in the evaluation of immunotherapeutic modalities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Advances in understanding how the immune system is regulated rekindled interest in immunotherapy as a treatment modality for localized and metastatic cancers. Animal studies have demonstrated that a number of immunotherapeutic approaches can induce anti-tumor immunity and prevent tumor growth of weakly immunogenic tumors [9, 40]. This success has justified phase I and II clinical trials which, unfortunately, have reported only partial responses in humans [33, 38]. The disappointing response in clinical trials may be related to the nature of the pre-clinical animal models used to assess the efficacy of immunotherapeutic agents or strategies. Immunotherapeutic modalities have been evaluated largely in prevention or vaccination models that do not accurately reflect clinical reality. Thus, there is a critical need to develop treatment models where different immune-based strategies can be evaluated in a clinically relevant setting.
In view of these considerations, we developed a treatment animal model for prostate cancer using a syngeneic cell line (TRAMP-C1) derived from a prostate tumor isolated from TRAMP (transgenic adenocarcinoma of mouse prostate) mice [10, 14]. Utilizing this model, we reported that C57Bl/6 mice injected with TRAMP-C1 cells developed progressively growing tumors approximately 1 month after transplantation. Immunotherapeutic intervention when tumors were palpable (~30 days post implantation) with flt3-ligand (flt3-L), a haematopoetic growth factor for both myeloid and lymphoid precursors [2], induced a dose-dependent tumor regression response and prolonged survival [6]. This was achieved despite down-regulation of MHC class I molecules by TRAMP-C1 cells, a common occurrence with human tumors, including prostate cancer [15, 23, 36]. Although some regressor mice remained "tumor free" for several months, termination of therapy was invariably associated with disease relapse.
Studies by Gaiger and colleagues [11] have recently demonstrated that TRAMP-C1 cells over-express Wilms' tumor gene transcription factor (WT1) at the mRNA level and this protein can be detected in TRAMP-C1 cells by immunohistochemistry (unpublished observation). WT1 functions as a tumor antigen because immunization with purified WT1 protein generated cytotoxic T cells (CTLs) that recognized a class I restricted immunodominant peptide expressed on TRAMP-C1 tumor cells. In humans, leukemic CD34+ progenitor cells can be selectively eliminated by cytotoxic T lymphocytes (CTLs) specific for WT1 [12]. Similar to human tumor antigens, WT1 appears to be a relatively weak antigen because immunization with irradiated TRAMP-C1 cells can significantly inhibit TRAMP-C1 tumor growth, but fail to provide long-term protection (unpublished observation). Thus, TRAMP-C1 cells express a well-characterized, relatively weak but naturally processed tumor antigen. This model therefore provides an opportunity to examine tumor/host cell interactions that may contribute to disease relapse following an immune-based therapy.
In this report we present evidence consistent with the view that flt3-L induced both inflammatory (innate) and adaptive immune responses that contributed to prostate tumor growth inhibition. However, residence within the prostate tumor microenvironment (TME) was associated with disruption of the T cell receptor (TCR) and CD3 signaling complex as well as loss of MHC class II molecules on dendritic cells (DCs) required for tumor antigen presentation. Combination flt3-L immunotherapy with either soluble CD40-L or agonistic anti-4-1BB Ab failed to prevent these TME-induced alterations or promote long-term cures.
Materials and methods
Mice, cell lines and reagents
Seven- to 8-week-old BALB/c and C57BL/6 (B6) male mice were purchased from Charles River Laboratories, Wilmington, Mass. and experiments carried out in accordance with the principles of laboratory animal care (NIH publication no. 85-23, revised 1985). B6.12987- Rag1 tm1Mom ( Rag1 -1-) mice were obtained from Jackson Laboratories, Bar Harbor, Me., and were maintained in a sterile environment and fed sterile food and water ad libitum. The parental transplantable epithelial prostate cancer cell line, TRAMP-C1, derived from a prostate adenocarcinoma in transgenic C57BL/6 mice [10], was kindly provided by Dr. Norman Greenberg (Baylor College of Medicine, Houston, Texas). TRAMP-C1 were cultured in DMEM supplemented with 5% fetal bovine serum, 5% NuSerum IV (Collaborative Biomedical Products, Bedford, Mass.), L-glutamine (2 mM), 5 ug/ml insulin and 0.01 nM dihydrotestosterone. P815 mastocytoma (H-2 d), YAC-1 lymphoma (H-2 k/d), B10.2 fibrosarcoma (H-2 b) and MKSA fibroblast (H-2 d) cell lines were maintained by bi-weekly passage in RPMI 1640 tissue culture media supplemented with 5% FBS, L-glutamine (2 mM) and penicillin/streptomycin. Human flt3-L, trimeric CD40-L and anti-4-1BB (M6, rat IgG2a) monoclonal antibody (mAb) were kindly provided by Immunex Corporation (Seattle, Wash.) and diluted in carrier [0.1% normal sterile mouse serum (NMS) in PBS]. Recombinant mouse IFN-γ was obtained from PeproTec Inc., Rocking Hill, N.J.
Animal treatment model
B6 mice were injected intradermally with 5×106 TRAMP-C1 tumor cells in the anterior chest wall. When tumors were palpable (~30 days post implantation), animals were treated subcutaneously (s.c.) with either carrier or flt3-L (30 μg/day). Unless indicated otherwise, treatments were for 21 consecutive days. When used in combination with flt3-L, CD40-L (50 μg/dose) was administered s.c. on days 14–21 of flt3-L treatment, whereas anti-4-1BB mAb (200 μg/dose) was injected intraperitoneally on days 3 and 6 of flt3-L treatment. Tumor volumes were monitored twice weekly as previously described [6]. Some tumors from cohorts were excised during (days 7, 14, 21) and after (day 28) flt3-L treatment, subjected to enzyme digestion [6] and tumor infiltrating leukocytes (TILs) isolated by ficoll centrifugation for phenotypic characterization.
Flow cytometry
At various time points during and after treatments, TILs isolated from digested TRAMP-C1 tumors were phenotyped by two- and three-color flow cytometry. Spleen cells from non-tumor-bearing animals were used as positive controls and negative gates set using isotype-matched antibodies. All primary and secondary antibodies used in these studies were obtained from PharMingen, San Diego, Calif., and were used according to the manufacturer's instructions
Cytotoxicity and DNA fragmentation assays
Natural killer (NK) cell and CTL activity was evaluated using a standard 51Cr-release assay as previously described [4]. Alloreactive CTLs were generated in vitro by co-culture of normal BALB/c spleen cells with mitomycin C-treated B6 spleen cells [5]. Target cells were labeled with 51Cr (New England Nuclear, Boston, Mass.) and then incubated with effector cells at the indicated effector/target cell ratios for either 4 or 24 h. The amount of isotope released in the supernatant was determined by liquid scintillation counting and the percent net release calculated [5]. In some experiments, effector and target cells were mixed with different concentrations of concanavalin A (Con A) (Sigma Chemical Co., St. Louis, Mo.) to determine if TRAMP-C1 cells could be killed in a lectin-dependent CTL assay. To verify that isotope release reflected cellular death, fragmentation of target cell DNA was evaluated following published procedures with slight modifications [28]. Briefly, target cells were labeled for 48 h with 3H-thymidine and then incubated with BALB/c anti-B6 spleen cells overnight. The following day cells were pelleted and samples of the supernatant removed as fraction M. Ice-cold lysis buffer (25 mM sodium acetate, pH 6.6) was added to the pellets and the samples incubated for 1 h on ice. The lysate was centrifuged (13,000× g, 15 min), the supernatant harvested (fraction S) and the pellet resuspended in 0.2 ml PBS (fraction P). The extent of DNA fragmentation was expressed as percent specific fragmentation calculated using the following formula:
Results
Flt3-L and the innate and adaptive immune response
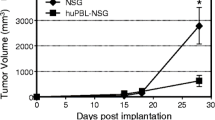
We have previously reported that flt3-L treatment of mice bearing ectopic TRAMP-C1 tumors induced a marked growth inhibition during therapy; however, tumor progression ensued following termination of treatment. Although treatment with 10 μg/dose for 21 days delayed TRAMP-C1 growth, the 30 μg/dose regimen was clearly more efficacious, because tumors uniformly regressed and many animals remained tumor-free for months, an outcome not obtained with the lower dose [6]. TRAMP-C1 tumors do not express receptors for flt3-L and high doses of flt3-L did not inhibit TRAMP-C1 proliferation in vitro (unpublished observation), suggesting that tumor growth inhibition was mediated indirectly by augmenting anti-tumor immunity. Therefore, to assess the contribution of innate versus adaptive immunity during flt3-L-induced tumor regression, T and B deficient (RAG-1-deficient, Rag-1-/-) mice bearing ectopic TRAMP-C1 tumors were injected with either carrier or flt3-L and tumor volumes determined during therapy. Figure 1A and B shows that in carrier-treated mice, TRAMP-C1 tumor growth was much more rapid in immunodeficient mice than normal B6 mice. However, Flt3-L did inhibit modestly TRAMP-C1 tumor growth in Rag-1—1-mice, suggesting a contribution by the innate immune response. It should be noted that this represented only a partial response, because tumor volumes of intact mice given flt3-L therapy were greatly reduced relative to Rag-/-mice given the same treatment (note different scales in Fig. 1A and B).
Flt3-L treatment partially inhibits tumor growth in Rag-1-deficient mice. Wild type ( A) or Rag-1-deficient mice ( B) were injected intradermally with TRAMP-C1 cells and when mice had palpable tumors, treated with either carrier ( open symbols) or flt3-L ( closed symbols). After 20 days of therapy, mice were killed and their final tumor volumes determined. Values represent mean tumor volumes ± S.D. of 4–5 mice/group. Arrows in both panels indicate when therapy was initiated and terminated. Note the different scales in A and B
These results and the observation that flt3-L does not directly inhibit TRAMP-C1 growth in vitro (data not presented), suggest that flt3-L augments both innate and adaptive immunity to TRAMP-C1 tumors. Consistent with this view, we previously reported that flt3-L induced a pronounced mixed inflammatory cell infiltrate into TRAMP-C1 tumors detectable by histological and immunohistochemical analysis ([6] and data not shown). To better characterize this infiltrate, mice with pre-existing TRAMP-C1 tumors were treated with either carrier or flt3-L and at the indicated times post implantation, TILs were isolated and stained with a panel of cell-type specific antibodies. Cells were also labeled with propidium iodine (PI) to detect the presence of contaminating aneuploid (TRAMP-C1) cells in the TIL fraction. Generally, <10% of this fraction contained TRAMP-C1 tumor cells (data not presented). It is apparent from Fig. 2A that 8 days of flt3-L immunotherapy modestly enhanced, relative to carrier treated mice, the number of B and T (CD4+ and CD8+) cells that infiltrated TRAMP-C1 tumors and that these differences became more pronounced after 16 days of treatment. After 20 days of flt3-L therapy, the number of lymphoid cells dramatically decreased, although lymphocytes could still be detected at low numbers at day 90. We failed to detect a significant natural killer (NK) cell infiltrate in carrier or flt3-L treated animals using a monoclonal antibody (clone DX5) that recognizes a pan NK cell marker (data not shown). Flt3-L also induced an impressive myeloid infiltrate consisting of macrophages (mΦ), granulocytes (Gr-1+) and DCs (CD11c+) that was apparent after 8 days of treatment (Fig. 2B). Continued flt3-L treatment resulted in a further influx of myeloid cells that peaked after 16 days and then rapidly declined to basal levels on day 20 of treatment. With the exception of mΦ on day 20, markedly reduced numbers of these same cell types were detected in tumors isolated from mice treated with carrier. The TME did not induce abnormal expression of cell-type specific markers. For example, when infiltrating mΦ were evaluated for co-expression of CD11c and Gr-1, less than 10% of these cells were positive for the markers associated with DC and granulocytes, respectively (data not presented).
Phenotypic characterization of lymphoid and myeloid cells infiltrating TRAMP-C1 tumors during flt3-L immunotherapy. Mice with palpable TRAMP-C1 tumors were treated for 21 consecutive days with either carrier or flt3-L (30 μg/injection). At the indicated times, tumors were excised, digested and TILs isolated and stained with the indicated mAb. The average number of cells isolated from four TRAMP-C1 tumors bearing the indicated lymphoid ( A) or myeloid ( B) markers was determined by flow cytometry. Note that the scales are different in A and B
Alterations in dendritic cell phenotypes induced by the prostate tumor microenvironment
The above findings suggest that the anti-tumor immune response was not sufficient to inhibit growth of residual flt3-L-refractory tumor cells. Because dendritic cells play a crucial role in the induction and maintenance of immunity, tumor-infiltrating DCs were phenotyped for the presence of MHC class II and the co-stimulatory molecule B7.2, proteins found critical for T cell antigen recognition and activation, respectively. We were also interested in CD8α+ DCs, because this subset may possess unique immunoregulatory functions [16]. The results of a representative experiment are presented in Fig. 3 and indicate that DCs normally infiltrate TRAMP-C1 tumors after 7 (data not shown) and 14 days (Fig. 3A) of treatment with carrier. However, it is also apparent that flt3-L treatment was associated with a more pronounced DC infiltrate (compare Fig. 3A and D, 23 versus 76%). This was also true when data was expressed as absolute numbers of DCs isolated per tumor (data not presented). After 1 week of therapy, most of the intra-tumor DCs were CD8α-I-Ab+ in both control and flt3-L-treated mice (Fig. 3B and E). An additional week of therapy was associated with the appearance of a minor population of CD8α+I-Ab+ DCs (Fig. 3C and F). Thus, CD11c+CD8α-I-Ab- DCs were the predominate intra-tumor DC subset during the early phases of tumor progression, especially in mice treated with flt3-L. Tumor progression in control mice treated with carrier was associated with continued loss of class II expression and the accumulation of CDllc+B7.2+I-Ab- intratumoral DCs (Fig. 3G and H). Because flt3-L induced a pronounced regression of TRAMP-C1 tumors after 21 days of therapy, we could not evaluate intratumoral DCs in a flt3-L setting at these latter time points. However, splenic DCs from TRAMP-C1-bearing mice treated with flt3-L were very deficient in class II antigen expression relative to DC class II antigen expression on splenic DCs from carrier treated mice and non-tumor-bearing animals (Fig. 3I–K).
Characterization of dendritic cell subsets infiltrating TRAMP-C1 tumors during flt3-L immunotherapy. TILs were isolated from TRAMP-C1-bearing mice after treatment with either carrier or flt3-L and then DCs phenotyped by 3-color flow cytometry. A and D illustrate a representative single color analysis (log fluorescence versus side scatter) using anti-CD11c to stain DCs present in TILs isolated from mice treated with carrier ( A) or flt3-L ( D) for 14 days. Using these gates, the co-expression of CD8α and I-Ab on tumor-infiltrating CD11c+ DCs was determined after 7 ( B), 14 ( C), 21 ( G) or 28 ( H) days of treatment with carrier. The phenotype of intratumoral DCs in mice treated for 7 and 14 days with flt3-L is presented in E and F, respectively. In I, the co-expression of B7.2 and I-Ab on normal splenic DCs (CD11c+) is presented for comparison with splenic DCs from mice treated with carrier ( J) or flt3-L ( K) for 3 weeks
Efficacy of flt3-L and CD40-L combination immunotherapy on prostate tumor growth
The limited expression of class II antigens on intra-tumor DC suggests that these cells may function poorly as antigen-presenting cells. Because CD40 ligand (CD40-L) can augment anti-tumor immune responses by promoting DC maturation [26], we tested the efficacy of flt3-L given in combination with CD40-L to promote long-term regression of pre-existing TRAMP-C1 tumors. The results, presented in Fig. 4, demonstrate that CD40-L alone did not inhibit the growth of TRAMP-C1 tumors relative to mice treated with carrier. Again, treatment with flt3-L for 21 days markedly inhibited TRAMP-C1 tumor growth with tumors undetectable in some animals at the end of therapy. The combination of CD40-L and flt3-L appeared to initially enhance flt3-L-induced tumor growth inhibition, but with time, tumor progression ensued following termination of therapy producing kinetics similar to the flt3-L treated group.
Efficacy of flt3-L given in combination with CD40-L to induce tumor regression and prevent disease relapse. Mice with palpable TRAMP-C1 tumors were treated with carrier, trimeric CD40-L (50 μg/dose), flt3-L (30 μg/dose) or a combination of flt3-L and CD40-L. Mice received 21 consecutive injections of carrier or flt3-L, whereas CD40-L was given just the last week of treatment. Values represent mean tumor volumes ± SD of 5–9 mice/group. Arrows indicate when immunotherapy was initiated and terminated. For humane reasons, tumor volume measurements were not obtained at latter time points for mice treated with either carrier or CD40-L. The experiment was repeated a second time and yielded similar results
Evaluation of agonistic 4-1BB antibody therapy on tumor growth
Because tumor-infiltrating DCs cells lose expression of MHC class II molecules, intratumoral CD4+ T cell anti-tumor immune responses will be diminished. Therefore, we sought to boost the flt3-L-dependent immune response by delivering an alternative co-stimulatory signal with agonistic anti-4-1BB mAb. The 4-1BB can function as a potent co-stimulatory signal for CD4 and CD8 anti-tumor T cells in vivo independent of B7/CD28-mediated co-stimulation [7, 37]. More importantly, co-stimulation with agonistic mAb to 4-1BB augments the immune response to weakly immunogenic tumors independent of CD4+ helper T (Th) cell function [8]. Mice with established tumors were therefore treated with carrier, flt3-L, anti-4-1BB mAb alone or a combination flt3-L and anti-4-1BB mAb. At various times during treatment, cohorts were also evaluated for splenic CTL and NK cell activity, two effector cell types reported to be augmented by flt3-L and 4-1BB mAb treatment. As expected, flt3-L dramatically inhibited the growth of TRAMP-C1 tumors, whereas, agonistic mAb to 4-1BB did not alter the growth kinetics of TRAMP-C1 tumors (Fig. 5A). Adjunctive therapy with agonistic 4-1BB mAb did not significantly alter the growth kinetics of TRAMP-C1 tumors relative to mice given flt3-L alone. Spleen cells from mice treated with carrier were not cytotoxic for either TRAMP-C1 target cells or the NK cell-sensitive cell line, YAC-1 (Fig. 5B). In contrast, YAC-1 target cells were killed in a dose-dependent fashion when incubated with spleen cells from mice treated with flt3-L, 4-1BB mAb or the flt3-L/4-1BB mAb combination (Fig. 5B, and data not shown). TRAMP-C1 targets were not lysed, indicating that these cells are relatively resistant to NK cell-mediated cytotoxicity. These findings indicate that flt3-L administered alone or in combination with agonistic mAb induced a marked growth inhibition of established TRAMP-C1 tumors. Despite an enhanced splenic NK cell response, adjunctive 4-1BB co-stimulation of T cells in a flt3-L setting did not result in long-term cures because all mice eventually experienced disease relapse following termination of therapy (data not shown).
Evaluation of flt3-L and 4-1BB combination immunotherapy for the treatment of prostate cancer. A Mice bearing palpable TRAMP-C1 tumors were treated for 21 consecutive days with carrier, flt3-L (30 μg/dose), agonistic anti-4-1BB Ab or a combination of flt3-L and 4–1BB Ab. Antibody to 4-1BB was given on days 3 and 6 of therapy at 200 μg/dose as indicated by upward pointing arrows. Tumor volumes were measured twice weekly and data are presented as mean tumor volume ± SD of 6–18 animals per group. Downward pointing arrows indicate when flt3-L therapy was initiated and terminated. B On days 7, 14 and 35 after initiation of therapy, spleen cells from TRAMP-C1-bearing mice treated with carrier, flt3-L or 4-1BB Ab were titrated into 96-well round-bottom plates containing a constant number of 51Cr labeled target cells. After a 4-h incubation, plates were centrifuged, supernatants removed and counted to determine % net release. In I, anti-4-1BB Ab treated mice were injected with a 0.05 ml rabbit anti-asialo GM1 serum (Waco Chemicals USA, Dallas, Texas) 1 day before performing the cytotoxicity assay. Spleen cells were then tested against YAC-1 target cells to confirm that cytolytic activity was mediated by NK cells ( open boxes)
Disruption of T cell signaling complex by the prostate tumor microenvironment
The failure of 4-1BB–mediated co-stimulation of T cells to induce a curative anti-tumor immune response may reflect the impact of an immunosuppressive prostate TME on T cell function. To determine whether the TCR/CD3 complex remains intact and potentially functional on tumor-infiltrating T cells, mice with palpable TRAMP-C1 tumors were treated with either carrier or flt3-L for 14 days and the co-expression of αβTCR and CD3ε on gated Thy-1+ cells determined by three-color flow cytometric analysis. Thy-1 was used as a pan T cell marker, because expression of this molecule was relatively stable within the TME (manuscript in preparation). As shown in Fig. 6, by day 7 of treatment, only 2–4% of Thy-1+ tumor-infiltrating T cells isolated from either carrier or flt3-L treated mice co-expressed CD3ε and TCRβ. This contrasts with normal splenic T cells, where 95% of Thy-1+ cells co-expressed CD3ε and TCRβ (compare Fig. 6A and M). Both CD4+ and CD8+ T cells lost expression of these molecules regardless of their treatment (Fig. 6B, C, E and F). Loss of double positive (TCRβ+CD3ε+) intratumoral T cells was due primarily to the disappearance of CD3ε. An additional week of tumor growth was also associated with loss of TCRβ expression on TILs isolated from carrier-treated mice (Fig. 6G–I). Although flt3-L treatment diminished the loss of TCRβ and to a lesser extent CD3ε on CD4+ T cells, it did not result in a population of T cells with normal signaling complexes because only 2% of CD4+ cells were TCRβ+CD3ε+ (Fig. 6K). Most tumor-infiltrating CD4+ T cells isolated from flt3-L treated mice were TCRβ+CD3ε- with minor populations of either CD3ε+TCRβ- or CD3ε-TCRβ-. In both groups of mice, TCRβ expression on CD8+ T cells was essentially lost by day 14 of treatment (Fig. 6I and L). Failure to express these signaling molecules was not due to proteolytic cleavage during tumor digestion, because normal spleen cells treated with the same enzymes expressed normal levels of TCRβ and CD3ε (data not shown). Disruption of the TCR/CD3 complex was restricted to TME because this complex remained intact on splenic T cells isolated from TRAMP-C1-bearing mice (data not presented).
Disruption of the TCR/CD3 signaling complex by the prostate tumor microenvironment. Mice with palpable TRAMP-C1 tumors were treated with either carrier ( A – C and G – I) or flt3-L ( D – F and J – L) and after 7( A – F) or 14 days ( G – L) tumors were excised, digested and TILs isolated for three-color flow cytometry. Low forward and side scatter cells were gated for Thy-1, CD4 or CD8 and then assessed for co-expression of the indicated molecules. In M, N and O, spleen cells from non-tumor-bearing mice were triple stained with the same antibodies used to phenotype TILs and are included to illustrate the level of expression of TCRβ and CD3ε on normal splenic T cells
Sensitivity of TRAMP-C1 tumor cells to cytotoxic T lymphocytes
Because tumors have devised mechanisms to avoid immune-mediated elimination, we tested the sensitivity of TRAMP-C1 cells to the lytic activity of CTLs, an effector population that is believed to play an important role in the clearance of malignant cells. In a standard 4-h isotope release assay, TRAMP-C1 target cells were not killed by alloreactive CTLs (Fig. 7A). This resistance was unrelated to the level of expression of class I antigens because pretreatment with IFN-γ induced up-regulation of class I antigens, but did not result in increased killing of TRAMP-C1 cells. (Fig. 7B and C). The inability of alloreactive CTLs to kill TRAMP-C1 tumor cells following up-regulation of class I antigens by IFN-γ suggests that these tumor cells may be inherently resistant to CTL-mediated lysis. We tested this possibility in a lectin-dependent assay and demonstrated that TRAMP C1 cells were not efficiently killed following conjugate formation (Fig. 7D). Lysis of B10.2 and syngeneic MKSA target cells in the presence of lectin confirmed the presence of cytotoxic activity in the alloreative CTL population. However, TRAMP-C1 cells were killed following an extensive incubation period (24 h), and the cytolytic activity was sensitive to anti-Thy-1 plus complement treatment (Fig. 7E and F). DNA fragmentation studies verified that isotope release over this extended incubation period was due to tumor cell destruction mediated by CTLs (Fig. 7G).
TRAMP-C1 tumor cells are relatively resistant to lytic activity of cytotoxic T lymphocytes. Alloreactive CTLs were generated in vitro by co-culture of BALB/c spleen cells with mitomycin C-treated splenic stimulators from B6 (H-2 b) mice. Cultures were harvested after 5 days and incubated for either 4 h with labeled (51Cr) TRAMP-C1 (TC1), B10-2 (H-2 b) and MKSA (H-2 d) target cells ( A). B TC1 cells were either incubated in media or 10 μg/ml of recombinant mouse IFN-γ for 48 h. Cells were then washed, radiolabeled and evaluated for their sensitivity to anti-H-2 b CTLs. C Aliquots of TRAMP-C1 cells incubated with media alone (-IFN-γ, left panels) or with IFN-γ (+IFN-γ, right panels) were stained with either a FITC-conjugated anti-H-2Kb ( upper panels) or an anti-H-Db Ab. The number of tumor cells expressing class I molecules was then determined by flow cytometry. D Alloreactive (BALB/c anti-B6) spleen cells were incubated in the presence of the indicated concentration of concanavalin A (Con A) in a 4-h isotope release assay. The increased killing of the syngeneic target MKSA in the presence of 10 μg/ml of Con A serves as a positive control. E, F Alloreactive CTLs were treated with media, rabbit complement (C')(Pel-Freez, Brown Deer, Wis.) alone or anti-Thy-1 Ab (PharMingen, San Diego, Calif.) plus complement (Ab + C') prior to testing in a 4- ( E) or 24-h ( F) isotope release assay. G Aliquots of cells used in F were examined for DNA fragmentation to verify that isotope release represented cell death
Discussion
We previously reported that flt3-L induces an impressive growth inhibition of well-established prostate tumors growing at an ectopic site. However, termination of therapy was invariably associated with disease relapse and re-initiation of flt3-L treatment at this time failed to prevent tumor progression [6]. In prior studies the mechanistic basis for the flt3-L-induced tumor regression was not evaluated. To address this issue, we assessed the ability of flt3-L to inhibit the growth of TRAMP-C1 tumors in severe combined immunodeficient (SCID) mice. Flt3-L inhibited TRAMP-C1 growth in these mice compared to SCID mice treated with carrier, suggesting that the innate response contributed to tumor growth inhibition. This view is also supported by flow cytometric studies demonstrating that flt3-L induced a marked myeloid infiltrate into TRAMP-C1 tumors. This response waned at day 21 of therapy, a time when few TRAMP-C1 cells could be detected at the inoculation site. However, TRAMP-C1 cells grew much more rapidly in SCID mice treated with either carrier or flt3-L relative to wild-type mice treated similarly. This suggests that both adaptive and innate responses contribute to flt3-L-mediated tumor growth inhibition. These data are similar to studies reported by Lynch and his collaborators in a fibrosarcoma model; they observed that flt3-L augmented both innate and tumor-specific immune responses [24]. However, this study differs from ours because they obtained long-term cures in a number of animals given flt3-L therapy. This disparity may be due to their early treatment of tumor-inoculated mice and, indeed, when treatment was delayed, fewer long-term cures were obtained.
With respect to anti-tumor immunity, infiltrating lymphoid cells (CD4+, CD8+, B220+, NK cells ) were detected only in trace numbers in tumors from control mice. Flt3-L treatment induced a lymphoid cell infiltrate composed primarily of CD4+ and CD8+ T cells as well as a robust DC infiltrate. There was little evidence by flow cytometry of a flt3-L-induced NK cell infiltrate, although NK cell activity was augmented in the spleen of animals treated with this cytokine. This observation is consistent with our inability to detect perforin+ cells in TRAMP-C1 tumors using P1-8, a monoclonal antibody specific for mouse perforin (data not shown). The failure of infiltrating T cells to eradicate TRAMP-C1 tumor cells suggests that the anti-tumor immune response was not sufficient to resist progressive growth of TRAMP-C1 cells that survived flt3-L treatment. The reason(s) for this is presently unclear, although we have identified several features of the TRAMP-C1 TME that may promote progressive tumor growth despite immunotherapeutic intervention. For example, we have documented the progressive loss of class II antigens on tumor-infiltrating DCs and the accumulation of CD11c+B7.2+I-A- DCs in TRAMP-C1 tumors. Deficient expression of class II antigens suggests that infiltrating DCs may be immature, particularly in a flt3-L setting, and incapable of inducing a sufficient anti-tumor immune response. That tumor-associated DCs may function poorly as antigen presenting cells (APCs) for sustaining intra-tumor immune responses is consistent with studies in a rat colon cancer model where tumor-derived DCs were shown to be poor stimulators of allogeneic T cell proliferation and cytokine production [3]. The functional defect was related to the limited expression of essential co-stimulatory molecules such as B7 on tumor-derived DCs. Vicari and colleagues [39] also recently reported that solid tumors induce a state of DC paralysis that renders them refractory to stimulation with lipopolysaccharide, interferon-α and anti-CD40 mAb. In humans, alterations and/or elimination of DCs is a significant negative predictor of overall survival, disease-free survival and time to disease recurrence in patients with oral carcinoma [15]. To promote DC differentiation in the TRAMP-C1 model and augment the anti-tumor immune response, mice were treated with the combination flt3-L and CD40-L. Prior studies demonstrated that CD40 is a requisite DC maturation signal and that flt3-L and CD40-L synergize in the generation of immune responses against poorly immunogenic tumors ([1, 26] and reviewed in [25]). The flt3-L/CD40-L combination produces more DCs than either of the cytokines alone, suggesting that CD40-L promotes DC proliferation and/or survival of DC generated by flt3-L treatment [1]. Indeed, antigen-specific T cell expansion cannot be sustained in the absence of CD154-CD40 interactions and this demise is due to the rapid disappearance of DC in vivo [30]. Because of these reported properties of CD40 signaling, TRAMP-C1-bearing mice were treated with the combination of flt3-L and CD40-L. However, mice treated with CD40-L alone or in combination with flt3-L were not protected from progressive tumor growth following termination of therapy. The inability of this combination to produce long-term cures was not due to loss of CD40, because ~40% of tumor infiltrating CD11c+ cells co-expressed CD40 (data not presented). Another feature of the TRAMP-C1 model is the intratumoral accumulation, in both carrier and flt3-L treated mice, of CD8α+ DCs, a subset with reported immunoregulatory properties [16]. However, recent studies by Iyoda et al. [18] demonstrated that CD8+ DCs, but not CD8- DCs, phagocytose and cross-present antigens derived from malignant cells in situ. Because CD8+ DCs were not detected in TRAMP-C1 tumors until 2 weeks of flt3-L treatment, WT1 peptides may not have been presented for activation of tumor infiltrating WT1 T cells. Thus, these data suggest that the inability of tumor-associated DCs to maintain expression of class II antigens makes it likely that an anti-WT1 CD4+ T cell response will not be sustained in the prostate TME. This response may be further dampened by the inability of tumor-associated CD8α- DCs to cross-present WT1 peptides for CTL generation.
Because tumor-associated DCs lose expression of class II antigens, we sought to more directly enhance CTL responses to TRAMP-C1 tumors by using agonistic anti-4-1BB mAb, which has been shown to induce CTL priming to peptide antigens independent of CD4+ T cell help [8, 31]. In addition, impressive CD4-independent regression and long-term cures of mice bearing established B10.2 tumors has been achieved with this mAb therapy [31]. Although a similar protocol was followed, agonistic anti-4-1BB mAb alone did not induce regression in any TRAMP-C1-bearing animals and did not enhance flt3-L-induced tumor growth inhibition. These different outcomes may be related to the progressive loss of MHC class I antigens on TRAMP-C1 cells during growth in vivo. Consistent with this view, 4-1BB mAb induced regression in four of six tumor models; refractory tumors were MHC class I negative similar to TRAMP-C1 [31].
Another characteristic of TRAMP-C1 tumors that may allow these cells to escape immune elimination is the ability to disrupt the TCR/CD3 signaling complex on infiltrating, but not systemic T cells. Although prior studies have reported loss of CD3ζ chains on T cells from tumor-bearing animals and patients with advanced disease, these studies used CD3ε as a T cell marker to examine co-expression of CD3ζ [17, 19, 20, 27, 34]. Because loss of CD3-epsilon expression may be a general feature in the tumor-bearing host, evaluating CD3ζ expression on CD3ε+ cells excludes a considerable percentage of T cells from this type of analysis. By gating on a marker like Thy-1 (or CD4/CD8), which better maintains expression in the TME (manuscript in preparation), CD3ε- cells were included in our studies and demonstrated disruption of the TCR (TCRβ loss) on tumor-infiltrating lymphocytes. Loss of CD3ε occurred first, and this was followed by loss of TCRβ chain, a sequence that would have prevented detecting TCRβ loss in prior studies that gated on CD3ε+ cells. TME-induced alterations in the TCR signaling complex could not be reversed by flt3-L treatment because <2% of the tumor-infiltrating T cells co-expressed these proteins. It could be argued that intra-tumor Thy-1+ cells are not T cells. However, Thy-1+ cells cultured overnight in IL-2 re-expressed both CD3ε and TCRβ (manuscript in preparation). These data could not be explained by the preferential survival of CD3ε+TCRβ+ cells during the culture period. Thus, Thy-1+CD3ε-TCRβ- cells represent bona fide T cells whose TCR/CD3 signaling complex is markedly altered by the TME. Recent examination of the CD3-zeta chain revealed loss of this signaling molecule prior to loss of CD3ε and TCRβ (manuscript in preparation). Whiteside and colleagues have demonstrated that CD3ζ is a substrate for intracellular caspases and based on this and other observations argued that loss of CD3ζ indicates that these cells are undergoing apoptosis in their model [13]. The ability of Thy-1+ cells to re-express these signaling molecules after in vitro culture is not consistent with this hypothesis, but supports the view that loss of TCR/CD3 signaling molecules precedes apoptotic death [19].
In summary, TRAMP-C1 tumors established at an ectopic site underwent a dramatic flt3-L-induced growth inhibition that correlated temporally with a robust mixed cell infiltrate containing both myeloid and lymphoid elements. Studies in SCID mice suggested that flt3-L-induced tumor growth inhibition was mediated by both innate and adaptive anti-tumor immunity. Phenotypic analysis of infiltrating host cells revealed a progressive loss of MHC class II antigens on DCs and disruption of the TCR/CD3 complex even in a flt3-L setting. Combination immunotherapy designed to promote DC maturation (trimeric CD40-L) or T cell activation by an alternative co-stimulatory pathway (4-1BB) was no more effective than flt3-L alone. It should be noted that even if a potent WT1-specific CTL response was induced by these immune interventions, the inability of CTLs to kill TRAMP-C1 cells quickly may limit their ability to prevent tumor progression. The failure of CD40-L and agonistic 4-1BB Ab, two immune-based strategies with impressive efficacy in prevention models, to prevent growth of established tumors demonstrates the importance of utilizing treatment models to evaluate novel immunotherapies. Thus, new strategies will have to be designed that effectively overcome the immunosuppressive properties of prostate tumors microenvironment before long-term cures will be achieved by immunotherapeutic interventions.
References
Borges L, Miller RE, Jones J, Ariail K, Whitmore J, Fanslow W, Lynch DH (1999) Synergistic action of fms-like tyrosine kinase 3 ligand and CD40 ligand in the induction of dendritic cells and generation of antitumor immunity in vivo. J Immunol. 163: 1289
Brasel K, McKenna HJ, Morrissey PJ, Charrier K, Morris AE, Lee CC, Willliams DE, Lyman SD (1996) Hematologic effects of flt3 ligand in vivo in mice. Blood 88: 2004
Chaux P., Favre N., Martin M, Martin F (1997) Tumor-infiltrating dendritic cells are defective in their antigen-presenting function and inducible B7 expression in rats. Int J Cancer 72: 619
Ciavarra RP (1990 T helper cells in cytotoxic T lymphocyte development: Role of L3T4+-dependent anti-independent T helper cell pathways in virus-specific and alloreactive cytotoxic T lymphocyte response. Cell Immunol 125: 363
Ciavarra, RP, Silvester S, Brody T (1987) Analysis of T cell subset proliferation at afebrile and febrile temperatures: differential response of LYT-1+23- lymphocytes to hyperthermia following mitogen and antigen stimulation and its functional consequences on development of cytotoxic lymphocytes. Cell Immunol 107: 292
Ciavarra RP, Somers KD, Brown RR, Glass WF, de Angelis Consolvo PJ, Wright GL, Schellhammer PF (2000) Flt3-ligand induces transient tumor regression in an ectopic treatment model of major histocompatibility complex-negative prostate cancer. Cancer Res 60: 2081
DeBenedette MA, Shahinian A, Mak TW, Watts TH (1997) Costimulation of CD28- T lymphocytes by 4–1BB ligand. J Immunol 158: 551
Diehl L, van Mierlo GJ, den Boer AT, van der Voort E, Fransen M, van Bostelen L, Krimpenfort P, Melief CJ, Mittler R, Toes RE, Offringa R (2002) In vivo triggering through 4–1BB enables Th-independent priming of CTL in the presence of an intact CD28 co-stimulatory pathway. J Immunol 168: 3755
Forni G., Lollini P. L., Musiani P., Colombo MP (2000) Immunoprevention of cancer: is the time ripe? Cancer Res 60: 2571
Foster BA, Gingrich JR, Kwon E., Madias C, Greenberg NM (1997) Characterization of prostatic epithelial cell lines derived from transgenic adenocarcinoma of the mouse prostate (TRAMP) model. Cancer Res 57: 3325
Gaiger A, ReeseV, Disis ML, Cheever MA. (2000) Immunity to WT1 in the animal model and in patients with acute myeloid leukemia. Blood 96: 1480
Gao L, Bellantuono I, Eisasser A, Marley SB, Gordon MY, Goldman JM, Stauss HJ (2000) Selective elimination of leukemic CD34+ progenitor cells by cytotoxic T lymphocytes specific for WT1. Blood 95: 2198
Gastman BR., Johnson DE, Whiteside TL, Rabinowich H (1999) Caspase-mediated degradation of T-cell receptor zeta-chain. Cancer Res 59: 1422
Greenberg, NM, DeMayo F, Finegoldm MJ., Medina D., Tilley WD., Aspinall JO, Cunha GR, Donjacour AA, Matusik RJ, Rosen JM (1995) Prostate cancer in a transgenic mouse. Proc Natl Acad Sci USA 92: 3439
Grandis JR, Falkner DM, Melhem MF, Gooding WE, Drenning SD, Morel PA (2000) Human leukocyte antigen class I allelic and haplotype loss in squamous cell carcinoma of the head and neck: clinical and immunogenetic consequences. Clin Cancer Res 7: 2794
Grohmann U, Bianchi R, Belladonna ML, Vacca C, Silla S, Ayroldi E, Fioretti MC, Puccetti P (1999) IL-12 acts selectively on CD8α- dendritic cells to enhance presentation of a tumor peptide in vivo. J Immunol 163: 3100
Healy CG, Simons JW, Carducci MA, DeWeese T, Bartkowski M, Tong KP, Bolton WE (1998) Impaired expression and function of signal transducing zeta chains in peripheral T cells and natural killer cells in patients with prostate cancer. Cytometry 32: 109
Iiyoda T, Shimoyama S, Liu K, Omatsu Y, Akiyama Y, Maeda Y, Takahara K, Steinman RM, Inaba K (2002) The CD8+ dendritic cell subset selectively endocytoses dying cells in culture and in vivo. J Exp Med 195: 1289
Kiessling R, Wasserman K, Horiguchi S, Kono K, Sjoberg J, Pisa P, Petersson M (1999) Tumor-induced immune dysfunction. Cancer Immunol Immunother 48: 353
Kono K, Ressing ME, Brandt RM, Melief CJ, Potkul RK, Amdersson B, Petersson M, Kast WM, Kiessling R (1996) Decreased expression of signal-transducing zeta chain in peripheral T cells and natural killer cells in patients with cervical cancer. Clin Cancer Res 2: 1825
Kopersztych S, Rexkallah MT, Miki SS, Naspitz CK, Mendes NF (1976) Cell mediated immunity in patients with carcinoma: correlation between clinical stage and immunocompetence. Cancer 38: 1149
Lai P, Rabinowich H,. Crowley-Nowick PA, Bell MC, Mantovani G, Whiteside TL (1996) Alterations in expression and function of signal-transducing proteins in tumor-associated T and natural killer cells in patients with ovarian carcinoma. Clin Cancer Res 2: 167
Le YS, Kim TE, Kim BK, Park YG, Kim GM, Jee SB, Ryu KS, Kim IK, Kim JW (2002) Alterations of HLA class I and class II antigen expressions in borderline, invasive and metastatic ovarian cancers. Exp Mol Med 34: 18
Lynch DH, Andreasen A, Maraskovsky E, Whitmore J, Miller RE, Schuh JC (1997) Flt3 ligand induces tumor regression and antitumor immune responses in vivo. Nat Med 6: 625
Mackey M, Barth RJ, Noelle RJ (1998) The role of CD40/CD154 interactions in the priming, differentiation and effector function of helper and cytotoxic T cells. J Leukocyte Biol 63: 418
Mackey MF, Gunn JR, Maliszewsky C, Kikutani H, Noelle RJ, Barth RJ Jr (1998) Dendritic cells require maturation via CD40 to generate protective antitumor immunity. J Immunol 161: 2094
Matsuda M., Petersson M, Lenkei R, Taupin JL, Magnusson I, Mellstedt H, Anderson P, Kiessling R (1995) Alterations in the signal-transducing molecules of T cell and NK cells in colorectal tumor-infiltrating, gut mucosal and peripheral lymphocytes: correlation with the stage of the disease. Int J Cancer 61: 765.
Matzinger P (1991) The JAM test. A simple assay for DNA fragmentation and cell death. J Immunol Methods 145: 185
Melero I, Shuford WW, Newby SA, Aruffo A, Ledbetter JA, Hellstrom KE, Mittler RS, Chen L (1997). Monoclonal antibodies against the 4-1BB T-cell activation molecule eradicate established tumors. Nat Med 6: 682
Miga AJ, Masters SR, Durell BG, Conzalez M, Jenkins MK, Maliszewski C, Kikutani J, Wade WF, Noelle RJ (2001) Dendritic cell longevity and T cell persistence is controlled by CD154-CD40 interactions. Eur J Immunol 31: 959
Miller RE, Jones J, Le T, Whitmore J, Boiani N, Gliniak B, Lynch DH (2002). 4-1BB-specific monoclonal antibody promotes the generation of tumor-specific immune responses by direct activation of CD8 T cells in a CD40-dependent manner. J Immunol. 169: 1792
Mizoguchi H, O'Shea JJ, Longo DL, Loeffler CM, McVicar DW, Ochoa AA (1992) Alterations in signal transduction molecules in T lymphocytes from tumor-bearing mice. Science 258: 1795
Murphy G, Tjoa B, Ragde J, Kenny G, Boynton A (1996) Phase I clinical trial: T cell therapy for prostate cancer using autologous dendritic cells pulsed with HLA-A0201-specific peptides from prostate-specific membrane antigen. Prostate 29: 371
Reichert TE, Day R, Wagner EM, Whiteside TL (1998) Absent or low expression of zeta chain in T cells at the tumor site correlates with poor survival in patients with oral carcinoma. Cancer Res 58: 5344
Reichert TE, Scheuer C, Day R, Wagner W, Whiteside TL (2001) The number of intratumoral dendritic cells and zeta chain expression in T cells as prognostic and survival biomarkers in patients with oral carcinoma. Cancer 91: 2136
Ryu KS, Lee YS, Kim BK, Park YG, Kim YW, Hur SY, Kim TE, Kim IK, Kim JW (2001) Alterations of HLA class I and II antigen expression in pre-invasive, invasive and metastatic cervical cancers. Exp Mol Med 33: 136
Tan JT, Whitmire JK, Ahmed R, Pearson TC, Larsen CP (1999). 4-1BB ligand, a member of the TNF family, is important for the generation of antiviral CD8 T cell responses. J Immunol 163: 4859
Velders MP, Schrieber H, Kast WM (1998) Active immunization against cancer: impediments and advances. Semin Oncol 25: 697
Vicari AP, Chiodom D, Vaure C, Ait-Yahia S, Dercamp C, Matsos F, Reynard O, Taverne C, Merle P, Colombo MP, O'Garra A, Trinchiere G, Caux C (2002). Reversal of tumor-induced dendritic cell paralysis by CpG immunostimulatory oligonucleotide and anit-interleukin-10 receptor antibody. J.Exp Med 196: 541
Wilcox RA, Flies DB, Zhu G, Hohnson AJ, Tamada K, Chapoval AI, Strome SE, Pease LR, Chen L (2002) Provision of antigen and CD137 signaling breaks immunological ignorance, promoting regression of poorly immunogenic tumors. J Clin Invest 109: 651
Acknowledgements
This study was supported by grants from the Elsa U. Pardee Foundation and the Jeffress Memorial Trust.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ciavarra, R.P., Brown, R.R., Holterman, D.A. et al. Impact of the tumor microenvironment on host infiltrating cells and the efficacy of flt3-ligand combination immunotherapy evaluated in a treatment model of mouse prostate cancer. Cancer Immunol Immunother 52, 535–545 (2003). https://doi.org/10.1007/s00262-003-0383-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-003-0383-x