Abstract
Purpose
To compare the success rate, clinical outcomes, and complications of retroperitoneal (RP) versus transperitoneal (TP) percutaneous catheter drainage (PCD) of the necrotic pancreatic fluid collections.
Materials and methods
This retrospective study comprised consecutive patients with acute pancreatitis who underwent PCD of lesser sac collections amenable to drainage via both TP and RP routes. The patients were divided into two groups based on the route of drainage (group I, RP, and group II, TP). The technical success, clinical success, complications, and clinical outcomes were compared between the groups. Subgroup analysis was performed based on the timing of drainage (acute necrotic collections, ANC vs. walled-off necrosis, WON) and organ failure (OF).
Results
Seventy-nine patients [mean age, 38.7 ± 12.3 years, 54 males] were included in the study. Group I and II comprised 22 (27.8%) and 57 (72.2%) patients, respectively. The procedures were technically successful in all the patients. There was no significant difference in the complication rate between the two groups. The clinical success was higher in group II (75.4%) as compared to group I (54.5%). However, the difference was not statistically significant (p = 0.070). There was no significant difference in the hospital stay (p = 0.298), intensive care unit stay (p = 0.401), need for surgical necrosectomy (p = 0.243), and mortality (p = 0.112) between the two groups. The outcomes in patients with OF and ANC were not affected by the route of PCD. Clinical success rate was significantly higher in WON undergoing TP drainage (p = 0.009).
Conclusion
Both RP and TP routes of PCD are safe and effective. Clinical success rate was significantly higher in WON undergoing TP drainage.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute pancreatitis (AP) is one of the most critical gastrointestinal conditions presenting to the emergency department. Based on the revised Atlanta classification (RAC), AP is classified into mild, moderately severe, and severe [1]. Most patients with mild AP have an uneventful course. However, those with moderately severe and severe AP have significant morbidity and mortality. The mortality rate in patients with severe acute pancreatitis ranges from 16.3 to 45.63% [2,3,4,5]. These patients may suffer local and systemic complications. The systemic complications predominate in the early phase of AP, which manifests clinically as systemic inflammatory response syndrome (SIRS) and multiple organ failure [1]. Among the local complications that predominate in the late phase of AP, necrotic collections are significant [6]. The management of necrotic peripancreatic collections has evolved significantly. A 'step-up approach' has evolved as the standard treatment for pancreatic collections [7]. This approach involves conservative management followed by drainage, either percutaneously or endoscopically. In case of non-resolution following drainage, necrosectomy either by minimally invasive surgical or by endoscopic methods is performed. Drainage of necrotic collections involves a multidisciplinary approach. Pancreatic fluid collections are increasingly being drained by the endoscopic route, which requires the collection to be closely abutting the stomach. Approximately, 42–48% of pancreatic fluid collections do not bulge into the gastric wall, limiting the efficacy and safety of endoscopic drainage [8]. Endoscopic ultrasound (EUS) is beneficial for collections that do not have a visible bulge. However, the endoscopic route is recommended only for mature collections (> 4 weeks) [9]. Many patients require drainage at an earlier stage (< 4 weeks) due to secondary infection. Also, the endoscopic route may not be suited in all patients due to generalized ill health. In such patients, percutaneous drainage has an indispensable role to play.
Image-guided percutaneous catheter drainage (PCD) is one of the most utilized methods for drainage [10, 11]. Almost half of the patients may respond to PCD alone [12]. In rest of the patients, PCD serves as an adjunct to endoscopic drainage (as a part of dual-modality drainage) or as a gateway to necrosectomy (either endoscopic or minimally invasive surgical) [13].
The two most common routes for PCD are retroperitoneal (RP) and transperitoneal (TP) routes. Less common transperitoneal approaches include transgastric and transhepatic [14]. RP is generally the preferred route suited for subsequent minimally invasive necrosectomy [9, 15, 16]. Also, this route can prevent the dissemination of infected material into the peritoneal cavity. Drainage of lesser sac collections via the RP route frequently requires lateral decubitus patient positioning and CT guidance, which may not be feasible in patients with severe AP on organ support. Collections in the lesser sac without significant extension to the pararenal space or paracolic gutters may not be safely accessible via RP approach and need direct TP drainage [17, 18].
The association between the route of drainage of pancreatic collection and the outcomes has not been systematically evaluated. Therefore, this study was conducted to evaluate the impact of the route of PCD on the technical success, clinical outcomes, and complications in patients with moderate to severe necrotizing AP.
Materials and methods
Study design and population
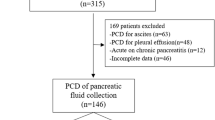
The local ethics committee approved this retrospective study, and the need for informed written consent was waived. A retrospective analysis of the database of consecutive patients of AP admitted in the Gastroenterology units of a tertiary care hospital between July 2018 and July 2020 was performed. Patients’ records were reviewed by a gastroenterologist, who was blinded to the route of PCD. Only those patients of AP were included in the study, who underwent PCD of necrotic fluid collections in lesser sac (with or without extension into left anterior pararenal or paracolic space) that were amenable to drainage via both RP or TP routes (based on imaging) but had PCD through one route (either RP or TP). Patients who underwent multiple PCD via both routes were excluded. Patients who underwent PCD of necrotic collection at other sites, including mesenteric, perihepatic, perisplenic, omentum, and right paracolic space, were also excluded. AP patients who underwent PCD for collections in chronic pancreatitis, and in whom complete clinical and radiological data were lacking, were also excluded.
Indications of PCD
Drainage was performed in patients with infected necrosis, pressure symptoms (causing gastric outlet obstruction or biliary obstruction), non-resolving organ failure, persistent SIRS, and intra-abdominal hypertension [19,20,21]. Infected necrosis was suspected based on clinical condition or the presence of gas within the collection on CT scan, and later confirmed by positive culture of the fluid aspirated at the time of drainage. As a part of our institutional protocol, aspiration of collection for diagnosis of infection was not done before PCD placement. All the patients with pancreatic fluid collections were managed using the step-up approach.
Patients who had walled-off necrotic collections in the vicinity of the gastroduodenal region underwent endoscopic drainage. All other patients underwent PCD.
PCD protocol
Interventional radiologists with 2–7 years of experience in abdominal interventions performed the procedures. Using image (CT/ultrasound) guidance catheter was inserted with the Seldinger technique. An 18-G needle was used to access the collection. Serial dilatations of the tract were done over 0.035″ inch stiff guidewire. Finally, a catheter (pigtail or malecot) was placed into the collection, followed by fixation of the catheter. The initial size of the catheter was 12–14 F regardless of the approach. Daily flushing of the catheter was done using 100 cc of normal saline. Catheter upsizing was done with a larger catheter (2–4 F larger than the previous catheter, maximum up to 24 F) based on the clinical status of the patient. The catheter was removed when there was no residual collection on imaging, drain output less than 10–20 cc/day for three consecutive days, and no features of sepsis.
Based on the route of PCD, the patient cohort was divided into two groups: RP (group I) and TP (group II).
PCD outcomes
The technical success of the PCD was defined as the completion of the drainage procedure as planned. Clinical success was defined as the resolution of collection (and discharge from the hospital) without the need for surgical necrosectomy. Other assessed parameters included resolution of organ failure, reduction in the volume of the collection by more than 50% of the pre-procedure size, total leucocyte count (TLC), and procalcitonin at one week after the procedure. Organ failure (OF) was defined using the modified Marshall scoring system [22]. The volume of collection was calculated pre and post PCD placement using a semi-automated method, using the three largest dimensions of the collection.
Procedure-related complications were recorded. Specifically, spillage of the contents of collection within the peritoneal cavity and hemorrhagic complications were assessed using a CT scan performed within 3–10 days after the procedure. The former was diagnosed when there were new air foci in the vicinity of collection away from the PCD, free air within the peritoneal cavity that was not seen on the last CT before drainage or increase in the ascites with new-onset or worsening abdominal pain and clinical signs of peritonitis. The catheter-related hemorrhagic complications were diagnosed in patients with gastrointestinal bleeding or bleeding into the PCD, or when a CT scan showed pseudoaneurysm or active contrast extravasation in the artery adjacent to the catheter tip. Additionally, catheter slippage was recorded.
Assessment of baseline characteristics and outcomes
The groups were compared for age, gender, etiology of AP, modified CT severity index (MCTSI), revised Atlanta classification (RAC) severity, nature of collection (acute necrotic collection, ANC vs. walled-off necrosis, WON), the volume of collection, TLC, procalcitonin, infected necrosis, organ failure (OF), the interval between onset of pain and PCD placement, and initial catheter size. OF was evaluated before the insertion of the first PCD. Various outcome parameters were assessed, including length of hospitalization (LOH), need for intensive care unit (ICU) admission, length of stay in the ICU, need for surgical necrosectomy, and mortality.
Statistical analysis
The continuous data were presented as mean with standard deviation, and the categorical data were presented as percentages. Kolmogorov–Smirnov test was used to assess the normality of data. Continuous variables were compared using the ANOVA or Kruskal–Wallis H test. Categorical variables were compared using the chi-square test. A p-value of < 0.05 was considered statistically significant for all the tests of association. SPSS software version 22 was used for the analysis. The outcomes were also compared in patients with OF and those with ANC and WON.
Results
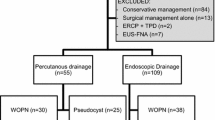
During the study period, 79 patients were included. Based on the approach to PCD, RP and TP drainage was performed in 22 (27.9%) and 57 (72.1%) patients, respectively. Figure 1 shows patient recruitment in detail.
Patient characteristics
The mean age was 38.7 years (± 12.3 years). There were 54 (68.4%) males and 25 (31.6%) females. Commonest etiological factor was alcohol consumption (n = 42, 51.3%), which was followed by cholelithiasis (n = 26, 33%) and endoscopic retrograde cholangiopancreatography (n = 2, 2.5%). According to RAC, 44 (55.6%) patients had severe disease, while 35 (44.4%) had moderately severe disease. The mean volume of collection was 458 cc (± 676.8 cc). The mean pain to PCD interval was 44.8 ± 64.8 days. Mean LOH was 33.1 days (± 19.9 days). Forty (50.6%) patients needed ICU admission. Surgical necrosectomy was required in 15(18.9%) patients. In-hospital mortality in the entire cohort was 16.4% (n = 13) (Table 1).
Comparison of baseline characteristics among the groups
The two groups were statistically similar in age, RAC severity, nature of collection (ANC vs. WON), the volume of the collection, MCTSI, and initial catheter size. Group I had a significantly higher number of male patients (77.3% vs. 61.4%, p = 0.010) and a higher percentage of alcohol-induced pancreatitis (82% vs. 42.1%, p = 0.008). The two groups were similar in baseline procalcitonin, TLC, pre-PCD OF, and infected necrosis (Table 2).
Technical success, clinical success, and complications
All the procedures were technically successful. There was no significant difference in the complications between the groups. There were no hemorrhagic complications in either of the groups. Spillage of the collection contents into the peritoneal cavity occurred in one patient in group I and two patients in group II. In the RP group, the spillage occurred as intraperitoneal air foci without clinical signs (Fig. 2). This patient was managed conservatively. One patient with intraperitoneal spillage in the TP group manifested as air foci within the adjacent mesentery and increased ascites with clinical signs of peritonitis. This patient was managed with PCD placement within the ascites. In the second patient, air foci were seen adjacent to the collection with no clinical signs. This patient was managed conservatively.
Although there was no significant difference in the clinical success (p = 0.070) between the two groups, there was a trend toward higher clinical success in group II (75.4% in group II vs. 54.5% in group I). In addition, LOH, need of ICU admission, LOICU, need of surgical necrosectomy, and mortality was also comparable between the groups (Table 3).
Subgroup analysis
Patients with OF (n = 45)
None of the outcome parameters were significantly different between the two groups (Table 4).
Patients with ANC (n = 46)
In the ANC subgroup, RP and TP drainage was performed in 10 and 36 patients, respectively. None of the outcome parameters were significantly different between the two groups (Table 5).
Patients with WON (n = 33)
RP and TP drainage was performed in 12 and 21 patients, respectively, in patients with WON. A significantly greater number of patients with TP drainage had clinical success (90.4 vs. 50%, p = 0.009). The rest of the outcomes were comparable between the two groups (Table 5).
Discussion
In this study assessing the impact of the route of PCD on the clinical outcomes in patients with AP and necrotic pancreatic fluid collections, the patients were divided into two groups (group I, RP, and group II, TP). These groups were similar in all the baseline characteristics, except for gender and etiology. The procedures were technically successful in all the patients. There was no significant difference in the complication rate between the two groups. The clinical success in group II was higher as compared to group I (75.4% in group II vs. 54.5% in group I); however, the difference was not statistically significant (p = 0.07).
On subgroup analysis, the outcomes in patients with OF and those with ANC were not affected by the route of PCD. However, significantly greater number of patients with WON undergoing TP drainage had clinical success. These results suggest that both RP and TP routes of drainage are safe and effective and either can be utilized for necrotic pancreatic collections.
The RP route is preferred for drainage of pancreatic collections as it can serve as a gateway for minimally invasive necrosectomy in patients who fail to respond to PCD alone [23]. Although this route can also provide access to the lesser sac collections, patient positioning in the lateral decubitus position and CT guidance are critical to the success of this approach. In patients with severe disease who are on organ system support, this becomes a technical challenge. Additionally, a safe window for drainage of some lesser sac collections may not be available via the RP route. TP route offers access to these collections. There is a lack of data comparing the two routes of catheter drainage.
In a study by Wronksi et al., 18 patients underwent PCD of pancreatic collections. RP approach through left lumbar access was preferred in all patients [24]. Drainage via the RP route was done in ten patients. Four patients underwent TP PCD, while other four underwent combined RP and TP catheter drainage because the collection was either inaccessible or undrainable through the left lumbar access. The overall success rate of PCD alone was 33%. There was no significant difference in the success rate between RP and TP routes. Bleeding occurred in two patients (one in the RP group and the other in the TP group). There was leakage of the necrotic contents into the peritoneal cavity in one patient in the TP group. Two patients in the RP group had an inadvertent injury to the peritoneum and leakage of contents into the peritoneal cavity.
Three series have explicitly reported the TP route for drainage of collections in AP. Baudin et al. reported TP PCD in 48 patients with clinical success of PCD alone in 64.6% of patients [25]. Bleeding occurred in two patients with spontaneous resolution in both the patients. In another series of 30 patients, TP PCD was performed at a mean of 18 days after pain onset in early infected pancreatic fluid collections. Clinical success was achieved in 63.3% of the patients with PCD alone [26]. Catheter-related complications were not explicitly reported. In the series by Freeny et al., TP drainage was done in 33 patients at a mean interval of 9 days in pancreatic parenchymal necrosis [27]. Clinical success with PCD alone was reported in 47% of the patients. There were no catheter-related complications. In a study of RP PCD in 40 patients planned for video-assisted RP debridement (VARD) of necrotic pancreatic collections, PCD alone was successful in 9 (23%) patients [28]. Among these patients, 7.5% had intrapancreatic only, 67.5% had an intrapancreatic and adjacent collection, and 25% had collection adjacent only to the pancreas. Twenty-five patients underwent VARD. Six patients underwent open necrosectomy. Three bleeding episodes were reported. Of these, one bleeding event occurred in PCD-alone group. However, this event was unrelated to the catheter. No studies are comparing the TP and RP routes of drainage.
There were a few limitations to our study. First, the sample size was small due to inclusion of patients who underwent PCD through either RP or TP route. Several patients who underwent both RP and TP procedures were excluded. Second, the retrospective nature of the study and lack of randomization led to different patient numbers in the two groups and may have affected the statistical significance of some of the results. Third, only those complications of PCD drainage were reported, which were documented on CT scans. Complications like secondary infection and external pancreatic fistula were not reported in the study. Finally, there was no long-term follow-up of these patients.
In conclusion, both RP and TP routes of PCD are safe and effective for drainage of necrotic pancreatic collections.
References
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG et al (2013) Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut 62(1):102-111.
Popa CC, Badiu DC, Rusu OC, Grigorean VT, Neagu SI, Strugaru CR (2016) Mortality prognostic factors in acute pancreatitis. J Med Life 9(4):413-418.
Fu C-Y, Yeh C-N, Hsu J-T, Jan Y-Y, Hwang T-L (2007) Timing of mortality in severe acute pancreatitis: experience from 643 patients. World J Gastroenterol 13(13):1966-1969.
Banks PA (1991) Infected necrosis: morbidity and therapeutic consequences. Hepatogastroenterology 38:116–119.
Büchler MW, Gloor B, Müller CA, Friess H, Seiler CA, Uhl W (2000) Acute necrotizing pancreatitis: treatment strategy according to the status of infection. Ann Surg 232:619–626.
Boxhoorn L, Voermans RP, Bouwense SA, Bruno MJ, Verdonk RC, Boermeester MA, et al (2020) Acute pancreatitis. Lancet 396(10252):726-734.
van Baal MC, van Santvoort HC, Bollen TL, Bakker OJ, Besselink MG, Gooszen HG (2011) Systematic review of percutaneous catheter drainage as primary treatment for necrotizing pancreatitis. Br J Surg 98(1):18-27.
Antillon MR, Shah RJ, Stiegmann G, Chen YK (2006) Single-step EUS-guided transmural drainage of simple and complicated pancreatic pseudocysts. Gastrointest Endosc 63(6):797-803.
Elmunzer BJ (2018) Endoscopic drainage of pancreatic fluid collections. Clin Gastroenterol Hepatol 16(12):1851-1863.
Mallick B, Dhaka N, Gupta P, Gulati A, Malik S, Sinha SK, et al (2018) An audit of percutaneous drainage for acute necrotic collections and walled off necrosis in patients with acute pancreatitis. Pancreatology 18(7):727-733.
Gupta P, Gupta J, Kumar C, Samanta J, Mandavdhare H, Sharma V, et al (2020) Aggressive Percutaneous Catheter Drainage Protocol for Necrotic Pancreatic Collections. Dig Dis Sci 65(12):3696-3701.
van Santvoort HC, Besselink MG, Bakker OJ, Hofker HS, Boermeester MA, Dejong CH, et al (2010) A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med 362(16):1491-1502.
Gupta P, Rana P (2021) Interventions in Pancreatitis: Drainage Procedures. In: Mukund A. (eds) Basics of Hepatobiliary Interventions. Springer, Singapore. pp 57-70.
Gupta P, Bansal A, Samanta J, Mandavdhare H, Sharma V, Gupta V, et al (2021) Larger bore percutaneous catheter in necrotic pancreatic fluid collection is associated with better outcomes. Eur Radiol 31(5):3439-3446.
Tyberg A, Karia K, Gabr M, Desai A, Doshi R, Gaidhane M, et al (2016) Management of pancreatic fluid collections: A comprehensive review of the literature. World J Gastroenterol 22(7):2256-2270.
Besselink MG, de Bruijn MT, Rutten JP, Boermeester MA, Hofker HS, Gooszen HG, et al (2006) Surgical intervention in patients with necrotizing pancreatitis. Br J Surg 93(5):593-599.
Gupta P, Virk M, Gulati A, Muktesh G, Shah J, Samanta J, et al (2021) Unusual Sites of Necrotic Collections in Acute Necrotizing Pancreatitis: Association with Parenchymal Necrosis and Clinical Outcomes. Dig Dis Sci 66(7):2362-2367.
Delattre J-F, Levy Chazal N, Lubrano D, Flament J-B (2004) Place du drainage percutanééchoguidé dans le traitement chirurgical de la pancréatiteaiguë grave. Annales de Chirurgie 129(9):497-502.
Leppäniemi A, Tolonen M, Tarasconi A, Segovia-Lohse H, Gamberini E, Kirkpatrick AW, et al. (2019) WSES guidelines for the management of severe acute pancreatitis. World J Emerg Surg 14(1):27.
Singh AK, Samanta J, Gulati A, Gautam V, Bhatia A, Gupta P, et al. (2021) Outcome of percutaneous drainage in patients with pancreatic necrosis having organ failure. HPB (Oxford) 23(7):1030–1038.
Ke L, Dong X, Chen T, Doig GS, Li G, Ye B, et al (2021) Early on-demand drainage or standard management for acute pancreatitis patients with acute necrotic collections and persistent organ failure: A pilot randomized controlled trial. J Hepatobiliary Pancreat Sci 28(4):387-396.
Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ (1995) Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med 23:1638–1652.
Baron TH, DiMaio CJ, Wang AY, Morgan KA (2020) American Gastroenterological Association Clinical Practice Update: Management of Pancreatic Necrosis. Gastroenterology 158(1):67-75.
Wroński M, Cebulski W, Karkocha D, Słodkowski M, Wysocki L, Jankowski M, et al (2013) Ultrasound-guided percutaneous drainage of infected pancreatic necrosis. Surg Endosc 27(8):2841–2848.
Baudin G, Chassang M, Gelsi E, Novellas S, Bernardin G. Hébuterne X et al (2012) CT-guided percutaneous catheter drainage of acute infectious necrotizing pancreatitis: assessment of effectiveness and safety. AJR Am J Roentgenol 199(1):192–199.
Navalho M, Pires F, Duarte A, Gonçalves A, Alexandrino P, Távora I (2006) Percutaneous drainage of infected pancreatic fluid collections in critically ill patients: correlation with C-reactive protein values. Clin Imaging 30(2):114-119.
Freeny PC, Hauptmann E, Althaus SJ, Traverso LW, Sinanan M (1998) Percutaneous CT-guided catheter drainage of infected acute necrotizing pancreatitis: techniques and results. AJR Am J Roentgenol 170(4):969–975.
Horvath K, Freeny P, Escallon J, Heagerty P, Comstock B, Glickerman DJ, et al (2010) Safety and efficacy of video-assisted retroperitoneal debridement for infected pancreatic collections: a multicenter, prospective, single-arm phase 2 study. Arch Surg 145(9):817–825.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Verma, N., Maurya, M., Gupta, P. et al. Retroperitoneal versus transperitoneal percutaneous catheter drainage of necrotic pancreatic collections: a comparative analysis. Abdom Radiol 47, 1899–1906 (2022). https://doi.org/10.1007/s00261-022-03476-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-022-03476-7