Abstract
Intestinal pneumatosis (IP) is an infrequent radiological sign defined as pathological gas infiltration into the bowel wall. It may be associated to different underlying clinical conditions—inflammatory bowel diseases, malignancies, chemotherapy, infections, immune deficiency status, trauma, intestinal ischemia, and necrosis—that are often related to emergency state and require a prompt diagnosis. All the imaging techniques, especially abdominal radiography and Computed Tomography, could detect the presence of IP and discern the forms related to emergency conditions. The differential diagnosis is essential to start an immediate clinical or surgical management and treatment. The aim of this article is to review the radiological features of IP in different illnesses, with particular attention to differential diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intestinal pneumatosis (IP) is a rare condition that affects 0.03% of the population [1]. It is defined as pathological gas infiltration into the bowel wall. IP has been known for a long time: it was first described by Du Vernoy in 1730 [2].
Conventional radiology has a high sensitivity in recognizing air and so it has proved useful in the diagnosis of IP. Radiological detection of IP has been related to intestinal infarction in adults and to necrotizing enterocolitis (NEC) in infants. In any case, the IP discovery has long been considered a medical emergency, especially if related to porto-mesenteric vein gas (PMVG) or pneumoperitoneum (PNP) [1, 3].
With the advent of more advanced radiological techniques such as computed tomography (CT), IP has been more frequently observed in many other clinical conditions, including inflammatory bowel disease, connective tissue disease, surgery, immune deficiency or chemotherapy, with a wide variety of possible outcomes [4, 5], therefore the prognostic value of IP has been revised.
Classification and physiopathology
IP can be classified into primary (15% of cases) and secondary forms (85%). The two forms are clearly different entities with their own clinical significance and disparate therapeutic approaches [6] (Fig. 1).
The primary form consists of Pneumatosis Cystoides Intestinalis (PCI), an idiopathic gas infiltration of the bowel wall that resembles a bunch of grapes (Fig. 2).
This is the case of a 62 yo female with unexpected pneumatosis cystoides intestinalis at a CT examination who underwent for pelvic cancer follow-up. Sagittal (a) and axial (b, c) reconstructions demonstrate multiple gas-filled cysts in the submucosa of the bowel walls (a, b, arrows) and free peritoneal air (c)
Secondary forms of IP are more frequent and associated to a wide range of pathological patterns, more often related to acute intestinal ischemia. Thus, it is a radiological sign associated with a variety of pathological conditions and is not a nosographic entity itself.
The etiology of IP is unclear, in 1998 Pear introduced a classification of the major pathogenic mechanisms causally involved in intramural gas formation, which included (i) bowel necrosis, (ii) mucosal disruption, (iii) increased mucosal permeability and (iv) pulmonary diseases [7]. It is probable that different mechanisms may work in different conditions to produce IP.
Over time, in addition to Pear’s classification, three pathogenetic hypotheses have been accepted:
-
(i)
mechanical hypothesis—increase of intraluminal pressure resulting in mechanical damage to the bowel wall and leading to gas migration from the gastrointestinal lumen to the intestinal wall [8];
-
(ii)
bacterial hypothesis—aerogenic bacteria that penetrate the bowel mucosal barrier and ferment in the intestinal wall [9];
-
(iii)
pulmonary hypothesis—in chronic lung diseases, such as chronic obstructive pulmonary disease (COPD) and asthma, increased thoracic pressure causes alveolar rupture and gas diffusion towards the gastrointestinal serosa by following perivascular or perilymphatic routes [9, 10].
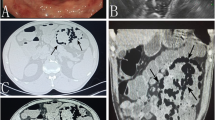
IP is a relevant radiological sign due to its strict correlation to intestinal infarct. Bowel necrosis could cause intestinal wall gas infiltration, eventually spreading in mesenteric and portal vessels (Fig. 3a–e) [11].
IP in patients with intestinal infarcts. a Small amount of gas in small bowel loop (arrows). b A predominant bubble-like pattern of IP (arrows) in a not too advanced phase. c Coronal reconstruction. An advanced phase with a circumferential pattern of IP (black arrows), gas in superior mesenteric vein and in portal branches (white arrows), and presence of peritoneal fluid close to the liver. d Coexistence of different patterns of IP, from bubble-like (white arrows) to circumferential (black arrows), presence of mesenteric fluid and fat stranding. e IP (black arrows) associated with mesenteric gas (white arrow). Association of IP and PMVG is more frequently observed in transmural bowel necrosis
Mucosal disruption has been associated with iatrogenic lesions (i.e., nasogastric tube or endoscopic maneuvers) (Fig. 4) [12] and to blunt abdominal trauma, where the sudden compression of intragastric gas can dissect the mucosa passing into the gastric wall and mesenteric veins [13]. Similarly, an increased intraluminal pressure in bowel obstruction (Fig. 5) or in the pyloric obstruction of the newborn may result in gastrointestinal passage of air [9].
In addition, mucosal damage and increased mucosal permeability may be the reason why IP is observed in conditions like cancer (Fig. 6), inflammatory diseases and intestinal infections [14].
The bacterial etiology hypothesis has been supported by analyses of the gas collected in the intramural cysts in PCI, which is characterized by high levels of hydrogen and nitrogen [15]. Intestinal cells do not produce these gasses so a bacterial origin has been hypothesized. This is also in accordance with persistence of cysts in PCI that would be difficult to explain and also with a report of a therapeutic effect of antibacterial drugs [16]. Increased mucosal permeability may be associated with subsequent aerogenic bacterial penetration and this is thought to be the reason that IP can be observed in immunosuppressed patients without other evident bowel involvement [9].
The pulmonary hypothesis has been advocated in the genesis of IP, since in several cases it has been reported the association of IP with COPD [17].
Imaging techniques
Abdominal radiography and CT are the main imaging techniques used to diagnose IP.
A proper X-ray abdomen examination should always include, in addition to upright projection or latero-lateral projection in not standing patients, a supine antero-posterior projection to analyze air distribution and better recognize IP. Gas in portal branches is visible on X-ray like linear transparencies peripherally located on the liver shadow.
CT has been shown to be more sensitive than radiography in IP [18] and PMGV detection [19].
CT scan can be performed without or with intravenous contrast agent injection. Anyway, IP in benign and asymptomatic forms may be an ancillary finding in CT examination not performed to examine the intestinal wall.
When a CT examination is focused on bowel wall analysis, especially in emergency conditions, contrast injection is mandatory. Acquisitions should be obtained in arterial and venous phases and the evaluation should be completed with multiplanar reconstructions [20, 21]. Neutral intraluminal bowel contrast is not recommended in emergency conditions; however, its use could be considered according to specific clinical indications.
In order to visualize IP, it is relevant to evaluate CT with appropriate window settings, typically a window level of − 25 Hounsfield units (HU) and window width of 500 HU allows a clear distinction between fat and air with still a fair distinction of solid parenchyma and bowel wall.
CT angiography and a careful study of the whole abdomen in the venous phase are critical in putting a radiological diagnosis. IP is an important sign arising the suspect of intestinal ischemia, but the final judgment requires a systematic search of associated signs, through a careful evaluation of intestinal lumen and wall, arterial and venous mesenteric vessels, mesentery, peritoneum and abdominal solid organs, taking in account the morphologic and the dynamic aspects, in particular searching for enlarged loops, air or fluid filled loops, air-fluid levels, thickness or thinning of the intestinal wall, PMVG, vascular thromboembolism, thickening of mesenteric folds, mesenteric edema or fat stranding, peritoneal fluid, pneumoperitoneum (PNP), bowel wall enhancement features, prominence of intestinal folds, solid organs enhancement features (Fig. 7).
Ultrasonography (US) was also used in detecting IP [22]; however, US detection of IP is not easy for the disturbing effects of intraluminal air and this technique is mainly used, but nor exclusively, in newborns.
Occasionally IP may be detected on MRI, anyway MRI has little indication in the study of IP and related conditions [23, 24] (Fig. 8).
Primary form of IP: PCI
The primary form of IP is represented by PCI, an idiopathic gas infiltration of the bowel wall disposed as a bunch of grapes.
PCI, according to Jamart [25], primarily affects the small intestine, but it has also been described in the large intestine and some authors report a higher frequency in this part of the intestine [26, 27]. Recently, Ling [28] and Wu [29] reported that in a Chinese ethnic cohort colonic localization was more frequent, with a colon/small bowel ratio of 1.3:1. There is a high variability in the different reports in the male/female distribution: Horiuki et al. [30] report a higher frequency in women, while Wu et al. [29] report that PCI is more frequent in males (male/female ratio of 2.4:1). It is likely that these conflicting reports are a consequence of the low number of observed cases.
PCI is generally a benign pathological condition but can also present with sub-occlusion [31] and require surgery. PCI may be associated with PNP which can spontaneously reabsorb [32].
In the majority of cases, there are no symptoms associated to PCI; however, when present clinical manifestations of PCI are non-specific: it may present with abdominal pain (59%), diarrhea (53%), nausea and vomiting (14%), mucus in stool (12%) and hematochezia (12%) [29]. These symptoms are often a consequence of PCI’s complications, including peritoneal irritation due to PNP, volvulus, intestinal obstruction or ischemia, that occur in 3% of cases and could require urgent surgical intervention [33]. Cases have been described in which PCI is associated to intussusception; in these cases, PCI can be considered as a cause of obstruction [34], or instead as the effect of the obstruction [35].
In PCI, abdominal X-ray usually shows multiple gas pockets or small round lucencies in the bowel wall. Contrast-enhanced CT may better reveal intramural gas, often disposed as a bunch of grapes, and the regular and non-inflamed mucosa that surround the air cysts. This intramural gas could spread in the portal venous system or it could be associated to a small volume of PNP (Fig. 2).
A feature of PCI is the mismatch between the impressive radiological signs in front of minimal or absent clinical signs.
Secondary forms
Secondary forms of IP are more frequent than PCI (85% vs 15%) and may occur in a wide range of pathological conditions, as inflammatory bowel diseases, malignancies and chemotherapy, infections, immune deficiency status, trauma or medical maneuvers, but it is a sign mainly related to intestinal ischemia and necrosis [36].
In secondary forms, IP is a radiological sign and not an illness in itself [36], then it does not have a proper clinical expression and its symptoms depend on the underlying disease. IP is usually associated to late phase of intestinal ischemia and infarction is usually seen in late phase, requiring a very prompt diagnosis to start an immediate and aggressive treatment. Conversely, IP induced by the mentioned non-ischemic causes commonly shows a less aggressive clinical course and often requires conservative management rather than surgery [37].
In the secondary IP, the radiological appearances are more varied. It is better detected and evaluated with CT scans, which is the gold standard technique to detect IP and should be used in adults in any case in which either X-rays or US raise the suspicion and in any patient with abdominal acute symptoms.
Intestinal ischemia
Acute mesenteric ischemia is a life-threatening condition caused by decreased blood flow to the bowel [20]. Its clinical findings are non-specific, as abdominal pain, often more severe than that expected on the basis of physical examination, nausea, vomiting, and diarrhea [20], therefore clinical diagnosis may be difficult. In case of acute ischemia, abnormal laboratory tests include leukocytosis, hemoconcentration, metabolic acidosis, and elevated levels of lactate, LDH, D-dimer, amylase and liver enzymes [21]. Notably, an increased lactate level is often a late marker of intestinal infarct [38]. Although laboratory tests are useful, diagnosis more often requires a CT confirmation [39].
IP is a frequent radiological sign of acute intestinal ischemia and its early recognition is of high value because permits the immediate surgical treatment and the appropriate medical supportive therapy, with consequent prevention of necrosis [37, 40, 41].
IP may be detected with X-rays, which can also clarify its pattern and distribution, presence of PMVG and other associated findings that can direct radiologists’ and clinicians’ attention towards a specific diagnosis. Nowadays, X-ray is used in newborns [42] (Fig. 9a–d), while in adults it has been overtaken by CT scans [10, 43].
On CT, IP usually appears as a linear and/or bubbly pattern of intramural gas associated to additional findings as thin bowel wall, absent or reduced mucosal enhancement, dilated bowel, ascites and arterial occlusion [19]. IP is sometimes associated with PMVG, that is differentiated from pneumobilia in X-rays by its characteristic tubular branching lucencies that extend to the periphery of the liver, whereas biliary air is more central [1].
Furthermore, IP in intestinal infarction has been considered an indicator of poor prognosis related to advanced necrosis [44], notably if it is associated to PMVG. These data have been studied by Wiesner et Al., who analyzed 23 patients and concluded that bubble-like IP may be related to partial mural bowel ischemia, while a band-like pattern of IP in association with PMVG was associated to transmural bowel infarction. In their experience, IP and PMVG were associated to a mortality rate of 44% and 56%, respectively, whereas when IP and PMVG were simultaneously present, the mortality rate increased up to 72% [45].
Greenstein et al. retrospectively studied IP in 40 patients over 10 years. They found an overall surgical rate of 35% with hospital mortality rate of 20%. The authors showed how combining radiological findings with clinical and laboratory results led to better management and better prognostic evaluation of IP [46].
In our previous experience, 52% of IP in adults was related to intestinal infarction with a mortality rate of 30.4%, rising to 50% when associated with PMVG [47].
In strong agreement with our data, Treyaud et al. reported bowel ischemia in 53.7% of IP detected on CT and in 69.6% when PMVG was also present. In this study, the only other radiological sign related to ischemia was the reduction of intestinal bowel wall enhancement. These authors also emphasize the importance of clinical and laboratory data [48].
NEC
NEC is a pediatric disease that mostly affects the premature infants’ intestine. The intestinal wall is invaded by bacteria, which cause local infection and inflammation, resulting in a bowel wall destruction.
In newborns IP may be a good indicator of NEC, usually starting from distal ileus and right colon, spreading then to the entire intestine and eventually evolving to bowel necrosis (Fig. 9a–d).
In contrast, IP in infants is not pathognomonic for NEC, but when associated to abdominal distension, hematochezia, paralytic ileus, NEC becomes a probable diagnosis. In non-neonatal pediatric patients, Kurbegov found that all of their patients with IP associated with PMVG had necrotic bowel, all of them required surgery or died before intervention [49].
Bowel US may be a useful adjunct to abdominal X-ray in the evaluation of infants with clinical suspicion of NEC, avoiding radiation exposure in this radio-sensitive population such as children [50]. In IP, US shows hyperechoic dots and lines in the edematous thickened bowel wall, while detection of sub-serosal gas could be more difficult because of the presence of concurrent intraluminal air [51].
IP, thick bowel wall (> 2.5 mm), PMVG ,and reduced peristalsis are independent diagnostic factors associated with NEC [52]. Cuna et al. in a meta-analysis found that US has low sensitivity but high specificity for diagnosis of NEC [53]. Direct US recognition of IP has been made in other emergencies in infants, James and Itazaki reported cases of intussusception [54, 55].
CT is rarely performed in children due to its invasiveness, but it could be appropriate in complicated cases to detect IP and related PMVG (Fig. 10).
Other
Other recognizable cases of IP include infection [36], recent abdominal traumas [13], iatrogenic gastrointestinal lesions (Fig. 4) [12], inflammatory bowel diseases (IBD), cancer (Fig. 6) and immunosuppression [14].
In these cases, IP is a sign associated to the typical radiological findings of the underlying disease (Table 1).
In IBDs, fever, weight loss, and recurrent sub-occlusive symptoms are frequent clinical findings, related to radiological stenotic pattern with high contrast-enhancement of the ileal wall.
IP may be associated to bowel cancer, where obstruction, rectal bleeding, fatigue and weight loss are typical symptoms and CT scan permits direct visualization of cancer and its complications.
Moreover, abdominal traumas or iatrogenic gastrointestinal lesions may present with IP, often associated to active bleeding, mucosal disruption, fractures and/or other trauma’s complications.
A relatively frequent clinical situation in which IP may occur is bowel obstruction (Fig. 5) [46]. In this case patients’ clinical presentation may be acute and the recognition of a cause of obstruction or a transition point should guide the radiologist. In some cases, intestinal necrosis and obstruction can be present simultaneously, this happens in the case of a twisted loop or of an internal or external hernia [42, 43].
Differential diagnosis
The distinction between PCI and the secondary form of IP is usually straightforward, since the morphological findings are quite different in the two forms.
On plain films it is very difficult to confidently detect IP, especially when there are enlarged bowel loops, PNP and/or retropneumoperitoneum. Possible pitfalls are superimposition of loops that may create false images (Fig. 11) or retropneumoperitoneum that may mimic IP (Fig. 12).
It is easier to detect PMVG, because of the linear transparencies on the liver shadow. In this case the radiologist has to take care to distinguish PMVG from pneumobilia and to recognize accompanying radiological signs, since portal air embolization may occur after umbilical catheterization.
US plays a role in the diagnosis of PMVG, because of the good detection of gas in portal branches. It is important to not confuse PMVG with pneumobilia—a distinction based on a correct recognition of portal vessels, ultimately using color doppler analysis. PMVG usually spreads peripherally in the liver, whereas pneumobilia has more typically a more central distribution toward hepatic hilum (Fig. 13) [1, 12].
As said before, CT is the gold standard technique in detection of both primary and secondary forms of IP. PCI has a specific radiologic pattern defined by multiple clusters of rounded cystic gas collections in the bowel wall, involving either the small or large bowel [47, 56].
The cystic presentation is more often associated to a benign cause [31], this pattern may also be misinterpreted in both senses: bowel content (Fig. 14a) and intestinal folds (Fig. 14b) can trap bubbles of air mimicking IP [55], so that false negative and false positive are possible. Usually trapped bubbles are located in the anterior part of the loop (Fig. 14c), whereas localization of IP is completely independent of position [57, 58].
a Bubbles surrounding semisolid intestinal content in cecum. In this case, gas bubbles are trapped in feces and not within the bowel wall. The patient did not have any abdominal acute complaint. b Bubbles entrapped in intestinal folds in the anterior part of the bowel. The radiological context, characterized by enlarged loops with hydro-aerial levels in the small bowel, is compatible with the diagnosis of intestinal infarction, but the exclusive anterior location of gas is not that of IP. c Another case of gas confined anteriorly in small bowel lumen simulating IP
In secondary forms of IP, the different morphologic patterns of gas distribution are described as linear, circumferential, and bubble-like (Figs. 3, 5, 6) [36].
Linear pattern of IP has been more frequently related to intestinal infarction in adults, with a rate of 75.5% [31]. Moreover, linear pattern is also associated to NEC in newborns and infants.
On the other hand, bubble-like gas distribution, more often associated to a benign cause [31], maybe also related to transmural bowel infarction, in accordance to Wiesner et al. [45].
Therefore, in secondary forms of IP, acute intestinal ischemia must always be excluded by the differential diagnoses since it requires immediate clinical and surgical management.
Conclusion
IP is a crucial sign in recognition of intestinal infarction in emergency situation, since it is a frequently associated sign, especially when PMVG is also present.
It may also be benign or associated with a wide range of non-ischemic causes, although it is fundamental to promptly exclude medical emergencies as intestinal ischemia or necrosis in differential diagnosis.
However, diagnosis of intestinal infarction cannot rely on this single sign, but rather on a series of signs in their proper radiological and clinical context. Thus, IP in patients with abdominal emergencies should prompt a careful search for associated findings and point clinicians to the possible presence of bowel necrosis.
Abbreviations
- IP:
-
Intestinal pneumatosis
- NEC:
-
Necrotizing enterocolitis
- PMVG:
-
Porto-mesenteric vein gas
- PNP:
-
Pneumoperitoneum
- CT:
-
Computed tomography
- PCI:
-
Pneumatosis cystoides intestinalis
References
Ho LM, Paulson EK, Thompson WM (2007) Pneumatosis intestinalis in the adult: benign to life-threatening causes. AJR Am J Roentgenol 188(6):1604-13.
Du Vernoy JG (1730) Aer intestinorum tam sub extima quam intima tunica inclusus: observationes anatomicae: comment. Acad Acient Imp Petropol 5:213-25
Na SY, Kim KJ, Yang DH, Jung K, Ye B, Byeon JS, et al (2011) Pneumoperitoneum in a patient with ulcerative colitis after sigmoidoscopy: is this always an indication for surgery? Inflamm Bowel Dis 17(6):E54-6.
Hoot NR, Pfennig CL, Johnston MN, Jones I (2013) An incidental finding? Pneumatosis intestinalis after minor trauma. J Emerg Med 44(2):e145-7.
Kirmanidis M, Boulas KA, Paraskeva A, Kariotis I, Barettas N, Kariotis S, Keskinis C, Hatzigeorgiadis A (2018) Extensive colonic pneumatosis in a patient on adjuvant chemotherapy after right colectomy for primary terminal ileum lymphoma: A decision-making process between surgical and non-surgical management. International Journal of Surgery Case Reports 52:84–88.
Feczko PJ, Mezwa DG, Farah MC, White BD (1992) Clinical significance of pneumatosis of the bowel wall. Radiographics 12(6):1069-78.
Pear BL (1998) Pneumatosis intestinalis: a review. Radiology 207:13-9.
Mazzei MA, Guerrini S, Cioffi Squitieri N, Genovese EA, Mazzei FG, Volterrani L (2012) Diagnosis of acute mesenteric ischemia/infarction in the era of multislice CT. Recenti Prog Med 103(11):435-7.
Khail PN, Huber-Wagner S, Ladurner R, Kleespies A, Siebeck M, Mutschler W, Halfeldt K, Kanz KG (2009) Natural history, clinical pattern, and surgical consideration of pneumatosis intestinalis. Eur J Med Res 14(6):231–9.
Keyting WS, McCarver RR, Kovarik JL, Daywitt AL (1961) Pneumatosis intestinalis: a new concept. Radiology 76:733–41.
Florim S, Almeida A, Rocha D, Portugal P (2018) Acute mesenteric ischaemia: a pictorial review. Insights Imaging 9(5):673–682.
Lassandro F, Scaglione M, Rossi G, Grassi R, Romano L (2002) Portomesenteric vein gas: diagnostic and prognostic value. Emerg Radiol 9(2):96-9.
Solazzo A, Lassandro G, Lassandro F (2017) Gastric blunt traumatic injuries: A computed tomography grading classification. World J Radiol 9(2):85-90.
Mitsuyoshi A, Hamada S, Tachibana T, Momono T, Aoyama H, Kondo Y, Inoguchi K, Yokoyama D, Nakau M, Suzaki S, Okabe H, Yanagibashi K (2015) Pathogenic mechanisms of intestinal pneumatosis and portal venous gas: should patients with these conditions be operated immediately? Surg Case Rep 1:104.
Wang Y, Wang Y, Zheng Y, Jiang H, Zhang J (2018) Pneumatosis cystoides intestinalis: six case reports and a review of the literature. BMC Gastroenterol 18:100.
Gillon J, Tadesse K, Logan RF, Holt S, Sircus W (1979) Breath hydrogen in pneumatosis cystoides intestinalis. Gut 20:1008-11.
Iida A, Naito H, Tsukahara K, Yumoto T, Nosaka N, Kawana S, Sato K, Takeuchi N, Soneda J, Nakao A (2017) Pneumatosis cystoides intestinalis presenting as pneumoperitoneum in a patient with chronic obstructive pulmonary disease: a case report. Journal of Medical Case Reports 11:55.
Caudill JL, Rose BS (1987) The role of computed tomography in the evaluation of pneumatosis intestinalis. J Clin Gastroenterol 9:223–226.
Schindera ST, Triller J, Vock P, Hoppe H (2006) Detection of hepatic portal venous gas: its clinical impact and outcome. Emerg Radiol 12:164–170.
Fitzpatrick LA, Rivers-Bowerman MD, Thipphavong S, Clarke SE, Rowe JA, Costa AF (2020) Pearls, Pitfalls, and Conditions that Mimic Mesenteric Ischemia at CT. Radiographics 40(2):545-561.
Ginsburg M, Obara P, et al (2018) ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia. J Am Coll Radiol 15(11S):S332–S340.
Goskeet A, Goske MJ, Goldblum JR, Applegate KE, Mitchell CS, Bardo D (1999) The “circle sign”: A new sonographic sign of pneumatosis intestinalis – Clinical, pathologic and experimental findings. Pediatr Radiol 29:530-5.
Saba L, Berritto D, Iacobellis F, Scaglione M, Castaldo S, Cozzolino S, Mazzei MA, Di Mizio V, Grassi R (2013) Acute arterial mesenteric ischemia and reperfusion: Macroscopic and MRI findings, preliminary report. World J Gastroenterol 19:6825–33.
Mazzei MA, Guerrini S, Cioffi Squitieri N, Imbriaco G, Chieca R, Civitelli S, Savelli V, Mazzei FG, Volterrani L (2013) Magnetic resonance imaging: Is there a role in clinical management for acute ischemic colitis? World J Gastroenterol 19:1256–63.
Jamart J. (1979) Pneumatosis cystoides intestinalis. A statistical study of 919 cases. Acta Hepatogastroenterol (Stuttg) 26:419–422.
Kim KM, Lee CH, Kim KA, Park CM (2007) CT Colonography of pneumatosis cystoides intestinalis. Abdom Imaging 32:602–605.
Morris MS, Gee AC, Cho SD, Limbaugh K, Underwood S, Ham B, Schreiber MA (2008) Management and outcome of pneumatosis intestinalis. Am J Surg 195(5):679–82.
Ling F, Guo D, Zhu L (2019) Pneumatosis cystoides intestinalis: a case report and literature review. BMC Gastroenterology 19:176.
Wu L, Yang Y, Dou Y, Liu Q (2013) A systematic analysis of pneumatosis cystoids intestinalis. World J Gastroenterol 19(30):4973-4978.
Horiuchi A, Akamatsu T, Mukawa K, Ochi Y, Arakura N, Kiyosawa K (1998) Pneumatosis cystoides intestinalis associated with post-surgical bowel anastomosis: a report of three cases and review of the Japanese literature. J Gastroenterol Hepatol 13:534-537.
Attar A, Pocard M, Messing B (2005) Pneumatosis cystoides intestinalis in primary intestinal pseudo-obstruction: a nonsurgical cause of pneumoperitoneum. Clin Gastroenterol Hepatol 3:A21.
Vischio J, Matlyuk-Urman Z, Lakshminarayanan S (2010) Benign spontaneous pneumoperitoneum in systemic sclerosis. J Clin Rheumatol 16(8):379-81.
Galandiuk S, Fazio VW (1986) Pneumatosis cystoides intestinalis. A review of the literature. Dis Colon Rectum 29(5):358-63.
Ahrar K, Watkins GE, Gardiner G (1997) Colocolic intussusception caused by pneumatosis cystoides coli. Abdom Imaging 22:392-94.
Shaheen O, Ahmad W, and Mhammad NA (2019) Gastric Outlet Obstruction and Sigmoid Volvulus in a Patient with Pneumatosis intestinalis: An Etiology or a Complication. Case Rep Surg, 4065749.
Soyer P, Martin-Grivaud S, Boudiaf M, et al (2008) Linear or bubbly: a pictorial review of CT features of intestinal pneumatosis in adults. J Radiol 89:1907–1920.
Ko S, Hong SS, Hwang J, Kim HJ, Chang YW, Lee E (2018) Benign versus life-threatening causes of pneumatosis intestinalis: differentiating CT features. Rev Assoc Med Bras (1992) 64(6):543-548.
Tilsed JVT, Casamassima A, Kurihara H, Mariani D, Martinez I, Pereira J, Ponchietti L, Shamiyeh A, al-Ayoubi F, Barco LAB, Ceolin M, A. D’Almeida AJG, Hilario S, Olavarria AL, Ozmen MM, Pinheiro LF, Poeze M, Triantos G, Fuentes FT, Sierra SU, Soreide K, Yanar H (2016) ESTES guidelines: acute mesenteric ischaemia. Eur J Trauma Emerg Surg 42:253–270.
Kyang LS, Srinivasan R, Singh V (2019) Acute gastric volvulus with pneumatosis intestinalis and portal venous gas secondary to hiatus hernia induced gastric outlet obstruction. Images for Surgeons 89(12):582-E583.
Mazzei MA, Volterrani L (2015) Nonocclusive mesenteric ischaemia: think about it. Radiol Med 120(1):85-95.
Mazzei MA, Guerrini S, Cioffi Squitieri N, Vindigni C, Imbriaco G, Gentili F, Berritto D, Mazzei FG, Grassi R, Volterrani L (2016) Reperfusion in non-occlusive mesenteric ischaemia (NOMI): effectiveness of CT in an emergency setting. Br J Radiol 89(1061):20150956.
Kim D, Lee J, Yeh J (2013) Pneumatosis Intestinalis on Plain Film. The Journal of Emergency Medicine 44(1):175–176.1.
Jenkins M, Courtney H, Pope E, Williamson J (2017) A case report and approach to management in pneumatosis intestinalis. Annals of Medicine and Surgery 23:25-27.
Guerrini S, Bucalossi A, Cioffi Squitieri N, Mazzei FG, Volterrani L, Mazzei MA (2016) Ischemic colitis diagnosed by magnetic resonance imaging during lenalidomide treatment in a patient with relapsed multiple myeloma. Tumori 102(2).
Wiesner W, Mortelé KJ, Glickman JN, Ji H, Ros PR (2001) Pneumatosis Intestinalis and Portomesenteric Venous Gas in Intestinal Ischemia: Correlation of CT Findings with Severity of Ischemia and Clinical Outcome. AJR 177:1319–1323.
Greenstein AJ, Nguyen SQ, Berlin A, Corona J, Lee J, Wong E, Factor SH, Divino CM (2007) Pneumatosis intestinalis in adults: management, surgical indications, and risk factors for mortality. J Gastrointest Surg 11(10):1268-74.
Lassandro F, Mangoni di Santo Stefano ML, Porto AM, Grassi R, Scaglione M, Rotondo A (2010) Intestinal pneumatosis in adults: diagnostic and prognostic value. Emerg Radiol 17(5):361-5.
Treyaud MO, Duran R, Zins M, Knebel JF, Meuli RA, Schmidt S (2017) Clinical significance of pneumatosis intestinalis - correlation of MDCT-findings with treatment and outcome. Eur Radiol 27(1):70-79.
Kurbegov AC, Sondheimer JM (2001) Pneumatosis intestinalis in non-neonatal pediatric patients. Pediatrics 108(2):402-6.
James V, Aswin W, Khai PL, Ong GY (2017) Point-of-care ultrasound identification of pneumatosis intestinalis in pediatric abdominal pain: a case report Crit Ultrasound J 9:2.
Stranzinger E, Di Pietro MA, Yarram S, Khalatbari S, Strouse PJ (2009) Intramural and subserosal echogenic foci on ultrasound in large bowel intussusception. Prognostic indicator for reducibility? Pediatr Radiol 39(1):42–46.
Chen S, Hu Y, Liu Q, Li X, Wang H, Wang K, Zhang A (2019) Application of abdominal sonography in diagnosis of infants with necrotizing enterocolitis. Medicine 98(28):e16202.
Cuna AC, Lee JC, Robinson AL, Allen NH, Foley JE, Chan SS (2018) Bowel Ultrasound for the Diagnosis of Necrotizing Enterocolitis: A Meta-analysis. Ultrasound Q 34(3):113-118.
James V, Warier A, Lee KP, Ong GY (2017) Point-of-care ultrasound identification of pneumatosis intestinalis in pediatric abdominal pain: a case report. Crit Ultrasound J 9(1):2.
Itazaki Y, Tsujimoto H, Ito N, Horiguchi H, Nomura S, Kanematsu K, Hiraki S, Aosasa S, Yamamoto J, Hase K (2016) Pneumatosis intestinalis with obstructing intussusception: A case report and literature review. World J Gastrointest Surg 27;8(2):173-178.
Berritto D, Iacobellis F, Mazzei MA, et al (2016) MDCT in ischaemic colitis: how to define the aetiology and acute, subacute and chronic phase of damage in the emergency setting. Br J Radiol 89(1061):20150821.
Lassandro F, Valente T, Rea G, Lassandro G, Golia E, Brunese L, Laghi A (2015) Imaging assessment and clinical significance of pneumatosis in adult patients. Radiol Med 120(1):96-104.
Mazzei MA, Guerrini S, Lucii G, Mazzei FG, Volterrani L (2020) Bowel obstruction and intestinal ischemia: warnings for radiologists. Abdom Radiol (NY) 45(3):887-88.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare we have not conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lassandro, G., Picchi, S., Romano, F. et al. Intestinal pneumatosis: differential diagnosis. Abdom Radiol 47, 1529–1540 (2022). https://doi.org/10.1007/s00261-020-02639-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02639-8