Abstract
Contrast-enhanced ultrasound (CEUS) has become an established modality in various clinical indications for liver diseases. SonoVue®, a pure blood pure agent, and Sonazoid®, which exhibits an additional Kupffer phase, are contrast agents approved for liver imaging. This review discusses and compares the current clinical evidence for these two ultrasound contrast agents in the characterization and detection of focal liver lesions in the non-cirrhotic and cirrhotic liver, as well as for the use in interventional procedures such as liver biopsy guidance, and local ablation treatment monitoring. Reference is made to clinical studies which evaluated the accuracy of CEUS using a standard of reference, its safety, or to comparative studies of these two agents.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ultrasound has proven to be a useful tool for liver disease diagnosis and treatment follow-up, due to its continuous real-time imaging capability, non-invasiveness, low cost compared to other imaging modalities, and bed-side convenience[1,2,3]. The introduction of ultrasound contrast agents has significantly expanded the role of ultrasonography in the management of patients with liver disease, both for diagnosis and for treatment guidance and follow-up. Indeed, contrast-enhanced ultrasound (CEUS) in liver imaging has been used in the European and Asiatic countries for more than 10 years.
SonoVue® (Bracco Imaging SpA, Italy) and Sonazoid® (GE Healthcare Norway) are two second generation contrast agents approved for clinical use in CEUS of the liver in more than one country. SonoVue was first approved in 2001 in 15 European countries, and is currently registered in 44 countries, with global sales of over 1 million units in 2018, and has an extensive publication record [4,5,6]. Sonazoid was launched in Japan in 2007, and is currently registered in 4 countries, with sales of approximately 77,000 units in 2017 [7]. SonoVue, as the other second generation contrast agents Definity and Optison, is a pure blood pool agent; Sonazoid exhibits an additional Kupffer phase [1]. Although a few studies have reported on the efficacy of Sonazoid-enhanced US compared to the use of SonoVue, a systematic analysis and comparison of the available evidence based on clinical studies with these two contrast agents is lacking [8, 9]. Therefore, the aim of this review is to summarize the existing publications for CEUS of the liver using SonoVue and Sonazoid in the diagnosis of focal liver lesions (FLLs) and for CEUS guided liver interventions.
A dedicated literature search was conducted in PubMed up to April 2019 to identify original papers and meta-analyses for CEUS of the liver using SonoVue and/or Sonazoid. Selected were publications that used an independent standard of reference to assess the accuracy of these two agents. Identified indications were characterization or detection of FLLs in the non-cirrhotic or cirrhotic liver, and for CEUS guidance of liver interventions. Two papers were published later on during the preparation of the manuscript, a safety work on Sonazoid (71) in June 2019 (e-pub) and a multicenter study performed with Sonazoid for HCC surveillance published in September 2019 (49), which were additionally included in this review.
References that focused on the safety of CEUS with these two agents were also reviewed. The results of this analysis were presented and discussed during a meeting that took place in Beijing on April 30th 2019, involving International and Chinese CEUS users with the aim of developing a consensus of the value of CEUS of the liver with SonoVue and Sonazoid in the various indications. The discussion was based upon the clinical evidence on diagnostic performance, safety, patient management, and other practical concerns.
Materials and methods
This is a review paper therefore IRB approval was not required. A dedicated literature search was conducted in PubMed to identify original papers and meta-analyses for CEUS of the liver using SonoVue and/or Sonazoid. Selected were publications that used an independent standard of reference to assess the accuracy of these two agents. Identified indications were characterization or detection of FLLs in the non-cirrhotic or cirrhotic liver, and for CEUS guidance of liver interventions. References that focused on the safety of CEUS with these two agents were also reviewed. The results of this analysis were presented and discussed during a meeting that took place in Beijing on April 30th 2019, involving International and Chinese CEUS users with the aim of developing a consensus of the value of CEUS of the liver with SonoVue and Sonazoid in the various indications. The discussion was based upon the clinical evidence on diagnostic performance, safety, patient management, and other practical concerns.
Background information
SonoVue and Sonazoid microbubbles are second-generation ultrasound contrast agents, with greater stability than first-generation agents [1]. SonoVue consists of a monolayer phospholipid shell encasing a core of inert sulfur hexafluoride gas (SF6) [10]. The shell of Sonazoid is composed of hydrogenated egg phosphotidylserine (HEPS) with a perfluorobutane (PFB) core [11]. A summary of the characteristics of each agent, including composition of the microbubbles, their distribution after injection, and technical imaging aspects, is presented in Table 1.
Following intravenous injection, SonoVue does not diffuse into the extravascular space but remains in the blood vessels (with maximum concentrations occurring within 1 to 2 min after a single administration) until SF6 dissolves in the blood and is rapidly eliminated with expired air [12]. The maximum concentration of Sonazoid in the blood is also observed shortly after its intravenous administration; elimination of PFB is also via the lungs [13]. Sonazoid microbubbles are phagocytosed by the Kupffer cells (starting approximately 1 min after administration) and remain stable in these resident macrophages in the liver sinusoids, thus providing prolonged enhancement of the liver parenchyma up to 2 h post-injection [13,14,15,16].
Due to the dual blood supply of the liver from the hepatic artery (25–30%) and the portal vein (70–75%), three phases of vascular enhancement can be observed in CEUS with SonoVue: the arterial phase that starts within 10–20 s and continues up to 45 s post-injection; the portal venous phase that is characterized by arrival of the contrast agent also through the portal system and lasts up to 2 min post-injection; and the late phase during which the microbubbles are progressively cleared from the liver parenchyma (up to 5 min post-injection) [1]. For Sonazoid, because of the Kupffer cell uptake starting approximately 1 min after administration, the observed enhancement after 1 min represents a combination of the vascular phase and the Kupffer phase [16]. The pure Kupffer phase (also called post-vascular phase) starts approximately 10 min post-injection, when the microbubbles have been eliminated from the blood pool, and lasts up to 2 [16]. In order to avoid overlap with the prior vascular phases, scanning in the Kupffer phase should not start earlier than 10 min from administration of Sonazoid [1]. A complete examination with SonoVue comprising all three vascular phases usually lasts less than 5 min; an examination with Sonazoid, because of the Kupffer phase, extends to more than 10 min. This difference in examination time between the two agents might become even more pronounced in cases where a re-injection of contrast agent would be required.
A low mechanical index (MI) technique is used in CEUS with second-generation contrast agents, affording continuous real-time scanning that was not possible with first-generation agents [1]. Sonazoid may require the use of slightly higher mechanical index than SonoVue due to the higher stiffness of the shell [8]. Some authors have reported higher sensitivity using high mechanical index contrast modes (0.7–1.2) with Sonazoid compared to low mechanical index (0.21–0.23) in detecting Sonazoid microbubbles in normal liver parenchyma and in detecting hypervascular hepatocellular carcinomas as perfusion defects in the Kupffer cell phase [17, 18].
The enhancement patterns observed in each vascular phase, in real time, lead to the identification and characterization of lesions in the cirrhotic and non-cirrhotic liver [1, 19]. A complete description of characteristic lesion enhancement patterns and current lexicon is beyond the scope of this paper, and the reader is referred to the Guidelines and Good Clinical Practice Recommendations for Contrast Enhanced Ultrasound (CEUS) in the Liver, and Contrast-enhanced ultrasound of the liver: technical and lexicon recommendations from the ACR CEUS LI-RADS working group [1, 20]. The ACR LI-RADS report released in 2017 includes only pure blood pool agents.
Clinical evidence
Focal liver lesion characterization
CEUS should be used for the characterization of FLLs when patients have incidental findings at unenhanced ultrasound, are at high risk for hepatocellular carcinoma, cannot undergo other imaging modalities for safety reasons (e.g., renal insufficiency), have indeterminate lesions or conflicting results from other imaging studies, or prior to certain interventional procedures [1, 19, 21, 22]. Continuous CEUS imaging with purely vascular agents in real time permits the assessment of characteristic early and late wash out enhancement patterns [20]. The vast majority of clinical evidence for CEUS in FLL characterization comes from SonoVue, while much less is known for Sonazoid.
A meta-analysis by Friedrich-Rust et al. on contrast-enhanced ultrasound for the differentiation of benign and malignant focal liver lesion included 35 papers with SonoVue out of a total of 45 publications. The 35 SonoVue studies comprised a total of 7231 focal liver lesions, 4221 of which were malignant. The pooled sensitivity was 93% (range 91–95%) and the pooled specificity was 90% (88–93%). As described by the authors, this meta-analysis included studies on cirrhotic and non-cirrhotic patients, however, only studies evaluating more than one entity of FLLs were included to exclude a bias from patient selection [23].
The meta-analysis performed by Niu et al. on contrast-enhanced ultrasonography for the diagnosis of small hepatocellular carcinoma lesions (≤ 2 cm) included 15 publications, 12 of which presented data for SonoVue [24]. The 12 SonoVue papers included a total of 778 patients (878 lesions) and showed a pooled sensitivity of 84% (77–90%) and pooled specificity of 89% (81–94%).
A meta-analysis of the diagnosis value of focal liver lesions with SonoVue-enhanced ultrasound compared with contrast-enhanced computed tomography (CECT) and contrast-enhanced magnetic resonance imaging (CEMRI) was performed by Guang et al. [25] It included 10 SonoVue studies, 9 studies with CECT and 10 studies with CEMRI; 2646 patients (2981 lesions) were included. Only studies evaluating more than one entity of focal liver lesions were included in the present study to exclude a bias from prior patient selection. However, these selection criteria may have caused a bias themselves, as the approach to focal liver lesions in cirrhotic and non-cirrhotic livers is different. Therefore, the results of the present meta-analysis will differ from results performed in special patient groups (e.g., series of small focal liver lesions or cirrhosis).
The pooled sensitivity was 88% (87–90%), and the pooled specificity was 81% (79–84%) for SonoVue-enhanced ultrasound. Among the 3 techniques, SonoVue-enhanced ultrasound had the highest specificity, and CECT had the highest sensitivity (90%, (88–92%)); however, there was no significant statistical difference between CECT or CEMRI and SonoVue-enhanced ultrasound.
In a guidance and systemic review of the literature from the National Institute for Health and Care Excellence (United Kingdom), the clinical effectiveness of CEUS with SonoVue in the published literature for the characterization of FLLs identified either from routine monitoring of cirrhotic patients, or as incidental findings, was examined in comparison with CECT and/or CEMRI [26, 27]. A health economic analysis was also included. Seven of the published studies identified in the literature search were conducted in cirrhotic patients undergoing routine monitoring with unenhanced US and concerned the differentiation of hepatocellular carcinoma (HCC) versus other lesion types in small to medium (< 30 mm) FLLs. There was no consistent evidence for any significant difference in test performance among CEUS, CECT and CEMRI; CEUS with SonoVue showed sensitivity and specificity values around 90% for characterization of FLLs 11–30 mm in size. The primary outcome measure in the published studies conducted in patients with FLLs incidentally detected at unenhanced US was differentiation between malignant and benign lesions. All studies reported no significant differences among the 3 imaging modalities. The pooled estimates of sensitivity for diagnosis of “any liver malignancy” were approximately 95% for both CEUS with SonoVue and CECT. The pooled estimates of specificity were 94% and 93%, respectively. One study comparing CEUS with CEMRI found similar sensitivity and specificity values for both modalities. It was concluded that SonoVue CEUS could provide similar diagnostic performance to other imaging modalities (CECT and CEMRI) for the assessment of FLLs. Economic analyses indicated that CEUS was a cost-effective replacement for CEMRI. The use of CEUS instead of CECT was considered cost-effective in the surveillance of cirrhosis and the characterization of incidentally detected FLLs, with similar costs and effects for the detection of liver metastases from CRC.
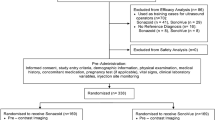
A Phase III study sponsored by GE Healthcare, compared the efficacy and safety of Sonazoid and SonoVue in patients with FLLs undergoing pre- and post-contrast ultrasound imaging; a total of 424 patients received either Sonazoid or SonoVue [9]. The study is not published at the time of submission of this manuscript and only summary results are available from the registry of clinical trials run by the United States National Library of Medicine (clinicaltrials.gov NCT03335566) and from an abstract presented at the 16th World Federation for Ultrasound in Medicine and Biology Congress. The primary endpoint of the study was the percentage of patients with accuracy improvement in post-contrast versus pre-contrast ultrasound for diagnosis of the liver target lesion as malignant or benign; histopathology, CECT, or CEMRI were the reference standard in the study. Ultrasound images, pre- and post-contrast, were evaluated by three blinded readers. Improvement in accuracy across the three readers ranged from 17 to 22.1% among patients who received Sonazoid and from 14.6 to 24.2% among those who received SonoVue. The improvement in accuracy was statistically significant for 1 reader with Sonazoid (p = 0.033), and 1 other reader for SonoVue (p = 0.012). The investigators concluded that Sonazoid and SonoVue were similar in diagnosing FLLs as benign or malignant.
A recently published study with a comparative parallel group design assessed the efficacy of Sonazoid and SonoVue in the characterization of FLL in 65 patients with at least one hepatic lesion [8]. Like the phase III study above, the primary objective was to test accuracy improvement compared to unenhanced ultrasound, which was not significantly different for the two agents. The sensitivity for diagnosis of HCC, metastasis, hemangioma, FNH, or other benign lesions ranged between 83.3 and 100% for SonoVue and between 84.6 and 100% for Sonazoid; the lowest sensitivity was observed for HCCs with both contrast agents. Specificities ranged between 95% and 100% for both agents. It was concluded that the diagnostic value of Sonazoid is noninferior to that of SonoVue.
Results from both single study reports and meta-analyses in the peer-reviewed literature confirm the high sensitivity and specificity of SonoVue-enhanced ultrasonography for characterization of FLLs in adults; less evidence is available for Sonazoid. Sonazoid was presented as equivalent to SonoVue for the determination of FLL malignancy when combining vascular and Kupffer phase in the above reported phase III study [8, 9]. The clinical evidence also confirms that all vascular phases are relevant to assess the typical patterns of vascular enhancement. Presence and timing of washout are relevant for differentiating benign from malignant lesion; furthermore, the differentiation of early versus late washout in the vascular phase adds in assessment for CCC and HCC diagnosis [19]. No clear added value of the Kupffer phase is documented thus far for the FLL characterization as benign vs malignant or for a specific lesion type characterization.
Focal Liver Lesion Detection
After initial assessment with unenhanced ultrasound, CEUS may be added to the ultrasound examination to aid in FLL detection to monitor treatment in oncology patients, routine surveillance in patients with chronic liver diseases or cirrhosis, or in pediatric patients where radiation exposure is a concern [28,29,30]. New CEUS techniques (e.g., Cadence contrast specific imaging, Siemens, Erlangen, Germany) have also improved detection of microbubbles and extended examination duration for the late vascular phase. The development of artificial intelligence tools could be of further help, especially for young, less experienced users.
Twelve published studies were identified that focused on detection of FLLs with SonoVue-enhanced ultrasound, involving a total of 873 patients. A range of 77.5%-100% was found for sensitivity and 76.7%-97.6% for specificity in the detection of FLLs vs. CT [31,32,33,34,35,36,37,38,39,40,41,42].
The assessment conducted by the National Institute for Health and Care Excellence in 2012 also included 4 published studies comparing the performance of CEUS with SonoVue versus the performance of CECT or CEMRI for detection of liver metastases in patients with known primary cancer (colorectal cancer in most cases) [26]. There was no difference found in diagnostic performance among the 3 imaging modalities. Per-patient and per-lesion estimates of sensitivity were generally high and above 83% for all imaging modalities in all studies; in one study, sensitivity was greater than 95% for both CEUS and CECT. The data available indicate that SonoVue CEUS alone may be adequate to rule out liver metastases in people with known primary malignancies.
In a prospective Phase II clinical trial published by Correas et al., Sonazoid was used in a dose-testing analysis to determine the optimal dose for the detection of liver metastases in patients with extra-hepatic malignancy vs. contrast-enhanced computed tomography (CECT) or contrast-enhanced magnetic resonance imaging (CEMRI) [43]. The sensitivity and specificity of Sonazoid were 78% and 29%, respectively in the 41 patients who received a dose of 0.12 µL/kg, which corresponds to the approved dose of the contrast agent for liver CEUS.
CEUS with Sonazoid was compared to CEMRI and CECT for the diagnosis of hepatocellular carcinoma (HCC) in a study from Alaboudy et al. [44] Thirty-two patients undergoing surgery and intra-operative contrast-enhanced ultrasound were included. The overall diagnostic sensitivity of CEUS, CECT, and CEMRI was comparable (72%, 74%, and 86%, respectively) and no significant difference among the modalities in the diagnosis of HCC was observed (p = 0.092). When combining the different imaging modalities, the diagnostic sensitivity of CEUS + CEMRI was 90%, while addition of Sonazoid-enhanced US to CECT, and CECT to CE MRI had a sensitivity of 82 and 88%, respectively. There was no significant difference between the three imaging combinations (p = 0.970).
Kunishi et al. evaluated the detection rate of HCC using CEUS with Sonazoid according to tumor size and typical or atypical vascular pattern of the lesion [45]. Eighty-seven HCCs with a maximum diameter between 1 and 3 cm were included. The overall detection rate of CEUS with Sonazoid was 83%, whereas the detection rate for HCCs with a maximum diameter of 1–2 cm was 80%. HCCs with a typical vascular pattern showed a detection rate of 99% (67/68), whereas HCCs with atypical enhancement pattern had a detection of 26% (5/19). Fifteen of the 87 HCCs (17%) missed at CEUS with Sonazoid were isoechoic in the post-vascular phase and were regarded as not having been detected. These 15 lesions were pathologically diagnosed as well-differentiated HCC.
Goto et al. used Kupffer phase imaging (≥ 15 min post-injection) with Sonazoid for the detection of HCC vs. unenhanced ultrasound, with CECT as the reference standard [46]. The detection sensitivity for unenhanced ultrasound was 84% for reader A and 85% for reader B. Sonazoid-enhanced sensitivity was 73% for reader A and 83% for reader B. Unenhanced ultrasound specificity was 90% and 95%, respectively; for Sonazoid specificity was 99% and 98%, respectively. The authors reported that a significant proportion of false-negative nodules are hyperechoic in B-mode US, likely because echogenicity hampers visualization of the defect in Kupffer imaging. They concluded that Kupffer phase by CEUS with Sonazoid showed mediocre sensitivity for HCC detection.
HCC tumor vascularity by Sonazoid early vascular phase (10–30 s post-injection) and Kupffer phase imaging (≥ 10 min post-injection), as compared to CECT, was evaluated by Mandai et al. in 92 newly diagnosed HCC nodules in 88 patients [47]. Truth standard in this study were typical enhancement patterns in at least 2 imaging modalities or biopsy. Hyperenhancement at the early vascular phase of Sonazoid was demonstrated in 71 (77%) lesions including 66 lesions that showed high density on the arterial phase of CT. The detection of tumors at the post-vascular phase of Sonazoid was 83%, with 76 hypoenhancing lesions at CEUS, including 70 lesions that showed low density on the portal phase of CT). The investigators found that the detection rate of vascularity with Sonazoid for both the early vascular and the post-vascular phase was significantly lower for nodules located deeper than 9 cm from the abdominal wall than for nodules located within 9 cm.
The findings of contrast-enhanced intraoperative ultrasound using Sonazoid and histologic grade of hepatocellular carcinoma (HCC) were correlated by Arita et al. [48] The study comprised 374 histologically proven HCCs in 239 consecutive patients. The proportion of hypoechoic tumors during the Kupffer phase was significantly lower among well-differentiated than among moderately and poorly differentiated HCCs (54% vs 92%, p < 0.0001). Duisyenbi reported that only 58 of 84 HCCs (69%) showed a perfusion defect in the post vascular phase using low MI imaging with Sonazoid, meaning that especially well-differentiated HCCs do not wash out at Kupffer phase imaging [18]. These authors and others suggest that the low MI contrast mode used with Sonazoid does not eliminate the background B mode signal sufficiently [18, 46, 48].
A recently published multicenter trial evaluated the added value of Sonazoid CEUS when combined with conventional B-mode US as an HCC surveillance tool in patients with liver cirrhosis [49]. The study included 524 participants; 10 HCCs were confirmed in 8 participants. The detection rate of early stage HCC was not significantly improved by adding Sonazoid CEUS to conventional B-mode US (difference, 0.4% (95% confidence interval: 20.3%, 1.1%); p = 0.16). Also, the detection rate of any stage of HCC was not improved by adding Sonazoid CEUS to unenhanced US. The study confirmed that CEUS improves the characterization of FLL since the number of false positive cases, and thus the false referral rate, was reduced from 4.4% (23 of 524) with B-mode US to 1.1% (six of 524) when Sonazoid CEUS was added.
In summary, high values of sensitivity and specificity are reported with SonoVue for detection of FLLs and the assessment conducted by NICE concluded that CEUS with SonoVue alone may be adequate to rule out liver metastases in patients with known primary malignancy. Detection of metastases was only moderate with Sonazoid in one study. Sonazoid does not appear to have any additional advantage over vascular phase agents in the detection of HCC. Lack of tissue background suppression in Sonazoid CEUS may hamper visualization of wash out in the post-vascular phase, and some well-differentiated HCCs do not wash out at Kupffer phase.
CEUS-guided Interventions
Biopsy
CEUS has added value in the guidance of percutaneous lesion biopsy because the needle is more precisely targeted, avoiding avascular or hypovascular areas, increases the ease of biopsy of very small nodules, and facilitates placement of the needle to tumor-affected organ areas where involvement is irregular [50].
Studies have shown the high rate of technical success that SonoVue and Sonazoid CEUS affords for the guided biopsy of lesions [51,52,53,54]. Similar success rates close to or higher than 90% are reported for both agents, as reported in Table 2.
Monitoring of ablation procedures
Local-ablative treatment such as radiofrequency (RF) ablation and microwave ablation (MW) are effective techniques for local tumor control in patients with low burden HCC and metastases [55, 56]. CEUS enables real-time evaluation of the tumor microvasculature, making it a valuable tool for pre-treatment assessment, for immediate evaluation during the intervention, and for follow-up evaluation of treatment efficacy [57].
A study by Liu et al. demonstrated the efficiency and feasibility of SonoVue CEUS in patients with HCC who underwent MW ablation under CEUS guidance [58]. CEUS and either CECT or CEMRI follow-ups were performed at 1- and 3-month intervals for one year, then at 6-month intervals thereafter. A total of 107 patients were included in the study; 105 HCCs were successfully visualized with SonoVue CEUS and treated. A complete ablation was obtained in 104 lesions, as confirmed at 1-month follow-up. The technique effectiveness rate was therefore 99%. Another study using SonoVue for CEUS-guided MW ablation found that lesion boundaries were more extensive with CEUS over unenhanced ultrasonography, and procedural complications were higher in the unenhanced ultrasound group [59]. Tumor recurrence rates were significantly lower, and progression-free survival significantly higher in the CEUS group.
Sonazoid imaging identified 96% of HCCs in a study by Miyamoto et al. [60] MDCT performed one day following guided RF ablation indicated that complete ablation was achieved in 96% of tumors. Kupffer-phase imaging with Sonazoid was evaluated by Park et al. for lesion conspicuity and guidance of percutaneous biopsy or RF ablation of FLLs [53]. Technical success rates were 95% for biopsy and 70% for RF ablation.
SonoVue was found to be an effective immediate assessment of RF ablation of malignant liver lesions, leading to a change in therapeutic management in 59% of the cases, in a study from Wiggerman et al. [57] Patients underwent CT-guided RFA after initial examination by unenhanced ultrasound, CEUS, and CECT. CEUS was performed immediately post-RF ablation to assess ablation. Where necessary, additional ablation cycles were performed with CEUS re-evaluation. The combined CT and CEUS RF ablation procedure resulted in complete ablations for all treated lesions in a 3-month follow up. In another study by Mauri et al, intraprocedural CEUS with SonoVue detected incomplete RF ablation in 36.5% of patients [61]. At the 24-h follow-up after additional ablative cycles, complete ablation was reported in 94.6% of patients. CEUS reduced the number of re-treatments and related costs per patient.
Post-ablation follow-up is critical to patient management, and a brief list of studies presenting additional information on this subject is shown in Table 3 [62,63,64,65,66]. The accuracy values for the detection of ablation success ranged from 92 to 97%.
Key for a successful local-ablative treatment is an accurate assessment of viable tumor tissue and microvasculature, that requires CEUS imaging during the early vascular phase, and to make sure lesion margins are negative; there is no evidence that Kupffer phase imaging with a prolonged post-vascular enhancement of the liver parenchyma has any additional value. Intraoperative assessment with CEUS is key to avoid repeated ablation procedures. Multimodality fusion imaging helps to best locate the lesion and guide the ablation procedures, and fusion 3D imaging for precise determination of safe margins [67, 68].
Other potential, useful indications of CEUS are not within the scope of this review, e.g., monitoring of systemic tumor treatment in oncology patients is not discussed.
Safety
In order to investigate the safety profile of SonoVue in a clinical setting, Piscaglia et al. conducted a retrospective study in 28 Italian centers on post-marketing use in abdominal examinations [69]. A total of 23,188 examinations were included. No fatal events occurred. Adverse events (AEs) were reported in 29 cases (0.0086%); two of these were graded as serious. SonoVue AE reporting rate in this study was lower than, or similar to, reported data on radiologic and MR contrast agents. A retrospective analysis of 30,222 cases from Tang et al. in patients who had undergone SonoVue CEUS of abdominal and superficial organs at a large hospital in China between 2005 and 2014 [70]. There were no fatal cases. Six patients (0.020%) experienced AEs, 2 were considered serious (0.007%).
In the dose testing study by Correas et al. with Sonazoid in 163 patients, a total of 23 AEs (14.4%) occurred with similar frequency across all dose groups, but were slightly higher in the highest dose group (0.36 µL/kg body weight, three times the approved dose) [43]. Five of these AEs (3.0%) were considered related to the use of Sonazoid. Four of these five cases occurred in the highest dose group. All reported events were mild in intensity. In the Sonazoid Phase III trial on the identification of FLLs reported by Jiang et al. in 424 subjects, no serious AEs or deaths were reported [28]. Mild Treatment-Emergent AEs were reported in that study for 55 (13%) of subjects. In a recent publication, safety results from a phase III trial with Sonazoid in 54 patients were reported [71]. Treatment-emergent AEs were recorded for 13 (24.1%) patients. Four patients (7.4%) experienced AEs for which there was a reasonable possibility that the AE was related to the contrast agent. The most common AE was abdominal pain (9.3%), followed by heart rate irregularity (5.6%). None of the 54 patients showed serious adverse effects.
The Sonazoid shell does contains HEPS, an egg product; in patients allergic to eggs or egg products, Sonazoid should be used only when the benefit outweighs the risk [72].
Overall, both SonoVue and Sonazoid have good safety profiles for abdominal imaging.
Conclusion
The evidence assessed in this review demonstrates the importance of the vascular phases in the diagnostic algorithm for FLLs. The pure post-vascular phase that is important to Sonazoid liver imaging begins at about 10 min and can extend to an hour or more [1]. This may potentially allow the assessment of wash out related findings during the late phase for a longer period of time, when compared to a blood pool agent. However, the post-vascular phase may not be practical for the work flow in a busy practice. It should be also considered that some benign lesions do not have Kupffer cells and may result as false positive findings at the post-vascular phase [73, 74]. It has also been reported that well differentiated hypervascular HCCs are more difficult to detect during the post-vascular phase [18, 46, 48].
CEUS has a proven high diagnostic accuracy in the characterization and detection of FLL in the non-cirrhotic liver, comparable to CT and MRI. For surveillance of patients with liver cirrhosis the detection of HCC is a crucial requirement. However, due to the short duration of arterial phase hyperenhancement of HCC adequate assessment of the whole liver is considered to be impossible, and the CEUS WFUMB guidelines do not recommend routine use of CEUS for the surveillance of patients at risk for HCC [75].
The bulk of the published data comes from the purely vascular agent SonoVue. Due to the limited published reports with Sonazoid, further studies might be needed with this agent to accurately correlate enhancement patterns and diagnostic accuracy.
CEUS is generally useful in various treatment monitoring indications for the guided biopsy and ablation procedure for pre-treatment, intraoperative and post-treatment assessment. CEUS is particularly beneficial for the immediate treatment evaluation during the intervention. Since the key information for guidance of interventional procedures is obtained during the early vascular phase, an additional benefit of the prolonged examination time by Kupffer phase imaging has not yet been identified.
References
Claudon M, Dietrich CF, Choi BL, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver – update 2012. Ultraschall Med 2013;34(1):11-29.
Ferraioli G, Meloni MF. Contrast-enhanced ultrasonography of the liver using SonoVue. Ultrasonography. 2018; 37(1):25-35.
Tarantino L, Ambrosino P, Di Minno MND. Contrast-enhanced ultrasound in differentiating malignant from benign portal vein thrombosis in hepatocellular carcinoma. World J Gastroenterol. 2015; 21(32):9457-9460.
Bracco Sine Pharmaceutical Corp Safety Update Report for SonoVue (China) 01 January 2009 to 31 December 2015.
Bracco Imaging S.p.A. Periodic Safety Update Report 01 October 2017 to 30 September 2018
Bracco Diagnostics Inc. Internal sales data.
Information Medical Statistics Health data accessed 17 May 2019.
Zhai H-Y, Liang P, Yu J, et al. Comparison of Sonazoid and Sonovue in the diagnosis of focal liver lesions. J Ultrasound Med 2019 Jan 25 EPub.
Jiang Y, Lv K, Liang P, et al. A Phase 3 Multicentre, Randomised, Comparative study of the efficacy and safety of Sonazoid and SonoVue in subjects with focal liver lesions undergoing pre- and post-contrast ultrasound imaging. Ultrasound Med Biol. 2017;43 Suppl 1 S34-S35.
Lumason [SonoVue] (sulfur hexafluoride lipid-type A microspheres) for injectable suspension, for intravenous use. Full Prescribing Information. December 2016.
GE Healthcare brochure: Sonazoid, Innovatively long-lasting microbubbles enabling confident diagnosis with Kupffer image. 2013
Morel DR, Schwieger I, Hohn L, et al. Human pharmacokinetics and safety evaluation of SonoVue, a new contrast agent for ultrasound imaging. Invest Radiol. 2000;35(1) 80-85.
Li P, Hoppmann S, Du P, et al. Pharmacokinetics of perfluorobutane after intra-venous bolus injection of Sonazoid in healthy Chinese volunteers. Ultrasound Med Biol. 2017;43(5) 1031-1039.
Yanagisawa K, Moriyasu F, Miyahara T, et al. Phagocytosis of ultrasound contrast agent microbubbles by Kupffer cells. Ultrasound Med Biol. 2007;33(2):318-325.
Dixon LJ, Barnes M, Tang H, et al. Kupffer cells in the liver. Compr Physiol. 2013;3(2):785-797.
Shunichi S, Hiroko I, Fuminori M, et al. Definition of contrast enhancement phases of the liver using a perfluoro-based microbubble agent, perflubutane microbubbles. Ultrasound Med Biol. 2009;35(11) 1819-1827.
Nihonmatsu H, Numata K, Fukuda H, et al. Low mechanical index contrast mode versus high mechanical index contrast mode: which is a more sensitive method for detecting Sonazoid microbubbles in the liver of normal subjects? J Med Ultrasonics. 2016;43(2):211-217
Duisyenbi Z, Numata K, Nihonmatsu H, et al. Comparison between low mechanical index and high mechanical index contrast modes of contrast-enhanced ultrasonography: evaluation of perfusion defects of hypervascular hepatocellular carcinomas during the post–vascular phase. J Ultrasound Med. 2019 Jan 17 EPub.
American College of Radiology https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/LI-RADS/CEUS-LI-RADS-v2017 accessed 03 July 2019.
Lyshchik A, Kono Y, Dietrich CF, et al. Contrast-enhanced ultrasound of the liver: technical and lexicon recommendations from the ACR CEUS LI-RADS working group. Abdom Radiol. 2018; 43(4):861-879.
Xie D-Y, Ren Z-G, Zhou J, et al. Critical appraisal of Chinese 2017 guideline on the management of hepatocellular carcinoma. HepatoBiliary Surg Nutr. 2017;6(6):387-396.
Nolsøe CP, Nolsøe AB, Klubien J, et al. Use of ultrasound contrast agents in relation to percutaneous interventional procedures a systematic review and pictorial essay. J Ultrasound Med. 2018;37(6):1305-1324.
Friedrich-Rust M, Klopffleisch T, Nierhoff J, et al. Contrast-Enhanced Ultrasound for the differentiation of benign and malignant focal liver lesions: a meta-analysis. Liver Int. 2013;33(5):739-755.
Niu Y, Huang T, Lian F, et al. Contrast-enhanced ultrasonography for the diagnosis of small hepatocellular carcinoma: a meta-analysis and meta-regression analysis. Tumor Biol. 2013;34(6):3667-3674.
Guang Y, Xie L, Ding H et al. Diagnosis value of focal liver lesions with SonoVue-enhanced ultrasound compared with contrast-enhanced computed tomography and contrast-enhanced MRI: a meta-analysis. J Cancer Res Clin Oncol.2011;137(11):1595-1605.
NICE Diagnostics guidance: SonoVue (sulphur hexafluoride microbubbles) – contrast agent for contrast-enhanced ultrasound imaging of the liver29 August 2012. https://www.nice.org.uk/guidance/dg5. Accessed 03 July 2019.
Westwood M, Joore M, Grutters J, et al. Contrast-enhanced ultrasound using SonoVue® (sulphur hexafluoride microbubbles) compared with contrast-enhanced computed tomography and contrast-enhanced magnetic resonance imaging for the characterisation of focal liver lesions and detection of liver metastases: a systematic review and cost-effectiveness analysis. Health Technol Assessment. 2013;17(16):1-243.
D’Onofrio M, Crosara S, De Robertis R, et al. Contrast-enhanced ultrasound of focal liver lesions. Am J Roentgenol. 2015;205(1):W56-W66.
Shiozawa K, Watanabe M, Kikuchi Y, et al. Evaluation of sorafenib for hepatocellular carcinoma by contrast-enhanced ultrasonography: A pilot study. World J Gastroenterol. 2012;18(40):5753-5758.
Sidhu PS, Cantisani V, Dietrich CF, et al. The EFSUMB guidelines and recommendations for the clinical practice of contrast-enhanced ultrasound (CEUS) in non-hepatic applications: update 2017 (long version). Ultraschall in Med. 2018;39(2):e2-e44.
Oldenburg A, Hohmann J, Foert E, et al. Detection of hepatic metastases with low MI real time contrast enhanced sonography and SonoVue. Ultraschall Med. 2005;26(4):277-284.
Bartolotta TV, Taibbi A, Picone D, et al. Detection of liver metastases in cancer patients with geographic fatty infiltration of the liver: the added value of contrast-enhanced sonography. Ultrasonography. 2017;36(2):160-169.
Hoeffel C, Job L, Ladam-Marcus V, et al. Detection of hepatic metastases from carcinoid tumor: prospective evaluation of contrast-enhanced ultrasonography. Dig Dis Sci. 2009;54(9):2040-2046.
Huf S, Platz Batista da Silva N, Wiesinger I, et al. Analysis of Liver Tumors Using Preoperative and Intraoperative Contrast-Enhanced Ultrasound (CEUS/IOCEUS) by Radiologists in Comparison to Magnetic Resonance Imaging and Histopathology. Rofo. 2017;189(5):431-440.
Janica JR, Lebkowska U, Ustymowicz A, et al. Contrast-enhanced ultrasonography in diagnosing liver metastases. Med Sci Monit. 2007;13 Suppl 1:111-115.
Konopke R, Kersting S, Bergert H, et al. Contrast-enhanced ultrasonography to detect liver metastases: a prospective trial to compare transcutaneous unenhanced and contrast-enhanced ultrasonography in patients undergoing laparotomy. Int J Colorectal Dis. 2007;22(2):201-207.
Konopke R1, Bunk A, Kersting S. Contrast-enhanced ultrasonography in patients with colorectal liver metastases after chemotherapy. Ultraschall Med. 2008;29 Suppl 4:S203-209.
Piscaglia F, Corradi F, Mancini M, et al. Real time contrast enhanced ultrasonography in detection of liver metastases from gastrointestinal cancer. BMC Cancer. 2007;7:171.
Quaia E, D’Onofrio M, Palumbo A et al. Comparison of contrast-enhanced ultrasonography versus baseline ultrasound and contrast-enhanced computed tomography in metastatic disease of the liver: diagnostic performance and confidence. Eur Radiol. 2006;16(7):1599-1609.
Cantisani V, Ricci P, Erturk M, et al. Detection of hepatic metastases from colorectal cancer: prospective evaluation of gray scale US versus SonoVue® low mechanical index real time-enhanced US as compared with multidetector-CT or Gd-BOPTA-MRI. Ultraschall in Med 2010;31(5):500-505.
Rafaelsen SR, Jakobsen A. Detection of hepatic metastases from colorectal cancer: prospective evaluation of gray scale US versus SonoVue® low mechanical index real time-enhanced US as compared with multidetector-CT or Gd-BOPTA-MRI. Colorectal Dis. 2011;13(4):420-425.
Dietrich CF, Kratzer W, Strobel D, et al. Assessment of metastatic liver disease in patients with primary extrahepatic tumors by contrast-enhanced sonography versus CT and MRI. World J Gastroenterol. 2006;12(11):1699-1705.
Correas J-M, Low G, Needleman L, et al. Contrast enhanced ultrasound in the detection of liver metastases: a prospective multi-centre dose testing study using a perfluorobutane microbubble contrast agent (NC100100). Eur Radiol. 2011;21(8):1739-1746.
Alaboudy A, Inoue T, Hatanaka K, et al. Usefulness of combination of imaging modalities in the diagnosis of hepatocellular carcinoma using Sonazoid -enhanced ultrasound, gadolinium diethylene-triamine-pentaacetic acid-enhanced magnetic resonance imaging, and contrast-enhanced computed tomography. Oncology. 2011;81 (Suppl 1):66-72.
Kunishi Y, Numata K, Morimoto M, et al. Efficacy of fusion imaging combining sonography and hepatobiliary phase MRI with Gd-EOB-DTPA to detect small hepatocellular carcinoma. Am J Roentgenol. 2012;198(1):106-114.
Goto E, Masuzaki R, Tateishi R, et al. Value of post-vascular phase (Kupffer imaging) by contrast-enhanced ultrasonography using Sonazoid in the detection of hepatocellular carcinoma. J Gastroenterol. 2012;47(4):477-485.
Mandai M, Koda M, Matono T, et al. Assessment of hepatocellular carcinoma by contrast-enhanced ultrasound with perfluorobutane microbubbles: comparison with dynamic CT. Br J Radiol. 2011;84(1002):499-507.
Arita J, Hasegawa K, Takahashi M, et al. Correlation between contrast- enhanced intraoperative ultrasound using Sonazoid and histologic grade of resected hepatocellular carcinoma. Am J Roentgenol. 2011;196(6):1314-1321.
Park JH, Park M-S, Lee SJ, et al. Contrast-enhanced US with perfluorobutane for hepatocellular carcinoma surveillance: a multicenter diagnostic trial (SCAN). Radiology. 2019;292(3): 638-646.
Spârchez Z, Radu P, Zaharia T, et al. Contrast enhanced ultrasound guidance: a new tool to improve accuracy in percutaneous biopsies. Med Ultrason. 2010;12(2):133-138.
Spârchez Z, Radu P, Kacso G, et al. Prospective comparison between real time contrast enhanced and conventional ultrasound guidance in percutaneous biopsies of liver tumors. Med Ultrason. 2015;17(4):456-463.
Eso Y, Takai A, Takeda H, et al. Sonazoid-enhanced ultrasonography guidance improves the quality of pathological diagnosis in the biopsy of focal hepatic lesions. Eur J Gastroenterol Hepatol. 2016;28(12):1462–1467.
Park HS, Kim YJ, Yu MH, et al. Real-time Contrast-enhanced sonographically guided biopsy or radiofrequency ablation of focal liver lesions using perflurobutane microbubbles (Sonazoid). J Ultrasound Med. 2015;34(3) 411-421.
Kang TW, Lee MW, Song KD, et al. Added value of contrast-enhanced ultrasound on biopsies of focal hepatic lesions invisible on fusion imaging guidance. Korean J Radiol. 2017;18(1):152-161.
McDermott S, Gervais DA. Radiofrequency ablation of liver tumors. Semin Intervent Radiol. 2013;30(1):49–55.
Brace CL. Radiofrequency and microwave ablation of the liver, lung, kidney and bone: What are the differences: “Organ-specific thermal ablation”. Curr Probl Diagn Radiol. 2009;38(3):135-143.
Wiggerman P, Zuber-Jerger I, Zausig Y, et al. Contrast-enhanced ultrasound improves real-time imaging of ablation region during radiofrequency ablation: preliminary results. Clin Hemorheol Microcirc. 2011;49(1-4):43-54.
Liu F, Yu X, Liang P, et al. Contrast-enhanced ultrasound-guided microwave ablation for hepatocellular carcinoma inconspicuous on conventional ultrasound. Int J Hyperthermia. 2011;27(6):555-562.
Yan S-Y, Zhang Y, Sun C, et al. Comparison of real-time contrast-enhanced ultrasonography and standard ultrasonography in liver cancer microwave ablation. Exper Therapeutic Med. 2016;12(3):1345-1348.
Miyamoto N, Hiramatsu K, Tsuchiya K, et al. Sonazoid-enhanced sonography for guiding radiofrequency ablation for hepatocellular carcinoma: better tumor visualization by Kupffer-phase imaging and vascular-phase imaging after reinjection. Japan J Radiol.2009:27(4):185-193.
Mauri G, Porazzi E, Cova L, et al. Intraprocedural contrast-enhanced ultrasound (CEUS) in liver percutaneous radiofrequency ablation: clinical impact and health technology assessment. Insights Imaging. 2014;5(2):209-216.
Du J, Li H-L, Zhai B, et al. Radiofrequency ablation for hepatocellular carcinoma: utility of conventional ultrasound and contrast-enhanced ultrasound in guiding and assessing early therapeutic response and short-term follow-up results. Ultrasound Med Biol. 2015;41(9):2400-2411.
Luo W, Numata K, Morimoto M, et al. Role of Sonazoid-enhanced three-dimensional ultrasonography in the evaluation of percutaneous radiofrequency ablation of hepatocellular carcinoma. Eur J Radiol. 2010;75(1):91-97.
Zheng S-G, Xu H-X, Lu M-D, et al. Role of contrast-enhanced ultrasound in follow-up assessment after ablation for hepatocellular carcinoma. World J Gastroenterol. 2013;19(6):855-865.
Bo X-W, Xu H-X, Sun L-P, et al. Bipolar radiofrequency ablation for liver tumors: comparison of contrast-enhanced ultrasound with contrast-enhanced MRI/CT in the posttreatment imaging evaluation. Int J Clin Exp Pathol 2014;7(9):6108-6116.
Frieser M, Kiesel J, Lindner A, et al. Efficacy of contrast-enhanced US versus CT or MRI for the therapeutic control of percutaneous radiofrequency ablation in the case of hepatic malignancies. Ultraschall in Med. 2011;32(2):148-153.
Bo X-W, Xu H-X, Guo L-H, et al. Ablative safety margin depicted by fusion imaging with post-treatment contrast-enhanced ultrasound and pretreatment CECT/CEMRI after radiofrequency ablation for liver cancers. Br J Radiol. 2017;90:20170063.
Xu E-J, Lv S-M, Li K, et al. Immediate evaluation and guidance of liver cancer thermal ablation by three-dimensional ultrasound/contrast-enhanced ultrasound fusion imaging. Int J Hypertherm. 2017;34(6)870-876.
Piscaglia F, Bolondi L, et al. The Safety of SonoVue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol. 2006;32(9):1369-1375.
Tang C, Fang K, Guo Y, et al. Safety of sulfur hexafluoride microbubbles in sonography of abdominal and superficial organs: Retrospective analysis of 30,222 cases. J Ultrasound Med. 2017;36(3):531-538.
Chou YH, Liang JD, Wang SY, Hsu SJ, Hu JT, Yang SS, et al. Safety of perfluorobutane (Sonazoid) in characterizing focal liver lesions. J Med Ultrasound 2019;27:81-5.
Sonazoid (Perfluorobutane) Microspheres for Injection. Prescribing Information. GE Healthcare Co., Ltd. Shanghai, China. July 31, 2018.
Ishibashi H, Maruyama H, Takahashi M, et al. Demonstration of intrahepatic accumulated microbubble on ultrasound represents the grade of hepatic fibrosis. Eur Radiol. 2012;22(5):1093-1090.
Lizardi-Cervera J, Cuéllar-Gamboa L, Motola-Kuba D. Focal nodular hyperplasia and hepatic adenoma: a review. Annals Hepatol. 2006;5(3):206-211.
Deitrich CF, N.C., Barr RG et. al., Guidelines and Good Clinical Practice Recommendations for Contrast Enhanced Ultrasound (CEUS) in the Liver – Update 2020. WFUMB in Cooperation with EFSUMB, AFSUMB, AIUM, and FLAUS. Ultrasound in Medicine and Biology, 2020 (in Press)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
RGB has the following COI: research grants from Philips Ultrasound, Siemens Ultrasound, Mindray, GE Ultrasound, SuperSonic Imagine, B and K Ultrasound. He is on the speaker’s bureau of Philips Ultrasound, Mindray, Siemens Ultrasound, and Bracco Diagnostics. He is on the advisory board of Bracco Diagnostics and Lantheus Medical. He receives royalties from Thieme Publishers. RZ—research grants from Philips Ultrasound and Mindray. She is on the speaker’s bureau of Mindray, Esaote, Sonoscape, Philips Ultrasound and Bracco Diagnostics. PH, YanL, XX, KY, XJ, YukunL, HX, JML declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Bracco Imaging S.p.A sponsored the meeting of the authors but had no influence on the content of this manuscript.
Rights and permissions
About this article
Cite this article
Barr, R.G., Huang, P., Luo, Y. et al. Contrast-enhanced ultrasound imaging of the liver: a review of the clinical evidence for SonoVue and Sonazoid. Abdom Radiol 45, 3779–3788 (2020). https://doi.org/10.1007/s00261-020-02573-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02573-9