Abstract
Objective
To compare the ability of MR elastography (MRE) with transient elastography (TE) and intravoxel incoherent motion (IVIM) diffusion-weighted MRI in staging hepatic fibrosis (HF).
Materials and methods
100 patients with chronic liver disease and 25 healthy volunteers underwent preoperative MRE, IVIM on a 3T MRI unit, and ultrasound-based TE. Liver stiffness measurement from MRE (LSM-MRE) and liver stiffness measurement from TE (LSM-TE) were measured; four diffusion parameters including the true diffusion coefficient (Dt), pseudo-diffusion coefficient, perfusion fraction (f), and apparent diffusion coefficient (ADC) were calculated. Receiver operating characteristic (ROC) curves were performed for significant parameters to compare the diagnosis performance for detecting HF.
Results
LSM-MRE and LSM-TE values showed positive correlation with the fibrosis stage (r = 0.910 and 0.813, P < 0.001). Dt, f, and ADC values showed negative correlation with the fibrosis stage (r = − 0.727, − 0.503, and − 0.601, all P < 0.001). The area under the ROC curve (AUC) of LSM-MRE (AUC = 0.965, 0.957, 0.983) was significantly higher than that of LSM-TE (AUC = 0.906, 0.913, 0.931) and Dt (AUC = 0.875, 0.879, 0.861) in discriminating significant HF (≥ F2), advanced HF (≥ F3), or cirrhosis (F4) (all P < 0.05). Although LSM-TE showed higher AUCs than Dt in detecting fibrosis stages, there were no significant differences between LSM-TE and Dt (P > 0.05) except for detecting F4 (P < 0.05).
Conclusion
MRE shows excellent diagnostic performance for predicting significant fibrosis, advanced fibrosis compared with TE and IVIM, while TE and IVIM have comparable diagnostic performance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hepatic fibrosis (HF) is a wound-healing response to various categories of chronic liver diseases [1]. The early stage of HF is potentially reversible after treatment [2,3,4]. However, the progression of untreated HF may eventually lead to hepatic cirrhosis, portal hypertension, and even hepatocellular carcinoma (HCC) which are accountable for a high rate of morbidity and mortality as well as increased resource costs [1, 4, 5]. To date, invasive liver biopsy is the reference standard for diagnosis and staging HF. However, this technique has some limitations such as invasiveness, risks of complications, observation variations, sampling error, and poor patient tolerance [6], making it poorly suitable for dynamically monitoring patients with chronic liver diseases. Therefore, reliable and non-invasive tools are essential for early detecting and staging of HF.
Recently, there are several non-invasive and potential imaging techniques for the assessment of HF, including magnetic resonance elastography (MRE), intravoxel incoherent motion diffusion-weighted MRI (IVIM DW-MRI), and ultrasound-based transient elastography (TE). MRE has been increasingly adopted for HF evaluation in patients with chronic liver diseases [1, 3, 7,8,9,10,11,12,13,14,15,16]. As shown in some studies, the stiffness and elasticity of the liver tissue may alter along with the degree of HF, impacts of chronic hepatitis before HF, and increased portal venous pressure [12,13,14,15,16]. Moreover, liver stiffness measurement with MRE (LSM-MRE) has been used for evaluating HF in clinical practice and has received significant attention.
Intravoxel incoherent motion (IVIM), a biexponential model of DWI which was introduced by Le Bihan et al. [17], would allow separate assessment of microcirculation in the capillaries and water-molecule diffusion. Currently, IVIM with multiple b-values has become a topic of interest in the assessment HF. Several prior studies have reported that IVIM parameters could show potential ability in diagnosing HF and may provide more accurate information concerning true water molecules diffusion and incoherent motion of water molecules in the capillary network [4, 18,19,20,21,22,23].
Transient elastography (TE) is also a non-invasive method by measuring liver stiffness to evaluate HF [24,25,26]. As we all know, this technique has the following advantages: simplicity, low cost, short performance time, high patient reception, and so forth. So far, the results of prior studies suggest that liver stiffness measurement with TE (LSM-TE) has a promising application prospect for evaluation of HF in clinical practice [24,25,26,27,28,29,30,31].
To date, although some studies have reported MRE, TE, and IVIM in the assessment of HF [1, 16, 32,33,34], there is a lack of comprehensive comparison among them. Given this background, the goal of this study was to quantitatively compare the ability among LSM-MRE, LSM-TE, and IVIM parameters in evaluating HF in the same individuals.
Materials and methods
Subjects
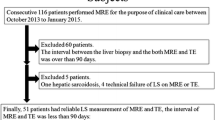
This prospective study was approved by our institutional review board. Informed consent in written was obtained from every subject prior to participation. Between May 2014 and January 2017, a total of 108 patients with chronic liver diseases were recruited consecutively for the study. All patients had undergone liver MRI (including MRE, IVIM-DWI) and TE. The inclusion criteria for patients with chronic liver diseases were as follows: no previous antiviral therapy; without a large amount of ascites; all subjects were confirmed by liver biopsy or liver resection; liver MRI and TE were performed within one month before liver biopsy or liver resection; acceptable image quality. Of these 108 patients, 6 were excluded from the study due to lack of histopathological results (n = 2) and poor images with artifacts (n = 4). In addition, 2 were excluded from the study on account of high iron content in liver. Finally, 100 patients (64 males and 36 females; mean age: 37.6 ± 9.3 years, age range: 22–58 years) were included in our study (Fig. 1, Table 1). Among the 100 patients, 81 were with hepatitis B, 8 with hepatitis C, 3 with non-alcoholic fatty liver disease, 2 with drug-induced hepatitis, and 6 with autoimmune hepatitis (Table 1).
Flowchart of the study enrolment population. The 25 healthy volunteers without ultrasound-guided liver biopsy and with no history or of evidence alcohol abuse, chronic liver disease, focal liver lesions, or liver dysfunction were assumed to have fibrosis stage F0 and inflammatory activity grade A0 in this study. *F0/A0 group includes 1 patient with pathologically proved F0/A0 and 25 volunteers who were regarded to have healthy livers
In the meantime, 25 healthy volunteers (7 males and 18 females, mean age: 31.5 ± 12.9 years, age range: 21–69 years) were recruited consecutively for the study (Fig. 1, Table 1). All the healthy subjects with no ultrasound-guided liver biopsy had undergone MRE, IVIM-DWI, and TE. The inclusion criteria for the healthy volunteers were no history of alcohol abuse; without chronic liver disease or focal liver lesions; without abnormal liver function test results; and acceptable image quality.
MR elastography
All the participants underwent liver MR examination on a 3-T MR imaging unit (Discovery MR 750; GE Medical Systems, Milwaukee, WI) using an 8-channel phased-array coil and fasted for at least 6 h before the examination. An active pneumatic driver was located outside the imaging room and produced 60-Hz mechanical vibrations. The active driver was connected with a passive driver through a plastic tube to deliver the vibrations to the right upper abdomen. As the patient stayed in the supine position, the passive driver was attached to the right chest wall via a rubber belt and the center of the driver was to be located at the xiphisternum level. Image acquisition of MRE was performed with a two-dimensional spin-echo echo-planar imaging (SE-EPI) sequence and the imaging parameters were as follows: TR/TE, 600/58 ms; flip angle, 30°; matrix, 256 × 128; bandwidth, 250 Hz/pixel; imaging frequency, 64 MHz; field of view, 42 × 42 cm; parallel imaging acceleration factor, 2; section thickness/ intersection gap, 10/0 mm; slice number, 3; number of excitations, 2; and acquisition time, 19 s. Three slices were acquired at the widest part of the liver. The liver stiffness maps were generated by processing the acquired propagating shear wave image through an inversion algorithm [1, 12]. For each participant, two radiologists independently measured the liver stiffness (LSM-MRE) values by placing ROIs in the right lobe of the liver on the stiffness maps. As a rule, each ROI was at least 150 mm2 and was positioned away from blood vessels, marginal liver tissues, poor shear wave amplitude, and multi-path wave interference. LSM-MRE value was expressed in kilopascals (kPa).
Transient elastography
LSM-TE was obtained by using ultrasound-based transient elastography (FibroScan; Echosens, Paris, France) in the light of the manufacturer’s recommendations, with the patient in the supine position. The tip of the transducer probe was daubed with coupling gel and located on the skin over the ribs above the right lobe of the liver. Ten successful acquisitions were accomplished on each patient by a trained operator. The median LSM-TE value was then calculated by the device and regarded as representative of the elastic modulus of liver for that patient [25]. The LSM-TE values were expressed in kilopascals (kPa). As per the manufacturer’s recommendations, a success rate of at least 60% and TE procedures with 10 valid measurements were thought to be reliable and could be retained [30].
IVIM-DWI
IVIM-DWI was performed with respiratory-triggered fat-saturated spin-echo echo-planar sequence in the transverse plane. The imaging parameters of IVIM-DWI with multiple b-values were as follows: TR/TE, 9230 ms/minimum; field of view, 36 × 38 cm; matrix, 128 × 128; slice thickness, 5 mm; intersection gap, 1 mm; parallel imaging reduction factor, 2; and acquisition time, approximately 10 min (variable depending on a patient’s respiratory cycle). Thirteen different b-values were used: 0, 50, 100, 150, 200, 300, 500, 800, 1000, 1300, 1500, 1700, and 2000 s/mm2. Motion proving gradient pulses were simultaneously used in three directions.
Three diffusion parameters are obtained from IVIM-DWI including the pseudo-diffusion coefficient which would reflect capillary perfusion (Dp; × 10−3mm2/s), the true diffusion coefficient which would reflect true molecular diffusion (Dt; × 10−3mm2/s), and the perfusion fraction (f; %) which characterizes the segmental volume occupied in the voxel via flowing spins. These parameter values were calculated with the biexponential IVIM model equation introduced by Le Bihan et al [18]:
where S(b) characterizes the signal intensity in the presence of diffusion sensitization, S(0) characterizes the signal intensity in the absence of diffusion sensitization, and b characterizes the diffusion sensitizing factor. The ADC value which represents an apparent diffusion coefficient was calculated from all the 13 b-values with a monoexponential model as follows [18]:
To obtain the diffusion parameters, IVIM images were transferred to a workstation (Advantage Workstation 4.6, GE Medical Systems) for processing. They were independently processed and analyzed by two radiologists with 9 and 11 years of experience in abdominal MR imaging who were blinded to the histopathologic results. The two radiologists independently placed three regions of interest (ROIs) in the right lobe of the liver on the images with b = 0 s/mm2. The ROI was automatically copied by software to each image (b = 50–2000 s/mm2) and the mean signal intensities within the ROIs were calculated for each image. Dt, Dp, f, and ADC values were calculated using the average signal intensities in each ROI. The areas of the ROIs varied from 150 to 200 mm2, and each ROI was avoiding bile ducts and large vessels to ensure accurate measurements.
Histopathological analysis
In the work, the liver biopsy was obtained by ultrasound-guided 18-gauge core liver biopsy from the right lobe of the liver in 94 patients. In addition, the liver specimens were obtained during liver resection for hepatocellular carcinoma (HCC) in 6 patients and the distance of specimens with tumor was 1–2 cm. Histopathology of the biopsy specimens and hepatic parenchyma in surgically resected livers were analyzed independently by two hepatopathologists with 8 and 17 years of experience. The hepatopathologists were blinded to all the patients’ imaging data and provided scores in consensus by using the METAVIR system [35]. The fibrosis was staged as follows: F0 = no fibrosis, F1 = portal fibrosis without septa, F2 = portal fibrosis and few septa, F3 = numerous septa without cirrhosis, and F4 = cirrhosis. The inflammatory activity was graded as follows: A0 = no activity, A1 = mild activity, A2 = moderate activity, and A3 = severe activity.
Statistical analysis
The mean and standard deviation (SD) of each parameter (LSM-MRE, LSM-TE, Dt, Dp, f, and ADC) were calculated for each fibrosis group. The Kruskal–Wallis test was employed for comparison of each parameter among the fibrosis groups. Spearman rank correlation was used to assess the correlation of each parameter with fibrosis stages. ROC curves were obtained for all parameters to evaluate the AUC and to determine which parameter was optimal for detecting fibrosis stages. All analyses were performed using statistical software (version 17.0; SPSS, Chicago, IL and version 12; MedCalc Software, Mariakerke, Belgium). The results with P values less than 0.05 were considered significantly different. The inter-observer agreement for the two independent measurements was assessed by calculating the intraclass correlation coefficient.
Results
Fibrosis staging and inflammatory activity grading
Histological quantification of HF was performed in 94 patients by liver biopsy and 6 patients by surgical hepatic resection. The 25 volunteers with healthy livers were regarded to have fibrosis stage 0 and inflammatory activity grade 0. Finally, the fibrosis stage distribution is as follows: F0, n = 26; F1, n = 17; F2, n = 33; F3, n = 25; and F4, n = 24. The inflammatory activity grade distribution is as follows: A0, n = 26; A1, n = 20; A2, n = 56; and A3, n = 23 (Fig. 1, Table 1).
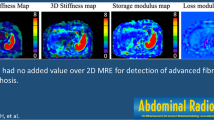
Figure 2 shows MRE, DWI (b = 0 s/mm2) images and ADC, Dt, Dp, as well as f maps for a patient with fibrosis stage 3 and inflammatory activity grade 2.
Relationships between fibrosis stage and all parameters
All parameters except Dp were significantly different among the groups F0, F1, F2, F3, and F4 (all P < 0.001). All parameters data in each fibrosis group are summarized in Table 2.
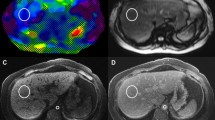
There was a strongly positive correlation between LSM-MRE and fibrosis stage (r = 0.910, P < 0.0001), and between LSM-TE and fibrosis stage (r = 0.813, P < 0.0001) (Table 2). LSM-MRE and LSM-TE values increased with the fibrosis stage progressing (all P < 0.0001) (Fig. 3a, b). In addition, there was a strongly negative correlation between Dt and fibrosis stage (r = − 0.727, P < 0.001), a moderately negative correlation between f and fibrosis stage and between ADC and fibrosis stage (r = −0.503 and r = − 0.601, all P < 0.001) (Table 2). Nevertheless, no significant correlation was observed between Dp and fibrosis stage (r = − 0.121, P > 0.05) (Table 2). All diffusion parameters except Dp decreased with the fibrosis stage progressing (all P < 0.001) (Fig. 3c–f).
Box plots of a liver stiffness value from MRE (LSM-MRE), b liver stiffness value from TE (LSM-TE), cDt, dDp, e f, and f ADC values for fibrosis stage groups F0, F1, F2, F3, and F4. LSM-MRE, LSM-TE, Dt, f and ADC values were significantly different among the above groups (all P < 0.001). However, Dp values did not show significant differences (P > 0.05). Line in each box characterizes the median, and the horizontal boundaries of the boxes characterize the first and third quartiles
Diagnostic performance of MRE, TE, and IVIM-DWI
Table 3 shows the AUCs, sensitivity, and specificity of LSM-MRE, LSM-TE, Dt, f, and ADC at their optimal cut-off values in detecting fibrosis stage ≥ F1, stage ≥ F2, stage ≥ F3, and stage F4. For the evaluation of fibrosis stages (≥ F1/ ≥ F2/ ≥ F3/F4), LSM-MRE showed the higher diagnostic value than LSM-TE, Dt (all P < 0.05), with an exception that LSM-MRE and LSM-TE showed a comparable diagnostic performance in detecting stage ≥ F1 (Table 4). For the evaluation of fibrosis stages, although LSM-TE showed the higher AUCs, there were no significant differences between LSM-TE and Dt (P > 0.05) except in detecting stage F4 (P < 0.05) (Table 4).
The overall mean intraclass correlation coefficient of LSM-MRE between the two independent radiologists was 0.936 (P < 0.001). The overall mean interclass correlation coefficient of IVIM parameters between the two independent radiologists was 0.874 (P < 0.001).
Discussion
In the study, we observed a significantly positive correlation between HF stage and LSM-MRE and LSM-TE, and a significantly negative correlation between HF stage and IVIM parameters with the exception of Dp. We also observed that MRE showed the highest diagnostic performance compared to TE and IVIM for discriminating fibrosis stage ≥ F2, ≥ F3 , and F4. Nevertheless, TE and IVIM had similar diagnostic performance for discriminating fibrosis stage ≥ F1, ≥ F2 , and ≥ F3.
Several prior studies [13, 14, 16, 25, 26, 29] have reported that MRE and TE showed significantly correlation with the HF stage and that the liver stiffness values increased as HF stage progressed. Our study had the similar results agreed with these prior studies. Furthermore, some studies [16, 23] have reported that Dp values from IVIM model showed negative correlation with the HF stage and the corresponding parameter values reduced as HF stage increased. Interestingly, the Dp values showed no significant correlation with the HF stage in this study; nevertheless, Dt showed a negative correlation. We considered that the discrepancies between the results of this study and the previous studies were caused by the following reasons: First, in this study, very low b-values (0 < b < 50 s/mm2) were not selected, which may result in underestimation of Dp; second, the instability and the large SD of Dp values might influence the findings. As prior studies have reported, the Dp values obtained from the IVIM model are unstable and may have low repeatability [16, 36]; third, the sample size in each stage was different and the study populations varied.
Previous studies [1, 23, 37] have indicated that patients with significant fibrosis (≥ F2) have a higher risk of developing cirrhosis in the future and need treatment; patients with advanced fibrosis (≥ F3) or cirrhosis should be screened for portal hypertension and HCC. Hence, accurate diagnosis of HF stage is very meaningful. In the study, LSM-MRE showed high diagnostic capability in detecting stage ≥ F1, ≥ F2, ≥ F3 , and F4 with cut-off values of 3.16, 3.57, 4.41, and 5.1 kPa, representing a combination of high sensitivity (86.9%, 89.0%, 87.8%, and 100%) and specificity (96.2%, 97.7%, 92.1%, and 90.1%). In comparison, Wang et al. [1] reported sensitivity of 72%, 91%, 92%, and 95% and specificity of 100%, 97%, 95%, and 87% with relatively higher cut-off values of 5.02, 5.37, 5.97, and 5.97 kPa. Venkatesh et al. [8] reported sensitivity of 96.08%, 97.4%, 100%, and 100% and specificity of 91.7%, 100%, 94.1%, and 95.2% with relatively lower cut-off values of 2.74, 3.2, 3.7, and 4.33 kPa. The current study and previous studies [1, 7,8,9,10, 12, 13] all showed that MRE could provide similarly excellent diagnostic performance for staging HF, whereas they showed variety of cut-off values which may be explained by the differences of the sample size and the etiology of study population, imaging protocols, and post processing procedures [1].
In the study, TE showed high diagnostic performance for detecting fibrosis stages, which was similar to previous studies [31, 32, 38]. However, the cut-off values of LSM-TE in detecting stage ≥ F3 and F4 (7.85 and 10.45 kPa) in this study are relatively lower than those results of prior studies (9.5 and 12–13.01 kPa) [31, 32, 38]. The inconsistencies between this study and prior studies might be ascribed to the factors including the etiology of the liver disease, the unbalanced distribution of patients with various degrees of HF, as well as the BMI of study population. Compared with MRE, TE showed inferior ability in distinguishing each stage of HF with the exceptions in detecting ≥ F1. LSM-MRE also demonstrated a combination of higher sensitivity and specificity in detecting stage ≥ F2, ≥ F3, and F4 than LSM-TE.
In the study, IVIM showed moderate diagnostic performance in detecting fibrosis stages. In a comparative study, LSM-MRE showed superior diagnostic performance than Dt from IVIM model (AUC: 0.964 vs. 0.865 for ≥ F1, 0.965 vs. 0.875 for ≥ F2, 0.957 vs. 0.879 for ≥ F3 and 0.983 vs. 0.861 for F4) and demonstrated a combination of higher sensitivity and specificity in detecting stage ≥ F1, ≥ F2, ≥ F3, and F4 than Dt. In the study by Dyvorne et al. [33] for assessment of advanced fibrosis and cirrhosis, LSM-MRE showed superior diagnostic performance than Dt from IVIM model (AUC: 0.94 vs. 0.79), which was in agreement with our study. For the detection of fibrosis stages, although LSM-TE demonstrated higher AUC values than Dt (AUC: 0.921 vs. 0.865 for ≥ F1, 0.906 vs. 0.875 for ≥ F2, 0.913 vs. 0.879 for ≥ F3 and 0.931 vs. 0.861 for F4), there was no significant difference in their capability to distinguish HF stages except for detecting F4. The study by Dyvorne et al. [33] also showed the similar result. Thus, Dt showed comparable diagnostic performance to LSM-TE in detecting significant fibrosis and advanced fibrosis.
This study has several limitations. First, it is well known that HF usually accompanies varying degrees of inflammation and the degrees of inflammation is closely correlated with the progression and prognosis of HF, whereas we did not evaluate the influence of inflammatory activity grade on LSM-MRE, LSM-TE, and IVIM parameters in the staging of HF; further research is required to address this issue. Second, the perfusion-related diffusion coefficients (Dp) obtained from IVIM model might have been underestimated as very low b-values (0 < b < 50 s/mm2) were not selected in the study. Third, our study population comprised various chronic liver diseases from multiple etiologies because of the small sample size of each etiology except chronic hepatitis B. Fourth, for the specimens, we did not take hepatic steatosis into account during pathology analysis in the study. In addition, the influence of hepatic steatosis on the liver stiffness and IVIM parameters was not assessed. Although fat deposition might not affect the stiffness measurement, steatosis could cause inflammation, and thus increase liver stiffness even in the absence of liver fibrosis [16, 39, 40]. In the study by Sandrasegaran et al. [4] for assessment of hepatic steatosis in patients with chronic liver disease, IVIM parameters showed no significant association with the severity of hepatic steatosis. Fifth, the healthy volunteers were selected and assumed to be F0 and A0 without histologic findings as the reference standard. According to both previous studies [16, 41], we selected strict clinical and laboratory data which served as the reference standard. Finally, we selected the ROIs of MRE and IVIM in the largest cross section of the right lobe of the liver and used slice position with vessels and fissures as landmarks. We selected the ROIs of TE in the right lobe of the liver, but TE provides localized spot measurements at limited depth in the liver in areas where there is an acoustic window. Thus, the ROIs of MRE, IVIM, and TE could not match exactly.
In conclusion, TE and IVIM imaging are useful techniques and have a comparable performance for detecting significant fibrosis and advanced fibrosis, while MRE shows the best performance in distinguishing significant fibrosis, advanced fibrosis, and cirrhosis compared with both TE and IVIM and may have the potential for replacement of liver biopsy as a reference standard.
References
Wang Y, Ganger DR, Levitsky J, Sternick L A, McCarthy RJ, Chen Z E, et al. (2011) Assessment of chronic hepatitis and fibrosis: comparison of MR elastography and diffusion-weighted imaging. AJR Am J Roentgenol 196: 553-561. https://doi.org/10.2214/AJR.10.4580
Costa-Silva L, Ferolla S M, Lima A S, Vidigal P V T, Ferrari, T C de A (2018) MR elastography is effective for the non-invasive evaluation of fibrosis and necroinflammatory activity in patients with nonalcoholic fatty liver disease. Eur J Radiol 98:82-89. https://doi.org/10.1016/j.ejrad.2017.11.003
Yin M, Glaser KJ, Talwalkar JA, Chen J, Manduca A, Ehman RL (2016) Hepatic MR Elastography: Clinical Performance in a Series of 1377 Consecutive Examinations. Radiology 278: 114-124. https://doi.org/10.1148/radiol.2015142141
Sandrasegaran K, Paul Territo P, Elkady RM, Lin Y, Gasparis P, Borthakur G, et al.(2018) Does intravoxel incoherent motion reliably stage hepatic fibrosis, steatosis, and inflammation? Abdom Radiol (NY) 43:600-606. https://doi.org/10.1007/s00261-017-1263-8
Yoo H, Lee JM, Yoon JH, Lee DH, Chang W, Han JK (2016) Prospective Comparison of Liver Stiffness Measurements between Two Point Shear Wave Elastography Methods: Virtual Touch Quantification and Elastography Point Quantification. Korean J Radiol 17:750-757. https://doi.org/10.3348/kjr.2016.17.5.750
Bravo AA, Sheth SG, Chopra S (2001) Liver biopsy. N Engl J Med 344: 495-500. https://doi.org/10.1056/NEJM200102153440706
Huwart L, Sempoux C, Salameh N, Jamart J, Annet L, Sinkus R, et al. (2007) Liver fibrosis: noninvasive assessment with MR elastography versus aspartate aminotransferase-to-platelet ratio index. Radiology; 245: 458-466. https://doi.org/10.1148/radiol.2452061673
Venkatesh SK, Wang G, Lim SG, Wee A (2014) Magnetic resonance elastography for the detection and staging of liver fibrosis in chronic hepatitis B. Eur Radiol 24:70-78. https://doi.org/10.1007/s00330-013-2978-8
Lee JE, Lee JM, Lee KB, Yoon JH, Shin CI, Han JK, et al. (2014) Noninvasive assessment of hepatic fibrosis in patients with chronic hepatitis B viral infection using magnetic resonance elastography. Korean J Radiol 15:210-217. https://doi.org/10.3348/kjr.2014.15.2.210
Rustogi R, Horowitz J, Harmath C, Wang Y, Chalian H, Ganger D R, et al. (2012) Accuracy of MR elastography and anatomic MR imaging features in the diagnosis of severe hepatic fibrosis and cirrhosis. J Magn Reson Imaging 35: 1356-1364. https://doi.org/10.1002/jmri.23585
Shi Y, Guo QY, Xia F, Dzyubak B, Glaser K J, Li Q J, et al. (2014) MR Elastography for the Assessment of Hepatic Fibrosis in Patients with Chronic Hepatitis B Infection: Does Histologic Necroinflammation Influence the Measurement of Hepatic Stiffness? Radiology 273:88-98. https://doi.org/10.1148/radiol.14132592
Yin M, Talwalkar JA, Glaser KJ, Manduca A, Grimm R C, Rossman P J, et al. (2007) Assessment of hepatic fibrosis with magnetic resonance elastography. Clin Gastroenterol Hepatol 5: 1207-1213. https://doi.org/10.1016/j.cgh.2007.06.012
Ichikawa S, Motosugi U, Ichikawa T, Sano K, Morisaka H, Enomoto N, et al. (2012) Magnetic resonance elastography for staging liver fibrosis in chronic hepatitis C. Magn Reson Med Sci 11:291-297. https://doi.org/10.2463/mrms.11.291
Yoon JH, Lee JM, Joo I, Lee ES, Sohn JY, Jang SK, et al. (2014) Hepatic Fibrosis: Prospective Comparison of MR Elastography and US Shear-Wave Elastography for Evaluation. Radiology 273:772-782. https://doi.org/10.1148/radiol.14132000
Nedredal GI, Yin M, McKenzie T, Lillegard J, Luebke-Wheeler J, Talwalkar J, et al. (2011) Portal hypertension correlates with splenic stiffness as measured with MR elastography. J Magn Reson Imaging 34:79-87. https://doi.org/10.1002/jmri.22610
Ichikawa S, Motosugi U, Morisaka H, Sano K, Ichikawa T, Enomoto N, et al. (2015) MRI-Based Staging of Hepatic Fibrosis: Comparison of Intravoxel Incoherent Motion Diffusion-Weighted Imaging with Magnetic Resonance Elastography. J Magn Reson Imaging 42:204-210. https://doi.org/10.1002/jmri.24760
Le Bihan D, Breton E, Lallemand D, Grenier P, Cabanis E, Laval-Jeantet M (1986) MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology 161: 401-407. https://doi.org/10.1148/radiology.161.2.3763909
Le Bihan D, Breton E, Lallemand D, Aubin ML, Vignaud J, Laval-Jeantet M (1988) Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology; 168:497-505. https://doi.org/10.1148/radiology.168.2.3393671
Seo N, Chung YE, Park YN, Kim E, Hwang J,Kim MJ (2018) Liver fibrosis: stretched exponential model outperforms mono-exponential and bi-exponential models of diffusion-weighted MRI. Eur Radiol 28 :1-11. https://doi.org/10.1007/s00330-017-5292-z
Franca M, Marti-Bonmati L, Alberich-Bayarri A, Oliveira P, Guimaraes S, Oliveira J, et al. (2017) Evaluation of fibrosis and inflammation in diffuse liver diseases using intravoxel incoherent motion diffusion-weighted MR imaging. Abdom Radiol (NY) 42(2):468-477. https://doi.org/10.1007/s00261-016-0899-0
Luciani A, Vignaud A, Cavet M, Nhieu JTV, Mallat A, Ruel L, et al. (2008) Liver cirrhosis: intravoxel incoherent motion MR imaging-pilot study. Radiology 249: 891-899. https://doi.org/10.1148/radiol.2493080080
Chung SR, Lee SS, Kim N, Yu ES, Kim E, Kühn B, et al. (2015) Intravoxel incoherent motion MRI for liver fibrosis assessment: a pilot study. Acta Radiol 56: 1428-1436. https://doi.org/10.1177/0284185114559763
Yoon JH, Lee JM, Baek JH, Shin C, Kiefer B, Han JK, et al. (2014) Evaluation of hepatic fibrosis using intravoxel incoherent motion in diffusion-weighted liver MRI. J Comput Assist Tomogr 38: 110-116. https://doi.org/10.1097/rct.0b013e3182a589be
Myers RP, Elkashab M, Ma M, Crotty P, Pomier-Layrargues G (2010) Transient elastography for the noninvasive assessment of liver fibrosis: A multicentre Canadian study. Can J Gastroenterol 24:661-670. http://dx.doi.org/10.1155/2010/153986
Sandrin L, Fourquet B, Hasquenoph JM, Yon S, Fournier C, Mal F, et al. (2003) Transient elastography: a new non-invasive method for assessment of hepatic fibrosis. Ultrasound Med Biol; 29: 1705-1713. https://doi.org/10.1016/j.ultrasmedbio.2003.07.001
Ogawa E, Furusyo N, Toyoda K, Takeoka H, Otaguro S, Hamada M, et al. (2007) Transient elastography for patients with chronic hepatitis B and C virus infection: Non-invasive, quantitative assessment of liver fibrosis. Hepatol Res 37: 1002-1010. https://doi.org/10.1111/j.1872-034X.2007.00160.x
Sporea I, Bota S, Gradinaru-Taşcău O, Sirli R, Popescu A, Jurchiş A. (2014) Which are the cut-off values of 2D-Shear Wave Elastography (2D-SWE) liver stiffness measurements predicting different stages of liver fibrosis, considering Transient Elastography (TE) as the reference method? Eur J Radiol 83: e118-e122. https://doi.org/10.1016/j.ejrad.2013.12.011
Rockey DC. (2008) Noninvasive Assessment of Liver Fibrosis and Portal Hypertension with Transient Elastography. Gastroenterology 134: 8-14. https://doi.org/10.1053/j.gastro.2007.11.053
Foucher J, Chanteloup E, Vergniol J, Castéra L, Le Bail B, Adhoute X, et al. (2006) Diagnosis of cirrhosis by transient elastography (FibroScan): a prospective study. Digest of the World Core Medical Journal 55: 403-408. https://doi.org/10.1136/gut.2005.069153
Lucidarme D, Foucher J, Le Bail B, Vergniol J, Castera L, Duburque C, et al. (2009) Factors of accuracy of transient elastography (fibroscan) for the diagnosis of liver fibrosis in chronic hepatitis C. Hepatology 49: 1083-1089. https://doi.org/10.1002/hep.22748
Friedrich-Rust M, Ong MF, Martens S, Sarrazin C, Bojunga J, Zeuzem S, et al. (2008) Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterol 134: 960-974. https://doi.org/10.1053/j.gastro.2008.01.034
Tang A, Cloutier G, Szeverenyi NM, Sirlin CB (2015) Ultrasound elastography and MR elastography for assessing liver fibrosis: part 2, diagnostic performance, confounders, and future directions. AJR Am J Roentgenol 205:33-40. https://doi.org/10.2214/ajr.15.14553
Dyvorne HA, Jajamovich GH, Bane O, Fiel MI, Chou H, Schiano TD, et al. (2016) Prospective comparison of magnetic resonance imaging to transient elastography and serum markers for liver fibrosis detection. Liver Int. 36: 659-666. https://doi.org/10.1111/liv.13058.
Bohte AE, de Niet A, Jansen L, Bipat S, Nederveen AJ, Verheij J, et al (2014) Non-invasive evaluation of liver fibrosis: a comparison of ultrasound-based transient elastography and MR elastography in patients with viral hepatitis B and C. Eur Radiol 24:638-648. https://doi.org/10.1007/s00330-013-3046-0
Bedossa P, Poynard T (1996) An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology 24:289-293. https://doi.org/10.1053/jhep.1996.v24.pm0008690394
Dyvorne HA, Galea N, Nevers T, Fiel M I, Carpenter D, Wong E, et al. (2013) Diffusion-weighted imaging of the liver with multiple b values: effect of diffusion gradient polarity and breathing acquisition on image quality and intravoxel incoherent motion parameters-a pilot study. Radiology 266: 920-929. https://doi.org/10.1148/radiol.12120686
The Polaris Observatory Collaborators (2018) Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study. Lancet Gastroenterol Hepatol 3:383-403. https://doi.org/10.1016/S2468-1253(18)30056-6
Tsochatzis EA, Gurusamy KS, Ntaoula S, Cholongitas E (2011) Davidson BR, Burroughs AK. Elastography for the diagnosis of severity of fibrosis in chronic liver disease: a meta-analysis of diagnostic accuracy. J Hepatol 54: 650- 659. https://doi.org/10.1016/j.jhep.2010.07.033
Chen J, Talwalkar JA, Yin M, Glaser KJ, Sanderson SO, Ehman RL (2011). Early detection of nonalcoholic steatohepatitis in patients with nonalcoholic fatty liver disease by using MR elastography. Radiology 259: 749-756. https://doi.org/10.1148/radiol.11101942
Motosugi U, Ichikawa T, Niitsuma Y, Araki T (2011). Acoustic radiation force impulse elastography of the liver: can fat deposition in the liver affect the measurement of liver stiffness? Jpn J Radiol 29:639-643. https://doi.org/10.1007/s11604-011-0607-5
Watanabe H, Kanematsu M, Goshima S, Kondo H, Onozuka M, Moriyama N, et al. (2011) Staging hepatic fibrosis: comparison of gadoxetate disodium-enhanced and diffusion-weighted MR imaging-preliminary observations. Radiology 259: 142-150. https://doi.org/10.1148/radiol.10100621
Acknowledgements
This work was supported by the National Key R&D Program of China (2017YFE0103600), National Natural Science Foundation of China (81720108021, 81772009, 81601466, 81641168, 31470047), and Scientific and Technological Research Project of Henan Province (182102310162).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fu, F., Li, X., Chen, C. et al. Non-invasive assessment of hepatic fibrosis: comparison of MR elastography to transient elastography and intravoxel incoherent motion diffusion-weighted MRI. Abdom Radiol 45, 73–82 (2020). https://doi.org/10.1007/s00261-019-02140-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02140-x