Abstract
Purpose
Hereditary hemorrhagic telangiectasia (HHT) is an autosomal dominant multi-organ vascular disorder that commonly affects the gastrointestinal tract and the liver resulting in telangiectasias and arteriovenous malformations (AVMs). Previous studies looking at the prevalence of liver and abdominal organ involvement in HHT have been limited by differing imaging techniques and sample size limitations. We sought to define the prevalence of HHT related abdominal vascular abnormalities using optimized multiphasic contrast-enhanced abdominal computed tomography (CT) exams in a large cohort of HHT patients.
Methods
Between January 2001 and May 2015; we identified a total of 333 consecutive HHT patients who had undergone a dedicated HHT protocol multiphase abdominal CT at our institution. The CT exams were reviewed by three board certified abdominal radiologists for the presence of vascular abnormalities involving the liver, pancreas, spleen, and other abdominal organs. Vascular abnormalities involving the liver were further categorized as telangiectasias, large confluent vascular masses, perfusion abnormalities, or hepatic shunts.
Results
In patients with abdominal vascular abnormalities, the liver was the most commonly involved organ, with 180 out of 333 (54.1%) patients demonstrating at least one hepatic vascular abnormality (telangiectasia, confluent vascular mass, transient perfusion abnormalities, and hepatic shunts), with most (70.0%) demonstrating multiple hepatic vascular abnormalities. The other most common organs involved included the pancreas (18.0%), spleen (6.3%), and small bowel (4.5%).
Conclusion
In patients with the clinical diagnosis of HHT, greater than half demonstrate an abdominal vascular abnormality, with the most commonly involved organ being the liver. These may be under recognized on routine or single phase contrast-enhanced CT of the abdomen. This supports the use of optimized multiphasic abdominal CT exams as an important tool for the evaluation and screening of patients with HHT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hereditary hemorrhagic telangiectasia (HHT), also known as Osler-Weber-Rendu disease, is an autosomal dominant inherited disorder with an estimated prevalence of 1–2 individuals per 10,000 [1, 2]. It is characterized by vascular abnormalities consisting of dilated, disorganized venules, with direct connection to arterioles (a.k.a. arteriovenous malformations or telangiectasias) [3]. The disease affects multiple organs and vascular beds throughout the body, with the skin, mucous membranes, lungs, central nervous system, gastrointestinal tract and liver among the most common sites of involvement [4, 5]. Many patients can be asymptomatic. When clinical manifestations do occur, they present as hemorrhage (epistaxis, GI bleeding, intracranial hemorrhage etc.) or by abnormal arteriovenous shunting resulting in high-output cardiac failure (due to liver arteriovenous shunting), systemic embolization resulting in stroke and cerebral abscesses, or hypoxemia due to pulmonary arterial shunting [6].
Clinical diagnosis of HHT is made via the Curacao criteria. The four criteria are: (1) spontaneous and recurrent epistaxis, (2) characteristic mucocutaneous telangiectasias (lips, oral cavity face and fingers), (3) visceral (brain, lung, liver, bowel) arteriovenous malformations (AVM), and (4) diagnosis of HHT in a first degree relative utilizing these same Curacao criteria [7]. Patients with ≥ 3 criteria are labeled as “definite HHT” while those with 2 of the 4 criteria are labeled as “possible” or “suspected” HHT [8].
It is important to recognize that liver and visceral AVMs often go unrecognized until a complication occurs. In a previous study; only 8% of HHT patients with hepatic vascular abnormalities were symptomatic and thus, hepatic involvement can often go unrecognized until late in the disease course [9]. This is also likely compounded by the fact that single phase contrast-enhanced computed tomography (CT) often poorly delineates hepatic and other organ involvement due to the fact that many vascular abnormalities are best seen (or only seen) during the early arterial phase. This early arterial phase is often not a part of the imaging protocol in most single and even multiphasic exams [6]. To provide an accurate estimate of the liver involvement, we performed this study to describe the prevalence of hepatic and other abdominal vascular abnormalities identified on an optimized contrast-enhanced multiphasic CT in patients clinically diagnosed with definite HHT.
Methods
Patient population
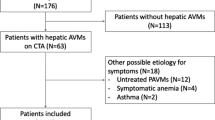
This study was approved by our center’s Institutional Review Board (IRB). We undertook a retrospective review of our database of all HHT patients seen at our center from January 2001 to May 2015. The database was compiled by searching our electronic medical record for the terms HHT, hereditary hemorrhagic telangiectasia, Osler-Weber-Rendu, or Rendu-Osler-Weber. Additionally, patients were searched for International Classification of Diseases-9 code of 448.0 in their chart, corresponding to HHT. Individual charts were reviewed and only patients with definite HHT based on the Curacao criteria, as described above, were included in the study. Of note, the study includes patients who were formally diagnosed with HHT both before and after our imaging study. Imaging studies were then reviewed, and only patients who had undergone a contrast-enhanced optimized multiphasic CT of the abdomen per our institution’s HHT protocol were included in the final dataset. These studies are obtained for multiple reasons, including assessment of vascular abnormalities to diagnose HHT or the presence of organ involvement and certain risk factors (such as large shunts) in patients with previously diagnosed HHT.
Imaging evaluation
Images were obtained with the patient in the supine position from the top of the liver to the iliac crest. Three phases were obtained in each patient, described as early arterial, late arterial, and portal venous phases. The goal of the early arterial phase is to have hepatic arterial enhancement without enhancement of the portal and hepatic veins, which can limit evaluation of hepatic shunting. In the current iteration of this protocol, a region of interest (ROI) is drawn in the descending aorta just above the scan field, and scanning is initiated for the early arterial phase as soon as possible after this ROI has reached 150 Hounsfield Units (HU). This early arterial phase acquisition typically occurred around 15–20 s after initiation of contrast injection. Late arterial and portal venous phase images are then obtained 20 s and 40 s, respectively, following the early arterial phase acquisition. Contrast volume, injection rate, and concentration varies based on the patients weight, though ranges between 100 and 200 mL, injected between 4 and 5 mL/s, with concentrations of 300–350 mg/mL of Iodine. Given that many patients undergo CT scans of the chest at the same time as the abdomen, it is important to point out our approach to accomplishing both. As arteriovenous malformations within the lungs are well seen without the use of intravenous (IV) contrast, these exams are typically performed without contrast. This allows contrast bolus timing to be focused on the liver to optimize the early arterial phase and minimize contrast within the hepatic and portal veins.
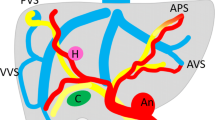
Exams were reviewed and reinterpreted by three board certified abdominal radiologists. Hepatic lesions were subcategorized into four groups: Telangiectasias, large confluent vascular masses, hepatic perfusion abnormalities, and hepatic shunts according to standard nomenclature. Telangiectasias were defined as typically round, 9 mm or less, arterial hyperenhancing foci which are due to a direct communication between arterioles and postcapillary venules [10]. Typically these are most conspicuous in the early arterial phase and are often subtle or imperceptible in the portal venous phase [6, 11]. Large confluent vascular masses appear similar to telangiectasias, but are defined as ≥ 10 mm in diameter [12]. Because of their larger size, these lesions can sometimes remain visible into the portal venous phase. Of note, large confluent vascular masses are usually homogeneously enhancing, in contrast to the more peripheral, nodular early enhancement of cavernous hemangiomas. While telangiectasias and large confluent vascular masses are focal lesions, hepatic perfusion abnormalities are defined as a non-focal heterogeneous enhancement pattern of the liver parenchyma. As with other hepatic vascular findings, this finding is typically best seen during the early and late arterial phases, with a normal enhancement pattern often seen in the portal venous phase [6]. Examples of telangiectasias, confluent vascular masses, and a perfusion abnormality are demonstrated in Fig. 1. The final group of abnormalities characterized was hepatic shunts, which included arteriovenous, arterioportal, and portovenous shunts. Arteriovenous and arterioportal shunts are defined as shunts between the hepatic artery and hepatic veins or portal veins, respectively. These are best seen during the early arterial phase and are identified by the premature/early enhancement of the hepatic vein (arteriovenous shunting) or portal vein (arterioportal shunting). Only the early arterial phase is utilized to identify these shunts, because opacification/enhancement of the portal and hepatic veins normally occur during the later (late arterial and portal venous) phases of contrast administration. Care must be taken to not confuse suboptimal contrast timing or contrast refluxing into the hepatic veins from the IVC as an abnormal shunt. An example of an arterioportal shunt is demonstrated in Fig. 1 and an example of arteriovenous shunting is demonstrated in Fig. 2. Portovenous shunts are abnormal shunts between the portal veins and hepatic veins. These are much less common and are best seen during the portal venous phase, with a dilated portal vein communicating with a hepatic vein. An example of a portovenous shunt is demonstrated in Fig. 3.
Arterial phase images of the liver in a patient with HHT. This patient has multiple hepatic vascular abnormalities. There is a dilated, tortuous left hepatic artery with early filling of an adjacent portal vein, consistent with arterioportal shunting (black arrow). There are also multiple telangiectasias (white arrow), confluent vascular masses (white arrow head), and a perfusion abnormality (black arrowhead)
Arterial phase images of the liver in a patient with HHT and high-output cardiac failure. a There are numerous significantly enlarged hepatic artery braches denoted by the black arrowheads. b Early filling of the hepatic veins is seen, denoted by the black arrows. Overall, findings are consistent with extensive arteriovenous shunting
Abnormal vascular lesions in other abdominal organs such as the pancreas, small bowel, spleen, stomach, and colon were also noted and recorded. These lesions were grouped by organ for the purpose of this study. For instance, both splenic artery aneurysms and splenic parenchymal vascular abnormalities were labeled splenic vascular lesions and lesions within the duodenum, jejunum, and ileum were all labeled as small bowel vascular lesions. Examples of pancreatic, adrenal, small bowel, and splenic vascular abnormalities are demonstrated in Figs. 4, 5, 6, and 7, respectively. Of note, the HHT CT protocol only covers the abdomen to the level of the iliac crests, often excluding portions of the small bowel and colon, in particular the cecum.
Portal venous phase images in a patient with HHT. Numerous foci of hyperenhancement were seen within the jejunum, including the small lesion denoted by the black arrow. Findings are consistent with small vascular malformations and were subsequently confirmed and treated with double-balloon enteroscopy
Statistical analysis
Statistical analysis to evaluate for a significant difference in the prevalence of abdominal vascular abnormalities based on the gender of the patient was performed using the Chi squared test. Genetic mutation information was collected (if available), and the Chi squared test was used to analyze any differences in the prevalence of hepatic vascular malformations in patients with ENG and ACVRL1 mutations. Additionally, analysis was performed to evaluate for a significant difference based on the patient’s age by using the Student’s t test.
Results
Patient population
333 patients with definite HHT based on the Curacao criteria were included in the study. The mean patient age was 53.7 years, with a standard deviation of 16.2 years and a range of 20–93 years. The majority of patients were female (n = 200, 60.1%). Epistaxis was the most common manifestation of HHT in our population with 303 patients (91.0%). This was followed by mucocutaneous telangiectasia in 299 (89.8%), family history in 292 (87.7%), and visceral AVM in 288 (86.5%). These findings are summarized in Table 1.
Prevalence of vascular abnormality by organ
The liver was by far the most commonly affected abdominal organ, with 180 patients (54.1%) demonstrating at least one hepatic vascular abnormality. Pancreatic vascular malformations were seen in 60 patients (18.0%). Pancreatic manifestations most commonly involved a singled dilated vessel. Twenty-one patients (6.3%) had either a splenic artery aneurysm or a vascular malformation within the spleen itself. Duodenal, jejunal, and ileal vascular abnormalities were grouped into a single category; in which 15 patients (4.5%) demonstrated at least one abnormality. Six patients (1.8%) had a vascular abnormality within the visualized colon. Finally, five patients (1.5%) were found to have gastric vascular abnormalities and four patients (1.2%) were found to have adrenal vascular abnormalities. These findings are summarized in Table 2.
Hepatic vascular abnormalities
Telangiectasias were the most common hepatic vascular abnormality, present in 165 (49.5%) of the patients. Large confluent vascular masses, perfusion abnormalities, and hepatic shunts were all found in lesser but similar numbers. Large confluent masses were seen in 76 (22.8%), perfusion abnormalities were seen in 77 (23.1%), and hepatic shunts were seen in 68 (20.4%). These findings are summarized in Table 3.
Only 54 patients (16.2%) were found to have a single type of hepatic vascular abnormality, while 132 patients (40.0%) had at least two types of hepatic vascular abnormalities. The most common combination of types was telangiectasia and perfusion abnormality, which was found in 27 (8.1%) of patients. As would be expected, the various combinations which included telangiectasias were more common than combinations without telangiectasias. These findings are summarized in Table 4.
Clinical variables associated with abdominal vascular abnormalities
A total of 184 patients demonstrated at least one abdominal vascular abnormality, while 149 patients did not. The mean age for those who had an abdominal vascular abnormality was 55.3 years (SD = 15.6 years), while the mean age in those negative for abdominal vascular abnormalities was 51.7 (SD = 16.8 years). This difference in prevalence based on age was statistically significant with a p-value of 0.04.
Women had a higher likelihood of having abdominal vascular abnormalities, with 117 out of 200 women (58.5%) and 67 out of 133 men (50.4%) having positive abdominal findings. However, these findings were not statistically significant, with a p-value of 0.18. These findings are summarized in Table 5.
Of the 333 patients, 102 had documented HHT genetic mutations. Fifty-six (16.8%) had an ENG mutation, as is seen in HHT1, and 46 (13.8%) had an ACVRL1 mutation, as is seen in HHT2. The prevalence of hepatic vascular abnormalities was 55.3% (31/56) in patients with ENG mutations and 67.4% (31/46) in patients with ACVRL1 mutations. While a higher percentage of patients with ACVRL1 mutations had hepatic vascular abnormalities, the results were not statistically significant, with a p-value of 0.30. These findings are summarized in Table 6.
Discussion
The prevalence of abdominal vascular abnormalities in patients with HHT is important information, as it helps us understand the extent of manifestations in HHT. Our study is particularly pertinent for assessment of organs such as the liver, where imaging studies are the only way to assess involvement and an HHT specific protocol is important for complete evaluation. Our study of 333 patients with a diagnosis of definite HHT found the prevalence of abdominal vascular abnormalities at 55.3%, with hepatic vascular abnormalities the most common abdominal manifestation. This is the largest series evaluating HHT abdominal findings to our knowledge. Remote studies estimated hepatic involvement in the range of 8–31% [13, 14]. However, these numbers were likely underestimated, as the CT technology required to visualize the often subtle hepatic findings was not available at the time. Later studies utilizing multidetector row CT demonstrated similar hepatic vascular malformation prevalence as our study [11, 15].
Several studies have examined the prevalence of vascular malformations within the bowel, primarily with endoscopy and capsule endoscopy. Various studies have shown gastric involvement ranging from 29 to 75% of patients and small intestinal involvement ranging from 56 to 91% of patients [16,17,18,19]. Our study, based on CT imaging, demonstrated much lower prevalence in both areas. The likely explanation for the discrepancy between our studies is the imaging modality. While CT is optimal for evaluation of the liver and can visualize larger vascular malformations in other organs such as the bowel, endoscopy is almost assuredly going to detect a higher percentage of small, mucosal lesions that these patients often have. In addition, the bowel was not completely included in our imaging, and dedicated bowel imaging, such as with triple-phase enterography, would likely help in detecting bowel lesions. This likely resulted in an underreporting of bowel vascular malformations in our study.
Similarly, prior studies investigating the prevalence of vascular abnormalities within the colon have primarily used colonoscopy. Colon involvement has again been reported as higher than in our study, with studies reporting a prevalence of 10–32% [20, 21]. This discrepancy again likely has to do with the imaging modality, similar to the small intestine. Also contributing to this discrepancy is the fact that our studies did not include a large portion of the colon, as only the abdomen to the level of the iliac crests was acquired. This precludes assessment of a large portion of the colon, including the cecum and sigmoid colon.
This study did not examine the relationship between abdominal vascular findings and associated symptoms and co-morbidities. Many of the patients evaluated showed only minimal abdominal involvement, such as a few small telangiectasias within the liver. In patients with only minimal involvement, it is unlikely that any significant symptoms or complications would be present. In fact, Garcia-Tsao et al. reported only 8% of patients with HHT and hepatic vascular malformations on imaging exhibited symptoms [9]. While symptoms may be rare, they can certainly be serious; with potential complications associated with hepatic vascular malformations including high-output cardiac failure, portal hypertension, and biliary necrosis. A potential avenue of further investigation involving our cohort would be to examine the prevalence of HHT symptoms and complications and how they relate to the severity of abdominal manifestations.
Limitations
Our study has limitations. All of the patients reviewed had definite HHT, meaning the reviewers were not blinded to the patient’s diagnosis. This could lead to some bias in reporting. It is likely that many patients presented to our institution after being diagnosed with HHT due to either symptoms being present or findings identified on prior imaging or procedural studies. This may cause an overestimation of abdominal findings in our study. Additionally, the presence of AVMs is a criterion used for diagnosis of HHT within the Curacao criteria. This could be a confounding factor due to all of our patients having a diagnosis of definite HHT based on the Curacao criteria, potentially leading to elevated prevalence of AVMs in our cohort.
This study evaluates imaging exams over the course of 15 years, in which various CT scanners with different levels of technology were used. Another limitation of our study relates to suboptimal image acquisition, particularly of early arterial and late arterial phases. While the protocol used is specifically designed for assessment of HHT manifestations, there are times when either the contrast bolus timing is suboptimal or reflux of contrast from the IVC opacifies the hepatic veins, limiting the assessment of hepatic shunting. While these may lead to underreporting of abdominal manifestations in some situations, it is often unavoidable due to the range of physiologic conditions encountered. Since these CT exams typically did not cover the pelvis, portions of the small bowel and colon as well as the bladder, uterus and adnexa, prostate gland, and seminal vesicles were not covered.
Conclusion
In patients with the clinical diagnosis of HHT, greater than half demonstrate an abdominal vascular abnormality, with the most commonly involved organ being the liver. These may be under recognized on routine or single phase contrast-enhanced CT of the abdomen. This supports the use of optimized multiphasic abdominal CT exams as an important tool for the evaluation and screening of patients with HHT.
References
Dakeishi M, Shioya T, Wada Y, Shindo T, Otaka K, Manabe M, Nozaki J, Inoue S, Koizumi A (2002) Genetic epidemiology of hereditary hemorrhagic telangiectasia in a local community in the northern part of Japan. Hum Mutat 19 (2):140-148. https://doi.org/10.1002/humu.10026
Kjeldsen AD, Vase P, Green A (2000) [Hereditary hemorrhagic telangiectasia. A population-based study on prevalence and mortality among Danish HHT patients]. Ugeskr Laeger 162 (25):3597-3601
Guttmacher AE, Marchuk DA, White RI, Jr. (1995) Hereditary hemorrhagic telangiectasia. N Engl J Med 333 (14):918-924. https://doi.org/10.1056/NEJM199510053331407
Peery WH (1987) Clinical spectrum of hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease). Am J Med 82 (5):989-997
Brinjikji W, Nasr DM, Wood CP, Iyer VN (2017) Pulmonary Arteriovenous Malformations Are Associated with Silent Brain Infarcts in Hereditary Hemorrhagic Telangiectasia Patients. Cerebrovasc Dis 44 (3-4):179-185. https://doi.org/10.1159/000478734
Siddiki H, Doherty MG, Fletcher JG, Stanson AW, Vrtiska TJ, Hough DM, Fidler JL, McCollough CH, Swanson KL (2008) Abdominal findings in hereditary hemorrhagic telangiectasia: pictorial essay on 2D and 3D findings with isotropic multiphase CT. Radiographics 28 (1):171-184. https://doi.org/10.1148/rg.281075037
Shovlin CL, Guttmacher AE, Buscarini E, Faughnan ME, Hyland RH, Westermann CJ, Kjeldsen AD, Plauchu H (2000) Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am J Med Genet 91 (1):66-67
McDonald J, Wooderchak-Donahue W, VanSant Webb C, Whitehead K, Stevenson DA, Bayrak-Toydemir P (2015) Hereditary hemorrhagic telangiectasia: genetics and molecular diagnostics in a new era. Front Genet 6:1. https://doi.org/10.3389/fgene.2015.00001
Garcia-Tsao G (2007) Liver involvement in hereditary hemorrhagic telangiectasia (HHT). J Hepatol 46 (3):499-507. https://doi.org/10.1016/j.jhep.2006.12.008
Buscarini E, Gandolfi S, Alicante S, Londoni C, Manfredi G (2018) Liver involvement in hereditary hemorrhagic telangiectasia. Abdom Radiol (NY). https://doi.org/10.1007/s00261-018-1671-4
Ravard G, Soyer P, Boudiaf M, Terem C, Abitbol M, Yeh JF, Brouard R, Hamzi L, Rymer R (2004) Hepatic involvement in hereditary hemorrhagic telangiectasia: helical computed tomography features in 24 consecutive patients. J Comput Assist Tomogr 28 (4):488-495
Memeo M, Stabile Ianora AA, Scardapane A, Buonamico P, Sabba C, Angelelli G (2004) Hepatic involvement in hereditary hemorrhagic telangiectasia: CT findings. Abdom Imaging 29 (2):211-220. https://doi.org/10.1007/s00261-003-0101-3
Plauchu H, de Chadarevian JP, Bideau A, Robert JM (1989) Age-related clinical profile of hereditary hemorrhagic telangiectasia in an epidemiologically recruited population. Am J Med Genet 32 (3):291-297. https://doi.org/10.1002/ajmg.1320320302
Reilly PJ, Nostrant TT (1984) Clinical manifestations of hereditary hemorrhagic telangiectasia. Am J Gastroenterol 79 (5):363-367
Barral M, Sirol M, Place V, Hamzi L, Borsik M, Gayat E, Boudiaf M, Soyer P (2012) Hepatic and pancreatic involvement in hereditary hemorrhagic telangiectasia: quantitative and qualitative evaluation with 64-section CT in asymptomatic adult patients. Eur Radiol 22 (1):161-170. https://doi.org/10.1007/s00330-011-2243-y
Canzonieri C, Centenara L, Ornati F, Pagella F, Matti E, Alvisi C, Danesino C, Perego M, Olivieri C (2014) Endoscopic evaluation of gastrointestinal tract in patients with hereditary hemorrhagic telangiectasia and correlation with their genotypes. Genet Med 16 (1):3-10. https://doi.org/10.1038/gim.2013.62
Chamberlain SM, Patel J, Carter Balart J, Gossage JR, Jr., Sridhar S (2007) Evaluation of patients with hereditary hemorrhagic telangiectasia with video capsule endoscopy: a single-center prospective study. Endoscopy 39 (6):516-520. https://doi.org/10.1055/s-2007-966349
Greve E, Moussata D, Gaudin JL, Lapalus MG, Giraud S, Dupuis-Girod S, Calender A, Plauchu H, Saurin JC (2010) High diagnostic and clinical impact of small-bowel capsule endoscopy in patients with hereditary hemorrhagic telangiectasia with overt digestive bleeding and/or severe anemia. Gastrointest Endosc 71 (4):760-767. https://doi.org/10.1016/j.gie.2009.11.004
Ingrosso M, Sabba C, Pisani A, Principi M, Gallitelli M, Cirulli A, Francavilla A (2004) Evidence of small-bowel involvement in hereditary hemorrhagic telangiectasia: a capsule-endoscopic study. Endoscopy 36 (12):1074-1079. https://doi.org/10.1055/s-2004-826045
Longacre AV, Gross CP, Gallitelli M, Henderson KJ, White RI, Jr., Proctor DD (2003) Diagnosis and management of gastrointestinal bleeding in patients with hereditary hemorrhagic telangiectasia. Am J Gastroenterol 98 (1):59-65. https://doi.org/10.1111/j.1572-0241.2003.07185.x
Proctor DD, Henderson KJ, Dziura JD, Longacre AV, White RI, Jr. (2005) Enteroscopic evaluation of the gastrointestinal tract in symptomatic patients with hereditary hemorrhagic telangiectasia. J Clin Gastroenterol 39 (2):115-119
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Welle, C.L., Welch, B.T., Brinjikji, W. et al. Abdominal manifestations of hereditary hemorrhagic telangiectasia: a series of 333 patients over 15 years. Abdom Radiol 44, 2384–2391 (2019). https://doi.org/10.1007/s00261-019-01976-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-01976-7